Molecular Genetics and Metabolism 80 (2003) 74–80
www.elsevier.com/locate/ymgme
Minireview
Canavan disease: a monogenic trait with complex genomic interaction
Sankar Surendran, Kimberlee Michals-Matalon, Michael J. Quast, Stephen K. Tyring,
Jingna Wei, Ed. L. Ezell, and Reuben Matalon*
Department of Pediatrics, ChildrenÕs Hospital, The University of Texas Medical Branch, Galveston, TX 77555-0359, USA
Received 1 July 2003; received in revised form 8 August 2003; accepted 8 August 2003
Abstract
Canavan disease (CD) is an inherited leukodystrophy, caused by aspartoacylase (ASPA) deficiency, and accumulation of
N-acetylaspartic acid (NAA) in the brain. The gene for ASPA has been cloned and more than 40 mutations have been described,
with two founder mutations among Ashkenazi Jewish patients. Screening of Ashkenazi Jews for these two common mutations
revealed a high carrier frequency, approximately 1/40, so that programs for carrier testing are currently in practice. The enzyme
deficiency in CD interferes with the normal hydrolysis of NAA, which results in disruption of myelin and spongy degeneration of the
white matter of the brain. The clinical features of the disease are macrocephaly, head lag, progressive severe mental retardation, and
hypotonia in early life, which later changes to spasticity. A knockout mouse for CD has been generated, and used to study the
pathophysiological basis for CD. Findings from the knockout mouse indicate that this monogenic trait leads to a series of genomic
interaction in the brain. Changes include low levels of glutamate and GABA. Microarray expression analysis showed low level of
expression of GABA-A receptor (GABRA6) and glutamate transporter (EAAT4). The gene Spi2, a gene involved in apoptosis and
cell death, showed high level of expression. Such complexity of gene interaction results in the phenotype, the proteome, with spongy
degeneration of the brain and neurological impairment of the mouse, similar to the human counterpart. Aspartoacylase gene
transfer trial in the mouse brain using adenoassociated virus (AAV) as a vector are encouraging showing improved myelination and
decrease in spongy degeneration in the area of the injection and also beyond that site.
Ó 2003 Elsevier Inc. All rights reserved.
Keywords: Canavan disease; GABA; EAAT4; Spi2; AAV; Glutamate
Introduction and history
Canavan disease (CD), spongy degeneration of the
brain, is an autosomal recessive disorder. Canavan in
1931, described the histological findings of spongy degeneration of the white matter of the brain in a patient
thought to have Schilder disease [1]. Canavan disease, as
a specific entity, was recognized in 1949 by van Bogaert
and Betrand [2], who described three Jewish children
with spongy degeneration of the brain. The disease is
caused by aspartoacylase (ASPA) deficiency [3] resulting
accumulation of N-acetylaspartic acid (NAA) in the
brain [3]. The urine of patients with CD contain elevated
levels of NAA, so that urine testing can be diagnostic
and brain biopsy is no longer needed for the diagnosis.
*
Corresponding author. Fax: 1-409-772-9595.
E-mail address: rmatalon@utmb.edu (R. Matalon).
1096-7192/$ - see front matter Ó 2003 Elsevier Inc. All rights reserved.
doi:10.1016/j.ymgme.2003.08.015
After the discovery of ASPA deficiency in CD, the gene
for ASPA was cloned and mutations that cause CD were
identified. While two mutations are the molecular basis
of CD among Jewish patients, a wide range of mutations
were found among non-Jewish patients with CD [4–8].
The creation of a knockout mouse for CD [9] affords the
opportunity to investigate the molecular events that lead
to the pathophysiology of CD and also experiment with
gene transfer to the brain.
Clinical course of CD
Infants with CD appear normal during the first few
months of life, although careful examination reveals
mild delays, hypotonia, and inadequate visual tracking.
These infants become progressively irritable, and remain
hypotonic with poor head control. Developmental delay
S. Surendran et al. / Molecular Genetics and Metabolism 80 (2003) 74–80
and larger head become noticeable after 6 months of
age. The hypotonia, head lag, and megalencephaly are
common features of CD, and should lead the physician
to consider leukodystrophy [10]. When children with
CD become older, developmental delays such as, motor
and verbal skills become obvious. In spite of the profound delays, children with CD are able to interact,
laugh, smile, reach for objects, and lift their head when
in prone position. Patients do not develop the ability to
sit, stand, walk or talk. Children with CD develop optic
atrophy and have difficulty focusing, but are able to
recognize their surroundings. When patients with CD
become older, hypotonia gives way to spasticity. Feeding difficulties increase with age, and feeding by a nasogastric tube or permanent gastrostomy will be needed.
With improved nursing and medical care such patients
can reach the second decade of life or beyond that
[11,12].
Diagnosis of CD
The diagnosis of CD relies on demonstrating high
levels of NAA in the urine. The NAA in the urine of a
patient with CD is more than 50 times the normal urinary level. The mean values of urine NAA in normal
and CD patients were, 23.5 16.1 (n ¼ 53) and
1440.5 873.3 (n ¼ 95) lmol/mmol creatinine, respectively [13]. Patients with a slight increase in urine NAA
are often confused with Canavan disease [7]. NAA is
elevated about 3-fold in blood and CSF in patients with
CD. Blood does not have ASPA activity and enzyme
activity in cultured fibroblasts is difficult to interpret
because the enzyme activity is sensitive to culture conditions. Brain biopsy is no longer needed for the diagnosis of CD. Mutation analysis is important to
determine the genotype for purposes of counseling.
Mutation expression needs to be determined because
some mutations are polymorphic [7].
Computed tomography (CT) scan of the head or
magnetic resonance imaging (MRI) of the brain show
diffuse white matter degeneration in CD [14–16].
Nuclear magnetic resonance spectroscopy (MRS) of the
CD brain show increase in the peak of NAA [16–18].
75
Fig. 1. Diagram of the gene for aspartoacylase with 5 introns and 6
exons. The human ASPA gene spans 39 kb and it is localized in the
short arm of chromosome 17(17p-ter). Mutation E285A mutation in
exon 6 and Y231X in exon 5 are the common Jewish mutations. In
non-Jewish populations, mutations vary.
cDNA, suggesting that ASPA is highly conserved during
evolution [20]. The genomic organization of the gene for
ASPA with various mutations is shown in Fig. 1. Some
mutations in exon 6 of the gene shows polymorphism
and the polymorphic mutations do not change the
enzyme activity [21,22]. Therefore expression studies
are important to understand functional significance of
mutations.
There are two mutations, E285A and Y231X that
account for over 96% of the mutations among Ashkenazi Jewish population [13,19]. Carrier frequency for
CD among Ashkenazi Jewish populations has ranged
from 1/37 to 1/60 [23,24]. This high frequency of carriers
means that routine preventive measure using DNA
analysis for the common Jewish mutations needs to be
recommended for Ashkenazi Jews.
In non-Jewish patients the mutations are more variable. The most common mutation in non-Jewish patients is A305E [23]. There have been over 40
mutations identified in various ethnic groups [8,12,25–
28]. Many appear to be sporadic mutations that run in
families. Mutation D114Y was found in a small geographical region in Norway and D249V mutations was
specific to Norwegian and Swedish population [29] indicating some mutations in the ASPA gene are founder
mutations.
Genotype and phenotype correlation
Aspartoacylase gene
Aspartoacylase gene was cloned and localized on the
short arm of chromosome 17 (17p13-ter) [19,20]. The
human aspartoacylase gene spans 30 kb, contains five
introns and six exons coding for 313 aminoacids [19], an
enzyme with a molecular weight of 36 kDa. Southern
blotting of genomic DNA from eukaryotes including
rabbit, chicken, monkey, mouse, dog, cow, and yeasts
show fragments that hybridize with human ASPA
The majority of patients with Canavan disease have
a severe phenotype. The Jewish mutations E285A and
Y231X lead to a severe phenotype. Homozygosity of
the common non-Jewish mutation A305E has been
reported with both severe and mild CD [25]. The nonJewish mutation, D249V, converts a negatively charged
aspartate residue into a hydrophobic valine residue,
resulting in complete loss of ASPA activity. Phenotypically patients with D249V have a severe phenotype
76
S. Surendran et al. / Molecular Genetics and Metabolism 80 (2003) 74–80
with nystagmus and irritability at birth [8]. Mutations
that disrupt the conformation of the active site of
ASPA [26,27] will result in total loss of enzyme activity
and a severe phenotype. Mutation C152W forms a
disulfide bond that disrupts the active site [8]. Thus
severe genotypes often correspond to a severe phenotype.
Prevention and prenatal diagnosis
Carrier detection and genetic counseling are important to prevent CD. These approaches are now being
promoted for the Jewish population using DNA samples to determine the common Jewish mutations for
CD. When both parents are carriers and their mutations are known they are informative for prenatal diagnosis [30,31]. Prenatal diagnosis based on mutation
analysis should also include the study of other DNA
markers to avoid possible maternal cell contamination
[31]. In non-informative families, the biochemical assay
for NAA in amniotic fluid should be offered and progressive increase of NAA (5- to 10-fold) in the amniotic fluid can be used for prenatal diagnosis of CD
[32,33].
Pathology of CD brain
Aspartoacylase, the enzyme deficient in Canavan
disease, hydrolyzes NAA to acetate and aspartate
(Fig. 2). Aspartoacylase is abundant in the white
matter of the brain, kidney and to a lesser extent in
liver and other tissues. Aspartoacylase activity is localized in the white matter and NAA is synthesized in
the gray matter of the brain [9,34] and this compartmentation of substrate and enzyme in different regions
of the brain require a mechanism to transport NAA to
the site of the enzyme, the oligodendrocytes for its
normal metabolism [35]. The discovery of the enzyme
defect in CD indicates that normal metabolism of
NAA is important for the synthesis and maintenance
of healthy white matter. The level of NAA in the human brain is 8-mmol/g tissue [10]. The swollen astrocytes from the brain of a child with CD are shown in
Fig. 3. The increased levels of NAA in CD lead to
swelling or sponginess of the brain. The osmolite role
-OOC. CH . CH. COO- + H O
2
2
HN.CO.CH3
N-Acetylaspartic acid
ASPA
-OOC. CH .CH.COO- + CH . COO2
3
L-Aspartic acid
Acetate
Fig. 2. Aspartoacylase (ASPA) hydrolyzes N-acetylaspartic acid
(NAA) to acetate and aspartic acid. Deficiency of ASPA leads to
accumulation of NAA.
Fig. 3. Subcortical spongy changes in the white matter of the brain in a
patient with CD.
of NAA and its lack of hydrolysis in CD lead to water
accumulation in the brain [36,37]. The mitochondria also gets distorted and elongated in CD brain
[13,38,39] suggesting that energy metabolism may be
affected.
Knock-out mouse for CD
The mouse 129/SvJ ASPA gene was cloned in our
laboratory. The ASPA coding sequence in mouse is
approximately 86% identical to the human ASPA
cDNA sequence in the ORF region [20]. The longest
uninterrupted ORF in the cDNA is 936 bases that
predicted 312 aminoacids residues of mouse ASPA
protein, while 313 aminoacids are observed in human
ASPA protein. Deletion of 10 bp from exon 4 of the
mouse ASPA cDNA was accomplished and followed
by Cre-mediated recombination. These experiments
resulted in a knockout mouse for Canavan disease
[9].
Spongy degeneration observed by MRI and peaks
of NAA in the CD mouse brain analyzed using MRS
S. Surendran et al. / Molecular Genetics and Metabolism 80 (2003) 74–80
77
Fig. 4. The proton spectra of brain extracts of (A) Canavan and (B) wild type mice. The peak areas are creatine, NAA, glutamate, and GABA. In the
wild type brain, GABA and glutamate levels are higher than Canavan mice. The NAA level is high in the Canavan mouse brain.
are shown in Fig. 4. This type of signal intensity and
elevated NAA is similar to the white matter changes
observed in patients with CD. The vacuolation of the
white matter in the deep cortex and white matter
bundles in the corpus striatum was found in the CD
mouse [9] and can be observed in patients with CD.
Vacuolation in the brain of CD mouse is shown in
Fig. 5. Urine NAA is approximately 10-fold higher in
CD mice compared to the wild type [9]. The
knockout mouse for CD showed higher bone mineral
loss compared to the wild type of similar age [40].
This is probably associated with the muscle weakness
observed in the mouse with CD.
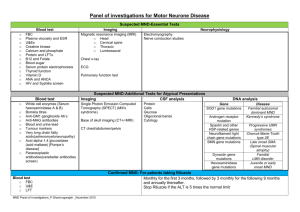
Analysis of CD mouse brain revealed abnormal
expressions of serine proteinase inhibitor (Spi2), the
GABA-A receptor-GABRA6, neurogenic differentiation factor, genes involved in inflammatory reaction
and cell death and the glutamate transporter, EAAT4.
While glutamate, EAAT4, c-amino butyric acid
(GABA) and GABRA6 levels were down regulated in
the CD mouse brain, Spi2 level was increased [41]
(Table 1). The peaks of glutamate and GABA are
shown in Fig. 4. The abnormal expression of these
genes in the cerebellum of the brain, may be responsible for hypotonia and muscle weakness observed in
CD [41]. These observations need to be studied in
humans with CD. Aspartate aminotransferase was
also lower in the CD mouse brain [40]. These studies
suggesting involvement of multiple genomic interactions in the pathophysiology observed in CD.
78
S. Surendran et al. / Molecular Genetics and Metabolism 80 (2003) 74–80
Gene therapy
Fig. 5. Spongy degeneration in the subcortex of the CD mouse brain.
Vacuoles are seen in the CD mouse brain, while no vacuoles are found
in the wild type.
The brain pathology in CD is more complex than just
NAA accumulation. Thus the creation of the CD mouse
should give insight in the changes of the brain resulting
in the CD phenotype.
Gene therapy for CD was first carried out with
plasmid containing ASPA gene prepared by incorporating 145 bp inverted terminal repeats (ITRs) from
AAV and the LPD/pAAV-ASPA complex was injected
in the ventricles of two patients with CD [42]. Even after
a 1-year period, efficacy of the treatment was retained in
one patient by reducing NAA level to normal range. The
MRI study on the patient suggested new myelination of
the corpus callosum as well as basal ganglia and the
posterior limb of the internal capsule after 9 months of
treatment [42]. The other treated patient showed normal
level of NAA in the occipital lobe for 9 months. However, improvement of myelination was not observed
after 9 months [42]. Currently, there is a protocol for the
use of rAAV2-ASPA to treat with patients with CD [43].
The knockout mouse for CD is being used for experimentation with gene transfer. The rAAV2-ASPA
was used for injection into the striatum and thalamus of
the brain of the knock-out CD mouse and the efficacy
was studied until 5 months period after treatment. The
mouse showed less sponginess and reduction in the elevation of NAA beyond the injected site as examined by
MRI/MRS [44,45]. The ASPA activity increased after
AAV mediated ASPA gene transfer and activity remained even 5 months after injection while the site of
rAAV2-GFP injected mice did not result in any change
in sponginess or ASPA activity [44,45]. Although the
improvement of brain histology extends beyond the site
of injection, remote areas such as cerebellum are not
affected by rAAV-ASPA.
Table 1
Microarray expression and quantitative analysis in the brain of knockout mouse for CD
GenBank Accession No.
Fold
Genes
(A) Microarray expression analysis showing abnormal gene expression
Cell growth/signal transduction genes
AJ222970
119.1#
GABRA6
U28068
7.0#
Neurogenic differentiation
factor mRNA
D83262
9.7#
Glutamate transporter
EAAT4 mRNA
D10210
16.0#
D -Aminoacid oxidase
mRNA
Cell death and inflammatory genes
M64086
29.8"
Y13089
L28095
4.4"
3.8"
Spi2 proteinase inhibitor
mRNA
Caspase-11 mRNA
IL-1b converting enzyme
(B) Quantitative analysis showing abnormal levels of glutamate, GABA, and Spi2
Real-time RT-PCR
Knockout mouse
Brain
GABRA6
Spi2
>2800-fold#
(<10 copies/lg RNA)
6-fold"
Arrows shows: ", higher; #, lower in the knockout mouse brain.
Biochemical assay
of glutamate
NMR spectra
of GABA
5-fold#
67%#
S. Surendran et al. / Molecular Genetics and Metabolism 80 (2003) 74–80
Conclusion
Since the discovery of basic defect for CD, substantial
studies have been made in the identification of the gene
for ASPA and mutations that lead to CD. Thus there is
a clear molecular mechanism for diagnosis and prevention. Studies at the molecular level using the knockout
mouse reveal information about the complexity of this
monogenic trait and the resulting phenotype. Gene
transfer in the knockout mouse is an important step for
human gene therapy of CD.
References
[1] M.M. Canavan, SchilderÕs encephalitis perioxalis diffusa, Neurology 15 (1931) 299–308.
[2] L. van Bogaert, I. Betrand, Sur une idiotie familiale avec
degerescence sponglieuse de neuraxe (note preliminaire), Acta
Neurol. 49 (1949) 572–587.
[3] R. Matalon, K. Michals, D. Sebasta, M. Deaching, P. Gashkoff, J.
Casanova, Aspartoacylase deficiency and N-acetylaspartic aciduria in patients with Canavan disease, Am. J. Med. Genet. 29
(1988) 463–471.
[4] R. Kaul, G.P. Gao, M. Aloya, K. Balamurugan, R. Matalon,
Canavan disease: mutations among Jewish and non-Jewish
patients, Am. J. Hum. Genet. 55 (1994) 34–41.
[5] R. Kaul, R. Matalon, G.P. Gao, K. Balamurugan, K. Michals, M.
Aloya, A. Petrosky, et al., Spectrum of Canavan mutations among
Jewish and nonJewish patients, Am. J. Hum. Genet. (Suppl. 55)
(1994) 212.
[6] O.N. Elpeleg, Y. Anikster, V. Barash, D. Bransky, A. Shaag, The
frequency of C854 mutation in the aspartoacylase gene in
Ashkenazi Jews in Isreal, Am. J. Hum. Genet. 55 (1994) 287–288.
[7] S. Surendran, F.J. Bamforth, A. Chan, S.K. Tyring, S.I. Goodman, R. Matalon, Mild elevation of N-acetyl aspartic acid and
macrocephaly: a diagnostic problem, J. Child Neurol. (2003) (in
press).
[8] B.J. Zeng, Z.H. Wang, L.A. Ribeiro, P. Leone, R. De Gasperi,
S.J. Kim, S. Raghavan, E. Ong, G.M. Pastores, E.H. Kolodny,
Identification and characterization of novel mutations of the
aspartoacylase gene in non-Jewish patients with Canavan disease,
J. Inherit. Metab. Dis. 25 (2002) 557–570.
[9] R. Matalon, P.L. Rady, K.A. Platt, H.B. Skinner, M.J. Quast,
G.A. Campbell, K. Matalon, J.D. Ceci, S.K. Tyring, M. Nehls, S.
Surendran, J. Wei, E.L. Ezell, S. Szucs, Knock out mouse for
Canavan disease: a model for gene transfer to the central nervous
system, J. Gene Med. 2 (2000) 165–175.
[10] R. Matalon, K. Michals-Matalon, Spongy degeneration of the
brain, Canavan disease: biochemical and molecular findings,
Pediatr. Pathol. Mol. Med. 18 (2000) 471–481.
[11] R. Matalon, K. Michals-Matalon, Molecular basis of Canavan
disease, Eur. J. Paediatr. Neurol. 2 (1998) 69–76.
[12] R. Matalon, K. Michals-Matalon, Spongy degeneration of the
brain, Canavan disease: biochemical and molecular findings,
Front. Biosci. D (2000) 307–311.
[13] R. Matalon, K. Michals-Matalon, Recent advances in Canavan
disease, Adv. Pediatr. 46 (1999) 493–506.
[14] A.R. Rushton, B.A. Shaywitz, C.C. Duncan, R.B. Geehr, E.E.
Manuelidis, Computerized tomography in the diagnosis of Canavan disease, Ann. Neurol. 10 (1981) 57–60.
[15] J. Brismar, G. Brismar, G. Gascon, P. Ozand, Canavan disease:
CT and MR imaging of the brain, Am. J. Neurol. Res. 11 (1990)
805–810.
79
[16] R. Matalon, K. Michals, R. Kaul, M. Mafee, Spongy degeneration
of the brain, Canavan disease, Int. Pediatr. 5 (1990) 121–124.
[17] W. Grodd, I. Kragaloh-Mann, D. Peterson, F.K. Trefz, K.
Harzer, In vivo assessment of N-acetylaspartate in brain in spongy
degeneration (Canavan disease) by proton spectroscopy, Lancet
336 (1990) 437–438.
[18] H.J. Wittsack, H. Kugel, B. Roth, W. Heindel, Quantitative
measurements with localized 1H NMR spectroscopy in children
with Canavan disease, J. Magn. Reson. Imaging 6 (1996) 889–893.
[19] R. Kaul, G.P. Gao, K. Balamurugan, R. Matalon, Human
aspartoacylase cDNA and mis-sense mutation in Canavan disease,
Nat. Genet. 5 (1993) 118–123.
[20] R. Kaul, K. Balamurugan, G.P. Gao, R. Matalon, Canavan
disease: genomic organization and localization of human ASPA to
17p13-ter: conservation of the ASPA gene during evolution,
Genomics 21 (1994) 364–370.
[21] O. Propheta, N. Magal, M. Shohat M, N. Eyal, N. Navot, M.
Horowitz, A benign polymorphism in the aspartoacylase gene
may cause misrepresentation of Canavan gene testing, Eur. J.
Hum. Genet. 6 (1998) 635–637.
[22] R.L. Alford, J.M. DeMarchi, C.S. Richards, Frequency of a DNA
polymorphism at position Y231 in the aspartoacylase gene and its
impact on DNA-based carrier testing for Canavan disease in
Ashkenazi Jewish population, Hum. Mutat. (Suppl. 1) (1998)
S161–162.
[23] R. Matalon, R. Kaul, K. Michals, Carrier rate of Canavan disease
among Ashkenazi Jewish individuals, Am. J. Hum. Genet. 55
(1994) A157.
[24] D. Kronn, C. Oddoux, J. Phillips, H. Ostrer, Prevalence of
Canavan disease heterozygotes in the New York metropolitan
Ashkenazi Jewish individuals, Am. J. Hum. Genet. 57 (1995)
1250–1252.
[25] A. Shaag, Y. Anikster, E. Christensen, J.Z. Glustein, A. Fois, H.
Michelakakis, F. Nigro, E. Pronicka, A. Ribes, M.T. Zabot, O.N.
Elpeleg, The molecular basis of Canavan (Aspartoacylase deficiency) disease in European non-Jewish patients, Am. J. Hum.
Genet. 57 (1995) 572–580.
[26] R. Kaul, G.P. Gao, K. Michals, D.T. Whelan, S. Levin, R.
Matalon, Novel (cys 125 arg) missense mutation in an Arab
patient with Canavan disease, Hum. Mutat. 5 (1995) 269–271.
[27] R. Kaul, G.P. Gao, R. Matalon, M. Aloya, Q. Su, M. Jin, A.B.
Johnson, R.B. Shutgens, J.T. Clarke, Identification and expression of eight novel mutations among non-Jewish patients with
Canavan disease, Am. J. Hum. Genet. 59 (1996) 95–102.
[28] K. Kobayashi, S. Tsujino, T. Ezoe, H. Hamaguchi, K. Nihei, N.
Sakuragawa, A missense mutation I143T in a Japanese patient
with Canavan disease, Hum. Mutat. (Suppl. 1) (1998)
S308– S309.
[29] T.R. Olsen, L. Tranebjaerg, E.A. Kvittingen, L. Hagenfeldt, C.
Moller, O. Nilssen, Two novel aspartoacylase (ASPA) gene
missense mutations specific to Norwegian and Swedish patients
with Canavan disease, J. Med. Genet. 39 (2002) e55.
[30] O.N. Elpeleg, A. Shaag, Y. Anikster, C. Jakobs, Prenatal
detection of Canavan disease (aspartoacylase deficiency) by
DNA analysis, J. Inherit. Metab. Dis. 17 (1994) 664–666.
[31] R. Matalon, R. Kaul, G.P. Gao, Prenatal diagnosis for Canavan
disease: the use of DNA markers, J. Inherit. Metab. Dis. 18 (1995)
215–217.
[32] M.J. Bennett, K.M. Gibson, W.G. Sherwood, P. Divry, M.O.
Rolland, O.N. Elpeleg, P. Rinaldo, C. Jackobs, Reliable prenatal
diagnosis of Canavan disease (Aspartoacylase deficiency): comparison of enzymatic and metabolite analysis, J. Inherit. Metab.
Dis. 16 (1993) 831–836.
[33] R.I. Kelley, Prenatal diagnosis of N-acetyl-L -aspartate in amniotic
fluid, J. Inherit. Metab. Dis. 16 (1993) 918–919.
[34] L. Ory-Lavolle, R.D. Blakely, J.T. Coyle, Neurochemical and
immunochemical studies on the distribution of N-acetylaspar-
80
[35]
[36]
[37]
[38]
[39]
[40]
[41]
S. Surendran et al. / Molecular Genetics and Metabolism 80 (2003) 74–80
tylglutamate and N-acetyl-aspartate in the rat spinal cord and
some pheripheral nervous tissues, J. Neurochem. 48 (1987)
895– 899.
T.N. Sager, C. Thomsen, J.S. Valsborg, H. Laursen, A.J. Hanson,
Astroglia contains a specific transport mechnism for N-acetyl-L aspartate, J. Neurochem. 73 (1999) 807–811.
B.T. Adornato, J.S. OÕBrien, P.W. Lampert, Cerebral spongy
degeneration of infancy: a biochemical and ultrastructural study
of affected twins, Neurology 22 (1972) 202–210.
M.H. Baslow, Molecular water pumps and the aetiology of
Canavan disease: a case of the sorcererÕs apprentice, J. Inherit.
Metab. Dis. 22 (1999) 99–101.
M. Adachi, J. Torii, L. Schneck, B.W. Volk, Electron microscopic
and enzyme histochemical studies of the cerebellum in spongy
degeneration (van Bogaert and Bertrand type), Acta Neuropathol.
20 (1972) 22–31.
Y. Luo, K. Huang, Spongy degeneration of the CNS in infancy,
Arch. Neurol. 41 (1984) 164–170.
S. Surendran, K. Matalon, S. Szucs, S.K. Tyring, R. Matalon,
Metabolic changes in the knock-out mouse for Canavan disease:
implications to patients with CD, J. Child Neurol. (2003) (in press).
S. Surendran, P.L. Rady, K. Matalon, M.J. Quast, D.K. Rassin,
G.A. Campbell, E.L. Ezell, J. Wei, S.K. Tyring, S. Szucs, R.
[42]
[43]
[44]
[45]
Matalon, Expression of glutamate transporter, GABRA6, serine
proteinase inhibitor 2 and low levels of glutamate and GABA in
the brain of knock-out mouse for Canavan disease, Brain Res.
Bull. 61 (2003) 427–435.
P. Leone, C.G. Janson, L. Bilanuk, Aspartoacylase gene transfer
to the central nervous system with therapeutical implications for
Canavan disease, Ann. Neurol. 48 (2000) 27–38.
C. Janson, S. McPhee, L. Bilaniuk, J. Haselgrove, M. Testaiuti, A.
Freese, D.J. Wang, D. Shera, P. Hurh, J. Rupin, E. Saslow, O.
Goldfarb, M. Goldberg, G. Larijani, W. Sharrar, L. Liouterman,
A. Camp, E. Kolodny, J. Samulski, Clinical protocol. Gene
therapy of Canavan disease: AAV-2 vector for neurosurgical
delivery of aspartoacylase gene (ASPA) to the human brain, Hum.
Gene Ther. 13 (2002) 1391–1412.
R. Matalon, P. Rady, S. Surendran, M.J. Quast, G.A. Campbell,
R.J. Mandel, N. Muzyczka, Delivery of rAAV-aspartoacylase in
knock out mouse for Canavan disease, J. Inherit. Metab. Dis.
(Suppl. 1) (2001) 123.
R. Matalon, S. Surendran, P.L. Rady, M.J. Quast, G.A. Campbell, K. Matalon, S.K. Tyring, J. Wei, C.S. Peden, E.L. Ezell, N.
Muzyczka, R.J. Mandel, Adeno-associated virus mediated aspartoacylase gene transfer to the brain of knock out mouse for
Canavan disease, Mol. Ther. 7 (2003) 580–587.