Developing a Therapy Bed Assessment Tool
advertisement

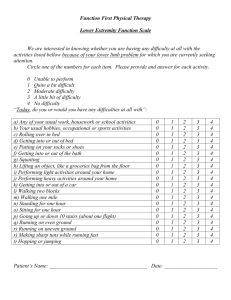
C L I N I C A L P R A C T I C E Developing a Therapy Bed Assessment Tool BY Kathryn Kozell Kathryn Kozell, RN, BA, BScN, MScN, ACNP/ET, is an Acute Care Nurse Practitioner/ Clinical Nurse Specialist in surgery at St. Joseph’s Health Care London in Ontario. She has been an Enterostomal Therapy Nurse since 1981. She is also a member of the CAET and CAWC. 12 Wo u n d C a re C a n a d a T herapeutic mattresses and bed frames are Therapy Bed Task Force designed to provide either pressure reduc- Our facility established the Therapy Bed Task Force, a tion or pressure relief in situations where nursing initiative that was composed of various clinicians skin integrity or other physiological systems are in representing the intensive care unit, orthopedics, family jeopardy of potential or actual injury. One of the greatest medicine and palliative care, as well as an acute care challenges for the clinician is to select the most appropri- nurse practitioner/clinical nurse specialist/enterostomal ate product for a patient’s specific individual demands. therapy nurse in surgery, a purchasing representative The experience of St. Joseph’s Health Care London, in from materials management, and a territory sales man- identifying the multiple risk needs of patients, institu- ager from the contracted company from which the ther- tional requirements and using an interdisciplinary team apy beds were being rented. The mandate of this team approach for developing a therapy bed assessment tool was threefold: 1. investigate and identify the pattern may serve as a useful model for other facilities. of therapy bed utilization within the health centre; There is a heightened awareness among health-care 2. develop and implement a system that would monitor professionals to seek out the best possible products and provide consistent and effective therapy bed that will provide the most efficient and effective thera- utilization; and 3. control the financial allowance peutic response. This has been well demonstrated with dedicated to therapy bed rental. the vast selection of wound-care products available to Doughty, Fairchild and Stogis2 referred to a three-phase meet the specificity of any wound. In the treatment of decisional approach regarding the use of replacement pressure-related skin injuries, specialty beds, perhaps mattresses. Using this approach in a slightly modified surprisingly, are not a new supportive device. In A process, our team concluded it was important to Historical Perspective on Specialty Beds and Other determine the following: Apparatus for Treatment of Invalids1 a medical report 1. who was using the therapy bed from way back in 1585 cites the “successful use of a 2. what the selection criteria were down cushion in concert with a program of nutrition, 3. what therapy bed would then be selected for hygiene, and pain relief for a pressure ulcer.” In today’s implementation world of therapeutic mattresses, manufacturers have responded with many therapeutic pressure devices; Results of the Task Force however, the decision-making process leading to the The Task Force identified that there were high-demand appropriate selection of the right mattress for the right therapy bed units (the intensive care unit, orthopedics patient can be as challenging as the presentation of and family medicine/palliative care) and low-demand any wound. therapy bed units (general medicine, general surgery— Vo l u m e 2 , N u m b e r 2 TABLE 1 Clinical Diagnoses/Characteristics patterns. This was accomplished by References combining patient characteristics within 1. Levine JM. A historical perspective on specialty beds and other apparatus for treatment of invalids. Advances in Wound Care. 1994;7(5):51-54. each of the high- and low-demand Medical Surgical Critical Care Dermatitis Flaps, grafts Hemodynamically unstable found in the Braden Scale for Predicting Oncology Draining wounds Comatose health pattern category now had three Paralysis Sepsis Positional intolerance to four descriptors, which described a Multiple ulcers Multiple ulcers Sepsis functional health demands to very Multiple fractures secondary to pathology Multiple bone fractures Large abdominal wounds complex functional health demands). units with the clinical descriptors as Pressure Sore Risk.4 Each functional range of health demands (from free of A score of zero (no risk) to eight (multiple risks) was assigned to each of Failed grafts the health responses. The territory sales representative primarily the vascular population). Once the patient- of the bed company contracted to our region was care areas were recognized, it was then critical to instrumental in providing the task force with information determine and analyze the patient demand, (essentially, about each of the therapy mattresses available. The what diagnoses or health-care patterns were patients clinical data to support their function, anticipated presenting that warranted a therapy bed?). Table 1 outcome and specific features given the health demand identifies the patient clinical characteristics for each of of the patient were reviewed and incorporated into the the high/low demand areas. tool. An assessment score was developed that further 2. Doughty D, et al. Your patient: Which therapy? Journal of Enterostomal Therapy. 1990;17(4): 154-159. 3. Gordon M. Nursing Diagnosis: A Process and Application. McGraw-Hill. 1982. 4. Bergstrom N, et al. The Braden scale for predicting pressure score risk. Nursing Research. 1987;36(4): 205-210. identified the type of therapy bed for the score range. Documentation Development Continued on page 14 During this period, the health centre’s nursing documentation was undergoing redesign to reflect Marjorie TABLE 2 Gordon’s Functional Health Patterns.3 The typology of the functional health patterns provides an assessment Modified Gordon’s Functional Health Patterns framework for identifying a patient’s health pattern (with sixth and seventh categories added) profile. To be consistent with both the documentation policy of the health centre and the overall nursing documentation system, the Therapy Bed Task Force adapted Health–perception–health management patterns Nutritional–metabolic pattern five of Gordon’s 11 functional health patterns as the Elimination pattern overall framework for the assessment tool (see Table 2). Activity–exercise pattern The task force added a sixth and seventh health pattern, Sleep–rest pattern Mobility-Exercise and Integumentary. Integumentary Self perception–self-concept pattern was specifically added, rationalizing that the skin, as the Role–relationship pattern largest organ—being multifunctional and subjected to varying degrees of threat and injury—was deserving of its own category. The creative aspect of developing the therapy bed assessment tool came with identifying the range of Sexuality–reproductive pattern Coping–stress-tolerance pattern Value–belief pattern Cognitive–perceptual pattern Mobility–exercise Integumentary “health responses” within each of the assessment health Vo l u m e 2 , N u m b e r 2 Wo u n d C a re C a n a d a 13 Upon completion of the assessment TABLE 3 tool, the clinician calculates a total Therapy Bed Assessment Tool (TBAT) PO # Date Bed Received: Assessment 0–5 6–10 11–15 Room # Ht.: score, which provides a recommendWt.: Recommended Bed Type Not Recommended – Conservative First Step Select Therakair Max. 200 lbs. ambulatory, pressure relief, edema, pulsation mattress Kinair Max. 300 lbs., non-ambulatory, advanced pressure relief, no pulsation 16–20 Therapulse Max. 300 lbs., non-ambulatory, advanced pressure relief, edema, pulsation ICU only Biodyne Max. 300 lbs., rotation, wider bed, deeper cushion, advanced therapy relief Triadyne Kinetic rotation, percussion, vibration, pulsation, pressure relief Safety/Management Barikair Wt: 350–850 lbs. Date Risk Factor Assessment Score Wk. 1 Wk. 2 Wk. 3 Health Management Pattern Free of major non-active health problems 0 Intractable pain, grafts, myocutaneous flaps 1 PVD, failed grafts/flaps, edematous, septic, fractures 2 Hemodynamically unstable, chest trauma, CVA, neurological conditions, ventilatory instability 3 Activity-Exercise Pattern Ambulatory without assistance 0 Up in a chair, confined to chair/wheelchair 1 Bed rest 2 Mobility-Exercise Pattern Independently moves extremities 0 Two turning surfaces available 1 One turning surface available 2 Immobile 3 Elimination Pattern Full bowel/bladder control, no diaphoresis 0 Either bowel/bladder incontinence, or diaphoresis 1 Bowel and bladder incontinence, no diaphoresis 2 Bowel and bladder incontinence and diaphoresis 3 Integumentary No skin breakdown 0 Stage I—Epidermis intact, reddened 2 Stage II—Blistered, epidermis break, more than two ulcers, moderate to large draining wounds 4 Stage III and IV—Ulceration to tendon, bone, muscle 8 Nutritional-Metabolic Pattern Nourished—adequate food/fluid intake, weight stable 0 Malnourished—limited oral intake, dehydrated, obese, cachectic, IV therapy, enteral supplements 1 Supplemented—no oral intake, TPN 2 Cognitive Pattern Alert, oriented x 3 0 Confused, disoriented, responds to visual, verbal, pain stimuli 2 Comatose (no visual, verbal, pain response) 3 Total Score Nurse’s Initials 14 Wo u n d C a re C a n a d a ation for the type of therapy bed appropriate for the patient being assessed (see Table 3). Therapy Bed Assessment Tool Development The outcome was a Therapy Bed Assessment Tool, which is designed to guide the clinician through a systematic process of assessing the patient through each of the seven functional health patterns. The operational word here is “recommended.” The clinician must still use his or her judgment to match the needs of the patient with the recommendation, always leaning toward maximizing the patient’s potential with the therapy bed and supporting those areas the patient and staff cannot meet together. There are certainly limitations to this tool, as it was designed with the acutecare perspective only and it has never been put through the rigours of being tested for reliability or validity. However, it has reinforced that the prescriptive nature of a therapy bed shows that it is not “a luxury item” but is an important and necessary variable in the overall treatment plan, which is grounded in science and research. Note to readers: The printing of brand names in the assessment tool does not in any way indicate an endorsement by the Canadian Association of Wound Care or Wound Care Canada for any of the products listed. Brand name inclusion was permitted to preserve the original intent of the tool. Vo l u m e 2 , N u m b e r 2