Aspirin and Salicylates
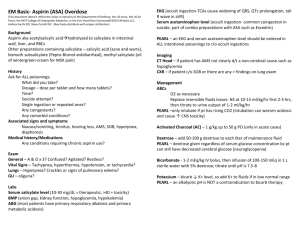
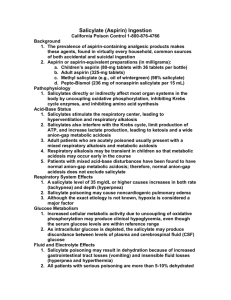
advertisement

Aspirin and Salicylates Salicylate-induced acute lung injury has been observed in humans. mecanisem is increased pulmonary vascular permeability This vascular injury also may involve the kidneys. Proteinuria is a prominent early finding in salicylate toxicity, starting at a serum salicylate concentration of >30 mg/dL, and it is directly related to salicylate concentrations. • glucose homeostasis: Although salicylate causes mobilization of glycogen stores, resulting in hyperglycemia, it is also a potent inhibitor of gluconeogenesis. • Therefore, normoglycemia, hyperglycemia, or hypoglycemia may occur in salicylate toxicity. • Animal studies demonstrate that toxic doses of salicylate produce a profound decrease in brain glucose concentration despite normal serum glucose concentrations. • This finding suggests that the supply of glucose to the brain in salicylate poisoning may be inadequate, even though serum glucose concentrations are normal. Antiplatelet activity is a well-known effect of aspirin, but hemorrhage is a rare complication of acute, single, massive overdose. typical clinical presentation includes : nausea and vomiting tinnitus hearing loss sweating hyperventilation • Tinnitus may develop in patients on chronic salicylate therapy when the serum salicylate concentration is at the upper limit of the therapeutic range of 20 mg/dL. • • • • • • • Uncommon features of acute salicylism include : fever neurologic dysfunction renal failure acute lung injury cardiac dysrhythmia hypoglycemia • Each of these uncommon manifestations indicates more severe poisoning, with associated greater morbidity and mortality • Other rare complications include: • rhabdomyolysis • gastric perforation • GI hemorrhage Several commercially available tests can qualitatively detect salicylate in the urine. However, there are severe limitations associated with bedside detection techniques for salicylic acid, their role has little utility in most clinical settings, and positive results must be confirmed with serum salicylate concentration. Commercially available tests for serum salicylate concentration are very accurate, and the only reported significant interference has been with diflunisal, which produces false positive results for significantly high serum salicylate concentrations. Some enteric-coated medications are radiopaque and visible on an abdominal radiograph. Thus, a positive radiograph can confirm that pills are present, but a negative radiograph does not exclude enteric-coated or modified-release tablets in the GI tract. Essential laboratory tests include : serum salicylate concentrations electrolytes glucose blood urea nitrogen and creatinin Arterial blood gases chest and abdominal radiograph ECG complete blood count serum calcium level urinalysis with urine pH determination There is no specific antidote for salicylate toxicity. The priority is immediate resuscitation with stabilization of airway, breathing, and circulation. Subsequent steps involve: correction of volume depletion metabolic derangements GI decontamination reduction in body salicylate burden • Salicylates can induce pylorospasm and form gastric bezoars, so that lavage may be beneficial even when performed more than 1 hour from the ingested overdose • However, the large size of enteric-coated and modified-release tablets may make them difficult to remove from the stomach • Salicylate absorption is effectively reduced by the administration of activated charcoal . • A single dose of activated charcoal, 1 to 2 gr/kg should be administered to patients who have ingested potentially toxic amounts of salicylate. There are no convincing data to support the use of repeated or multiple doses of activated charcoal in salicylate overdose. • Patients with severe salicylate intoxication are usually volume depleted,and have serious acid-base disturbances • Thrifor require IV volume and electrolyte replacement. • Careful assessment of a patient's volume and electrolyte status is important, particularly in the elderly and in patients with a history of cardiac disease. • Volume replacement is initially undertaken with normal saline, and because hypokalemia is common, potassium should be added to the infusion after adequate urine output has been established. • Serum potassium should be maintained in the 4.0 to 4.5 mEq/L • Supplemental potassium may be required as correction of acidemia further shifts potassium into cells. Urinary alkalinization does enhance salicylate elimination and is an effective treatment for salicylate toxicity, although the precise mechanism is debated. • Although a good outcome with urinary alkalinization as the only method to enhance elimination was reported for a severely poisoned patient • most toxicologists would opine that urinary alkalinization is a useful initial technique but should not be perceived as a substitute for hemodialysis in severe salicylism • A common approach is to volume restore patients with normal saline to a target urine output of 1 to 2 mL/kg/h. • Concurrently, in a second IV line, an IV bolus of sodium bicarbonate (1 to 2 mEq/kg) is given followed by a continuous infusion (three ampules of either 44 or 50 mEq/ampule of sodium bicarbonate added to 1 L of 5% dextrose in water). • The infusion is started at 2 to 3 mL/kg/h and adjusted to maintain the urine pH >7.5. • Except for the fluids used for initial resuscitation, all IV fluids administered should contain a minimum of 50 gr/L of glucose (5% dextrose in water) because hypoglycemia has been implicated in the pathophysiology of salicylate neurologic injury. • Patients with acute lung injury should be managed as are patients with acute lung injury from other causes. • Pulmonary edema begins to improve concomitantly with the lowering of serum salicylate concentrations, and this suggests that aggressive efforts toward rapid elimination by hemodialysis In addition, early hemodialysis enables removal of salicylate without the volume challenge that accompanies sodium bicarbonate administration, and it avoids the possibility of aggravating lung injury. Patients with clinically significant bleeding should be treated with fresh frozen plasma. Indications for hemodialysis include: salicylism requiring respiratory and ventilatory support clinical deterioration or failure of improvement despite intensive supportive care and an alkaline diuresis lack of success in establishing an alkaline urine renal insufficiency severe acid-base disturbance altered mental status patients with acute lung injury A patient may be discharged from the ED if it can be determined that the patient had an inconsequential salicylate overdose. It is recommended that a patient who has overdosed on enteric-coated or modified-release preparations of aspirin be treated regardless of initial serum salicylate concentrations, be observed for at least 24 hours, and obtain serial serum salicylate concentrations until a declining level is confirmed.