Poisoning and Toxicology
advertisement
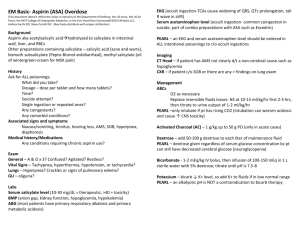
Poisoning and Toxicology 34 year old man presents to the hospital after being found in his apartment. According to NetCare, he has no significant past medical history except for multiple emergency room visits for coma from alcohol overdoses. He does not respond to painful stimuli and his breathing is shallow with O2 sats 89% but his blood pressure is 112/47 and heart rate is 85. You suspect that the patient has an overdose. What further information should you seek? – EMS: Empty cheap liquor bottles found at the scene. No suicide note nor any prescription medications. – Friend listed as contact: No known prescribed medications. Lots of problem with alcohol and recently was cut off EI and has run out of money. When examining the patient, what toxidromes and characteristics should you look for? – – – – – – – – Sympathomimetics Anticholinergic Hallucinogenics Opioid Sedative-hypnotic Cholinergic Serotonin Tricyclic antidepressant What investigations would you order? Describe the initial approach to the management of the poisoned patient. – Airway – Breathing – Circulation – Decontamination What antidotes are available and what role do they have in poisonings? On ABG, the patient is found to have an anion gap of 23. What is the differential for poisonings with an anion gap? – Consider: Methanol, ethanol, ethylene glycol INH, salicylates, metformin CO,CN, H2S, methemoglobin (cellular asphyxiants) Sympathomimetics How would you calculate the osmolar gap? The osmolar gap is 39. The ethanol level is 5 mmol/L. What is the differential for an elevated osmolar gap? – Consider: Ethanol, ethylene glycol, methanol, isopropyl alcohol Mannitol While awaiting confirmatory tests, you decide to initiate therapy. What treatments are available? 56 year old man with a past history of CAD presents with SOB and ringing in the ears. His initial ABG demonstrates a pH 7.45, PCO2 20, PO2 110, HCO3 20 and lactate 5. In the absence of any further history, what is the most likely ingestant? What is the mechanism of action of salicylate toxicity? Describe the clinical features (symptoms, signs and acid/base abnormalities) of salicylate toxicity? Discuss the management of salicylate intoxication? What is the role for alkalinization? What is the role of hemodialysis? 23 year old woman with a past medical history of depression presents to the hospital after reportedly taking 50 extrastrength Tylenol 3 hours ago. On examination, she is hemodynamically stable with no physical findings and no lab abnormalities. What is your initial approach and management of this patient? How does acetaminophen cause hepatoxicity and how does Nacetlycysteine prevent it? Suppose the patient presented 72 hours after ingestion. Her ALT is 1250, tylenol level 0, pH 7.23 and INR 3.0. How would you alter your management? At what point would you consider transplant? 24 year old boyfriend of the previous patient presents to hospital with acute psychosis. Soon after arrival, he develops generalized seizures lasting 15 seconds. On examination, he is febrile, blood pressure 87/32, heart rate of 143, O2 sats 91% on 5 L/min. Between seizures he is flushed, generally stiff with upgoing toes and clonus. His pupils are dilated, and his abdomen is distended. Head CT is normal as is CXR and ECG demonstrates only sinus tachycardia. What toxidrome does this presentation most resemble? EMS confirms that several empty bottles of Elavil were found at the scene as well as a suicide note. The patient is quite distraught by his girlfriend’s recent hospitalization. What are the pharmacological effects of tricyclic antidepressants? – – – – – – Presynaptic neurotransmitter reuptake Cardiac sodium channels Muscarinic acetylcholine receptors Peripheral alpha-1 adrenergic receptors Histamine receptors GABA-A receptors Describe the clinical features of TCA overdose; especially the cardiac, CNS and peripheral effects. How would you resuscitate this patient? What role does NaHCO3 have in the management of TCA poisoning and how does it work? If the patient developed a wide complex tachycardia, what antiarrhymics could be used? How would you treat this patient’s seizures? What issues can occur when decontaminating? 68 year old man with a history of heart failure recently started on Paxil for depression presents with fatigue, abdominal pain, confusion, and vomiting. His vital signs are 112/83, pulse 35, respiratory rate 20, and O2 sats 95%. His initial ECG demonstrates junctional rhythm. His ABG is normal except his K is 5.5. You suspect drug toxicity after ruling out other causes. What medications are on the differential diagnosis? The digoxin level is 4.6 nmol/L. What is the mechanism of action of digoxin and why is it toxic? How would you treat this patient? Should you treat the hyperkalemia? Would a potassium level of 3.4 mmol/L be reassuring? Questions??