Current Practices Toolbox - HIMSS Nursing Informatics
advertisement

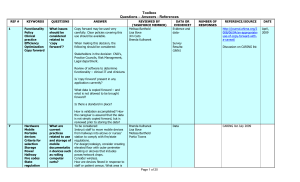
Toolbox Questions – Answers - References REF # 1 KEYWORDS Functionality Policy Clinical practice Efficiency Optimization Copy forward QUESTIONS What issues should be considered related to ‘copy forward’? ANSWER Copy forward may be used very carefully. Clear policies covering this use should be available. When making this decision, the following should be considered: REVIEWED BY (TASKFORCE MEMBER) Melissa Barthold Lisa Bove Jim Cato Brenda Kulhanek DATA OR EVIDENCE? Evidence and dataSurvey Results: (date) REFERENCE/SOURCE http://journal.ahima.org/200 8/06/04/an-appropriate-useof-copy-forward-with-acaveat/ Discussion on CARING list Stakeholders in the decision: CNO’s, Practice Councils, Risk Management, Legal department. Review of software to determine functionality – clinical IT and clinicians Is ‘copy forward’ present in any application currently? What data is copied forward – and what is not allowed to be brought forward? Is there a standard in place? 7 Hardware Mobile Portable devices Criteria for selection Storage Power Hallway Fire codes State regulation What are current practices related to use and storage of mobile documentatio n devices such as rolling computer carts? How is validation accomplished? How the caregiver is assured that the data is not simply copied forward, but is reviewed prior to storing the data? To be considered: Instruct staff to move mobile devices from hallways into alcove or nurses’ station to comply with fire/state regulations. For design/redesign, consider creating elevated floor with outer perimeter docking or alcoves that includes power/network drops. Consider wireless. How are devices flexed in response to staff or patient census. What area is Brenda Kulhanek Lisa Bove Melissa Barthold Portia Towns Page 1 of 28 Data CARING list July 2009 DATE April, 2009 Toolbox Questions – Answers - References REF # 3 2 KEYWORDS QUESTIONS ANSWER Fire Regulation Design Ergonomics Are mobile carts (COW’s, WOW,s, etc.) allowed in the hallway? available for parking the devices to maintain power? Place outlets/network drops at an ergonomic height. Physiological data Monitors Data validation Interface data capture Policy Practice Optimization Should physiologic data imported from monitors be validated before data is it stored in the EMR? Any physiological data imported from monitors into an electronic documentation system must be approved or validated by the nurse prior to its storage in the EMR. Electronic Signature HIPPA Documentatio n Policy Practice How is the electronic signature defined? Issues: Validating that data is correct coming across an interface Ensures clinician evaluation of the data prior to storage and provides the ability to observe trending or to correct technical issues, such as lead artifact or monitor/interface issue. Electronic signature is legal in all 50 States and the security standards of electronic signatures are addressed in the security and privacy provision of the Health Insurance Portability and Accountability Act (HIPAA). REVIEWED BY (TASKFORCE MEMBER) DATA OR EVIDENCE? Brenda Kulhanek Lisa Bove Melissa Barthold Portia Towns Data- Melissa Barthold Brenda Kulhanke Trish Gallagher Lisa Bove Portia Towns Portability and Accountability Act (HIPAA) It can be an electronic sound, symbol, or process associated with a record. It can be an automatic signature added by a system when an entry is saved by the user or it can be an intentional act of signing an electronic document. It is an electronic indicator added to the electronic medical record, including flowsheets, orders, notes, etc. that indicates signature of the licensed provider. It may not require additional Page 2 of 28 REFERENCE/SOURCE Discussion on CARING list CARING list Portability and Accountability Act (HIPAA). http://www.hhs.gov/ocr/priv acy/hipaa/administrative/sta tute/hipaastatutepdf.pdf. DATE Toolbox Questions – Answers - References REF # KEYWORDS QUESTIONS ANSWER REVIEWED BY (TASKFORCE MEMBER) separate action (such as re-entry of a password) – it may be as simple as the act of saving the data entered is the ‘signature’. HIPAA-covered entities that use electronic signatures for transactions must adhere to U.S. Department of Health and Human Services electronic signature standards. The software program must provide: 4 Documentatio n Standards Policy Practice Requirements Design Minimum data sets What should be considered when designing electronic documentatio n? Nonrepudiation - assurance that the signer cannot deny signing the document in the future, User authentication verification of the signer's identity at the time the signature was generated, and Message integrity - certainty that the document has not been altered since it was signed. When making this decision, the following should be considered: Build documentation that reflects standard practice and regulatory requirements. Examples: Minimum data sets from nursing organizations, Joint Commission, CMS and the Bureau of Vital Statistics. Melissa Barthold Brenda Kulhanke Trish Gallagher Lisa Bove Page 3 of 28 DATA OR EVIDENCE? REFERENCE/SOURCE DATE Toolbox Questions – Answers - References REF # KEYWORDS QUESTIONS ANSWER Who is going to view/utilize the data? Only collect data that is used by the care team or regulatory requirements. Purpose of documentation: o Communication among caregivers o Support of billing o Potential for research o Longitudinal record of patient’s health status and treatments Support documentation of assessments and treatments that reflect the standard of patient care as established by local, state and national regulations Guides staff to document the “right things” by preventing documentation of the “wrong things” through proper design Guides staff to document the “right things” by preventing documentation of the “wrong things” through proper design REVIEWED BY (TASKFORCE MEMBER) Suggestions: Documentation Categories: o Assessments o Interventions o Biometric data o Summary/Evaluation data o Progress Notes o Care Plans Page 4 of 28 DATA OR EVIDENCE? REFERENCE/SOURCE DATE Toolbox Questions – Answers - References REF # KEYWORDS QUESTIONS ANSWER REVIEWED BY (TASKFORCE MEMBER) Demographic data Patient education Communication to members of the patient care team o Communication between members of the patient care team Format of documentation o Easily viewed o Supports efficient documentation o Ability to obtain data for reporting (limited free-text fields) o Consider all disciplinesdocumentation needs and access needs o o o 5 What type of format should be used to indicate errors or changed documentatio n? Should the older data be displayed? How is the completed history of data configured? (audit trail) Is this vendor specific? Can it be configured to one standard? CHIT standard? HIM standard? Risk Management? “Error explanations– Page 5 of 28 DATA OR EVIDENCE? REFERENCE/SOURCE DATE Toolbox Questions – Answers - References REF # KEYWORDS 24 6 Devices Device configurations Hardware QUESTIONS changes – how much should be in strikethrough format? Or should it be in that format?” What policies should be addressed prior to electronic documentatio n design/imple mentation? What are the best devices and device configurations that support nursing workflow? ANSWER When making this decision, the following should be considered: Do you support point of care (real-time at the patient’s side) charting? REVIEWED BY (TASKFORCE MEMBER) DATA OR EVIDENCE? REFERENCE/SOURCE DATE Data Melissa Barthold Brenda Kulhanek Jim Cato Lisa Bove Trish Gallagher What applications are currently in use and what are planned? If you are using electronic medication records with bar coding, do you need a place to store individual medications? CARING list Most of the responders have hit on the main device pros and cons. There is no magic device (yet) that does not have some drawbacks, i.e screen visibility, battery life, wall space, hall space, etc. We tried our best to put devices in each room but were limited by the age of the facility and available wall space. Page 6 of 28 Sept 23, 09 Toolbox Questions – Answers - References REF # KEYWORDS QUESTIONS ANSWER REVIEWED BY (TASKFORCE MEMBER) We went live with clin doc in June. In addition to some WOWs and wall mounted devices in the halls from an earlier phase, we added "half-a-roos" with Panasonic One notebook to each double and quad room. Theoretically, this provides the opportunity for point of care charting of I&O, vital signs, etc. in the room with the half-a-roo acting like a small workstation, and also provides the flexibility of removing the notebook to allow staff to sit at the bedside to document longer items, such as an admission or discharge. Space may be an issue. Bedside charting should be an expectation There are many reasons for not doing point of care charting – culture, convenience. Success of beside charting partially depends on how much change enablement the facility wants to apply to this practice. Point of care documentation is not part of the actual IT project; but is part of the nursing work process and is managing by nursing administration. The bottom line, there is no perfect solution. Each facility presents its own challenges. Device Fair and pilot installation of prototypes to allow the staff to have input. Wall-mounted computers in the rooms. It took awhile for all to get use Page 7 of 28 DATA OR EVIDENCE? REFERENCE/SOURCE DATE Toolbox Questions – Answers - References REF # KEYWORDS QUESTIONS ANSWER REVIEWED BY (TASKFORCE MEMBER) to documenting assessments, etc in the room. It may be ideal because if a patient asks about their labs or other test results, we can easily pull it up for them in the room. At the other campuses, we have had a variety, but for med admin bar coding in the room is superior. A bedside PC may be good for many things, such as the admission data base, but should not be the bedside nurses only option. 8 9 10 Charting Real time Point of care Documentatio n Devices What is the best practice for maintaining the power supply on mobile devices? How is the appropriate number of documentatio n devices determined? How is ‘timeliness of charting’ defined?” How is this affected by the constraints of documentatio n technology? When making this decision, the following should be considered: Was there a ‘timeliness of documentation’ policy before automation? Any such policy needs to be reexamined or created prior to implementation of electronic documentation. Melissa Barthold Brenda Kulhanke Trish Gallagher Lisa Bove Has timeliness been defined in other applications such as medication Page 8 of 28 DATA OR EVIDENCE? REFERENCE/SOURCE DATE Toolbox Questions – Answers - References REF # KEYWORDS QUESTIONS ANSWER REVIEWED BY (TASKFORCE MEMBER) administration or ancillary charting? What type of device (WOW, tablet, compute in the room, desktop, etc.) does the user have access to? Generally, prior to automation, ‘timeliness of charting’ was defined by the expectation that the clinician would complete documentation prior to the end of their shift. With automation, the focus has moved to ‘real-time’, although ‘real-time’ can vary based on the type of device that a clinician uses. Late charting has been defined anywhere from 30 minutes (often based on medication administration policies) to 4 hours (batch charting twice a shift). 11 12 Downtime Paper forms Policy Procedures Are ‘default’ answers in forms permitted? How is the scope of default answers determined? What processes are used to document during a computer downtime? However defined, the policy needs to match practice. When making this decision, the following should be considered: Do you allow defaults on paper forms or in other applications? During a downtime, several processes must be considered: 1) How will results be obtained on patients who are currently admitted? Numerous vendors are now selling downtime solutions which reside on stand along PC’s in order to allow providers the ability to continue to review current Melissa Barthold Brenda Kulhanke Trish Gallagher Lisa Bove Jim Cato Page 9 of 28 DATA OR EVIDENCE? REFERENCE/SOURCE DATE Toolbox Questions – Answers - References REF # KEYWORDS QUESTIONS ANSWER REVIEWED BY (TASKFORCE MEMBER) clinical information on patients. If this option does not exist, the development of reports stored on a local PC which are updated automatically at frequent intervals and which can be accessed or printed when the EMR goes down, may be another viable option. 2) How will clinicians continue to document? This is generally accomplished with the use of downtime paper forms. Some organizations will want to revert to old paper documentation but in most cases, from a risk management perspective, the content of the downtime form must be consistent to ensure the same standard of care is provided during downtime. The development of downtime documentation forms are often part of the project scope. 3) Medications – access to an up to date list of the patients current medications along with the last date/time received and when the next dose is due is also imperative documentation during downtime. The generation of downtime MAR’s in order to allow staff to continue to document the administration of medications is necessary. Downtime policy and procedures along with a downtime ‘kit’ containing all the needed paper forms including order sets should be easily accessible on every unit. Also – don’t forget to train staff on downtime procedures during Page 10 of 28 DATA OR EVIDENCE? REFERENCE/SOURCE DATE Toolbox Questions – Answers - References REF # KEYWORDS Downtime Recovery QUESTIONS What data entry recovery and backfill processes are used after a computer downtime? What are the decision making processes to determine what data gathered during a downtime is backfilled into the computer system? What timeframes are used to determine what data is backfilled into the system and when the backfill must be completed? ANSWER the education process. Part of the project implementation should include a multidisciplinary focus group to determine downtime processes based on different types of downtime (ie Network, EMR clinical repository, ancillary systems that are interfaced etc). The main focus in determining what information is entered after a downtime should be centered around ensuring that risk to the patient is minimized after a downtime. It is important to consider: 1. The type of information. Information such as allergies, height and weight for Pharmacy orders and medication information should always be back entered since this is information required for the care of the patient. REVIEWED BY (TASKFORCE MEMBER) Melissa Barthold Brenda Kulhanke Trish Gallagher Lisa Bove Jim Cato 2. Who uses the information? Is the information only used by one ancillary department or is it reviewed by numerous providers to make clinical decicions? 3. How long has the system been down? A downtime which impacts a change in care providers (ie over a shift change) may be handled differently than one that does not. Often a downtime that is 4 hours or less may be handled differently than one which extends longer than 4 hours. Page 11 of 28 DATA OR EVIDENCE? Data REFERENCE/SOURCE DATE Toolbox Questions – Answers - References REF # KEYWORDS QUESTIONS ANSWER REVIEWED BY (TASKFORCE MEMBER) 4. Shat is the impact to it not being available in the EMR? If the patient is readmitted, will the information be valuable to have in the EMR (ie home medications, allergies, history etc)? Is the information related to the medication administration process? This high risk process may need to be handled differently since it involves a higher risk to the patient. 5. What risk exists for the patient if the information is not entered? 6. Is there a mechanism to denote a downtime occurred in the EMR so providers reviewing the information know to reference the paper chart More information has been written about the importance of a standard/ policy regarding how to access data during downtime than about what to document after downtime. Ideally, following a downtime all patient information recorded on paper should be electronically entered so that the EMR is complete and patient care is not compromised. This however is not always practical due to the time required to back chart the data and the issue of who is responsible if the shift changes during downtime. Many hospitals have two standards – one for a short, planned downtime and one for Page 12 of 28 DATA OR EVIDENCE? REFERENCE/SOURCE DATE Toolbox Questions – Answers - References REF # KEYWORDS QUESTIONS ANSWER REVIEWED BY (TASKFORCE MEMBER) DATA OR EVIDENCE? REFERENCE/SOURCE planned or unplanned downtimes lasting longer than 2 – 4 hours. For the short, planned downtimes (less than 4 hours usually), many hospital require that the nurse and/ or pharmacy (depending on the data) back chart the orders, medication administration and clinical documentation. Often for the longerthan-four-hour downtime, no backcharting is done. RECOMMENDATION: If your facility is not back-charting all clinical data regardless of the length of downtime, then make a notation in the electronic chart directing care givers to the paper chart for specific information. 14 Downtime Clinical documentatio n Policies and procedures What is current practice for communicatio n of downtimes to clinical areas? Early, often and as much as possible. Post where ever possible. Login notice, when logging into system Screen saver communication Overhead announcements Email Managers, for posting Page to beeper Potty trainers Melissa Barthold Brenda Kulhanke Trish Gallagher Lisa Bove Jim Cato Never too much! Page 13 of 28 Drazen, Erica, et al. Saving Lives, Saving Money In Practice: Strategies for Computerized Physician Order Entry in Massachusetts Hospitals Massachusetts Technology Collaborative and New England Healthcare Institute January 2009 http://www.nehi.net/pu blications/38/saving_liv es_saving_money_in_pr actice_strategies_for_co mputerized_physician_o rder_entry_in_massachu DATE Toolbox Questions – Answers - References REF # KEYWORDS QUESTIONS ANSWER REVIEWED BY (TASKFORCE MEMBER) DATA OR EVIDENCE? REFERENCE/SOURCE setts_hospitals accessed September 22, 2009 Nelson, Nancy, Downtime procedures for a clinical information system: a critical issue Journal of Critical Care (2007) 22, 45–50 15 combin ed 16 Does charting-byexception support best practice? Is it legally defensible? Charting by exception has been successfully implemented in many organizations. Important considerations: 1. Clearly define normals in documentation policy or in documentation system 2. Clearly define proper charting process and content for abnormals 3. This method of charting cannot be used to document teaching 4. changes in the patient’s condition, while still within the normal range, should be documented 5. Chart on time 6. Charting by exception has been associated with a decrease in nursing charting time of up to 75% 7. Meets JC Standards for individualization of patient care Melissa Barthold Brenda Kulhanke Trish Gallagher Lisa Bove "Ladies & gentlemen of the jury, I present... the nursing documentation".Full Text Available (includes abstract); Austin S; Nursing, 2006 Jan; 36 (1): 56-64 (journal article - case study, CEU, exam questions) ISSN: 0360-4039 PMID: 16395021 CINAHL AN: 2009089387 American Journal of Nursing: March 1999 - Volume 99 Issue 3 - p 24G, 24J (http://journals.lww.com/ajn online/Fulltext/1999/03000/ Charting_by_Exception__A_t imely_format_for_you_.16.a spx) Charting by Exception Applications: Making It Work in Clinical Settings by Laura J. Burke and Judith A. Murphy (Ring-bound - Jan Page 14 of 28 DATE Toolbox Questions – Answers - References REF # KEYWORDS QUESTIONS ANSWER REVIEWED BY (TASKFORCE MEMBER) DATA OR EVIDENCE? REFERENCE/SOURCE 15, 1995) Charting by Exception: A Cost Effective Quality Approach (A Wiley medical publication) by Laura J. Burke and Judy Murphy (Paperback - Oct 19, 1988 Charting by exception: http://allnurses.com/nursing -student-assistance/helpplease-charting-296172.html 17 What is current practice for enhancement request prioritization? How are clinical enhancement requests reviewed? Does the review of clinical enhancement requests include an assessment of the clnical impact of the changes? What is current practice for communicatio Page 15 of 28 DATE Toolbox Questions – Answers - References REF # 18 KEYWORDS Non-licensed EMR documentatio n QUESTIONS n of systemrelated changes, enhancement s? What documentatio n by nonlicensed staff is permitted in the EMR? What is current practice related to RN co-signature of documentatio n entered by non-licensed staff? Is the practice or policy enforced through technology or policy alone? ANSWER Generally, processes that were following in a paper patient chart should be followed in an electronic patient chart. If nonlicensed personnel documented in a paper chart without a cosignature and the practice was within a defined scope of practice, then this same documentation procedure would be appropriate within an electronic patient chart. REVIEWED BY (TASKFORCE MEMBER) Melissa Barthold Brenda Kulhanke Trish Gallagher Lisa Bove Jim Cato If documentation contains information that must be verified and co-signed by licensed personnel, then appropriate means for electronic signature must be configured within the electronic patient chart. There are often attempts to further restrict documentation practices by non-licensed personnel that is within scope of practice by creating electronic co-signatures. However, unless there is a pressing reason to further restrict or monitor the Page 16 of 28 DATA OR EVIDENCE? REFERENCE/SOURCE http://www.fhdeland.org /Portals/27/docs/Stude nt%20Nurse%20Privilg es.pdf DATE Sept 25, 2009 Toolbox Questions – Answers - References REF # KEYWORDS QUESTIONS ANSWER REVIEWED BY (TASKFORCE MEMBER) DATA OR EVIDENCE? REFERENCE/SOURCE documentation of non-licenses personnel, the creation of additional co-signature processes creates an additional burden of documentation for licenses and non-licensed personnel as well. Regular audits of compliance would be recommended, as would audits for all processes transferred to an electronic documentation environment. Examples of non-licensed personnel: Nursing assistants/patient care techs Therapy assistants Students Interns Unit secretaries Any role that documents under the authority of a licensed healthcare provider 19 What is current practice related to managing clinical students’ access to clinical documentatio CARING It seems that typically, prior to the beginning of each semester, the instructor contacts the IT department to assign user names and passwords to the students. The access administrator receives a list of students who will need information from or be entering information into the patients electronic medical record then assigns usernames Page 17 of 28 DATE Toolbox Questions – Answers - References REF # KEYWORDS QUESTIONS n systems? ANSWER REVIEWED BY (TASKFORCE MEMBER) and passwords to the instructor. This access typically has an expiration based upon the end of the clinical course. It is apparently a lot of work to manage all the different clinical students who train in the hospital so some hospitals are assigning username and passwords for the entire time the student is enrolled in their respective nursing school, medical school, rt, pt, ot, etc. Some hospitals give nursing students full security rights as they would have as registered nurses while others restrict their security rights to a student nurse status. Since the primary RN is ultimately responsible for the evaluation of and documentation for the patient it must be the primary RN who co-signs the medical record data as true and correct (there are numerous ways to do this and it typically is dictated by policy). The instructor is not able to follow every student into every room and watch their every action thus confirming that what is charted is true and accurate. DATA OR EVIDENCE? Data The ever more careful scrutiny of the patient’s medical record creates additional opportunities and challenges with documentation, especially when nursing students and faculty are involved in providing elements of nursing care. The specifics of documentation policies need to be developed within each institution. Some points to consider Page 18 of 28 REFERENCE/SOURCE CARING DATE 9-11-09 Toolbox Questions – Answers - References REF # KEYWORDS QUESTIONS ANSWER REVIEWED BY (TASKFORCE MEMBER) include: ♦ As a novice practitioner, a student nurse's observations are subject to careful review. A licensed nurse needs to be aware of what the student charted. The facility nursing staff is ultimately responsible for reassessment if documentation is in question. ♦ The patient record must provide for traceability of care givers. This may become especially challenging when several schools of nursing utilize the same facility and a caregiver only identified as “SN” could come from one of several schools. It is suggested that as a minimum, students document their name, student status and school if more than one school uses the facility. For example a student could sign the record "Susan J.Nurse, SN, Worlds Best College" ♦ The term “co-sign” is subject to misinterpretation. Documentation must clearly reflect if a “co-signer” is verifying the accuracy of students’ charting or only verifying that they have reviewed the charting. ♦ A "co-signer" should not change the original student entry unless the record reflects that the change was made by another party. ♦ If the facility policy requires documentation that the student charting was reviewed suggested formats for charting may include: • A faculty member signs the record Page 19 of 28 DATA OR EVIDENCE? REFERENCE/SOURCE DATE Toolbox Questions – Answers - References REF # KEYWORDS QUESTIONS ANSWER REVIEWED BY (TASKFORCE MEMBER) "WB Teacher, RN, MSN (oversight signature)" • A staff nurse signs "Charting reviewed by WB Nurse, RN, MSN" (http://drl.wi.gov/boards/nur/pap/pap1 8.pdf) Students have an log in number for the school that is different then their employee number. Their log in ID gives them more of a limited access then it would if they were a nurse on the floor. There is no co-signature requirement for students’ assessments that are documented in the computers. The instructors review the documentation that the students put into the computer charting, however we feel that to co-sign the students’ documentation would mean that we – the instructors - have done that assessment on that patient and often that is not the case. Our clinical instructors have up to 8 students and they may have up to three patients. We could not possibly do all of those assessment plus give medications and oversee new skills. We do co-sign medication administration because we are with them when they give medications to their patients. 20 How is the future state included in Page 20 of 28 DATA OR EVIDENCE? REFERENCE/SOURCE DATE Toolbox Questions – Answers - References REF # 21 KEYWORDS QUESTIONS ANSWER REVIEWED BY (TASKFORCE MEMBER) the planning and execution of current implementatio ns or enhancement s? How are technology decisions analyzed that may negatively impact future enhancement s/building? How are decisions made when an urgent need is addressed in a future enhancement that is not an organizational priority? What is the current best practice window for future technology planning? What is current practice for training staff. What is the current practice for Page 21 of 28 DATA OR EVIDENCE? REFERENCE/SOURCE DATE Toolbox Questions – Answers - References REF # KEYWORDS 22 Portia 23 Jim 24 25 26 QUESTIONS ANSWER REVIEWED BY (TASKFORCE MEMBER) training and utilizing SuperUsers? How are SuperUsers best utilized as a resource? What QA is necessary for electronic systems? Who should do QA? How is standardizatio n of practice documentatio n analyzed, implemented and measured? What is the current state of EHR use in mental health? How are ancillary departments trained to use the EHR? What is the best practice for use of computer protective equipment such as Page 22 of 28 DATA OR EVIDENCE? REFERENCE/SOURCE DATE Toolbox Questions – Answers - References REF # 27 KEYWORDS Change management Change QUESTIONS keyboard covers, and computer cleaning for computers used in patient care areas What is the best way to plan and manage ongoing change between IT and the clinical areas? ANSWER Simple Answer: The best way to plan and manage ongoing change between IT and Clinical Areas is to have an IT Adoption Methodology that promotes change management along with a supportive organizational culture. Six key principles of effective, sustainable change management include: (See Graphic) 1. Need for Change – the need for change (“Why?”) needs to be clearly articulated, documented and communicated. Without a need for change there will not be any action 2. Shared Vision – often times organizations function in disparate, departmental silo’s. Having a common/shared vision for where the organization is headed is a key success factor to effective Change Management. Without a shared vision there will be a “fast start that fizzles” as other competing priorities take over. 3. Leadership Commitment – the organizations entire leadership team (not just certain individuals) must be committed to the change. Anxiety and frustration will result without a unified leadership team to drive the change. 4. Employee REVIEWED BY (TASKFORCE MEMBER) Mark DATA OR EVIDENCE? Data Page 23 of 28 REFERENCE/SOURCE Multiple documents DATE 9-4-09 Toolbox Questions – Answers - References REF # 28 29 KEYWORDS QUESTIONS How is emergency access to the HIS available? ANSWER Involvement/Commitment – employees will be resistant to any change that they feel has been forced upon them. Early involvement of employees and a demonstrated commitment to change is essential 5. Integrated Organizational Change – invariably a change in one area of the organization will trigger a change in another. Integrating change across departmental prevents a “siloed” view of the change. 6. Performance Measures – one of the most commonly overlooked principles of effective change management is documentation of results through key performance indicators. Without performance measures in place there will be no measurable results to sustain the change. For staff members, such as those from Organ Procurement provided 2/47? Identify staff who may be using the system. Preferred: Create logins for all agency staff members. Create one ID for each agency and require a member to call the help desk, where the date/time/name of the staff member is recorded prior to issuing a password. The password expires in a defined time frame. REVIEWED BY (TASKFORCE MEMBER) Melissa Barthold Brenda Kulhanke Trish Gallagher Lisa Bove how you manage sound on computers in your hospital DATA OR EVIDENCE? REFERENCE/SOURCE data 8-14-09 CARING list Page 24 of 28 DATE 8-18-09 Toolbox Questions – Answers - References REF # 30 KEYWORDS CPOE Order sets Orders QUESTIONS setting. We are having discussions about enabling sound on select devices where possible for nursing and patient education (products like Elsevier, etc). How do your hospitals handle staff and patient education? Do you have sound-enabled devices at certain locations? If so, how is your patient education material approved? Do you have sound at devices in nursing stations How are CPOE order sets best created? ANSWER REVIEWED BY (TASKFORCE MEMBER) Like most things in our increasingly complex lives - one size doesn’t fit all for CPOE implementation. There are significant differences between critical access hospitals vs regional hospitals vs tertiary care facilities. Vertically integrated systems have different issues than do horizontal systems. Below, I provide some recommendations: DATA OR EVIDENCE? Data Page 25 of 28 REFERENCE/SOURCE Caring List DATE 8-7-09 Toolbox Questions – Answers - References REF # KEYWORDS QUESTIONS ANSWER REVIEWED BY (TASKFORCE MEMBER) 1) Situational Awareness theory says that the more you automate a process - the less aware you become of the process being automated. There can be an increased incidence of providers becoming reliant on the orderset to guide their decision making verses facilitating their decision making. Make sure your ordersets are clear, unambiguous and provide sufficient ability for choice - without making it too broad or too restrictive. 2) Study, study, study. Make sure you understand how the organization and all its parts work - and why. The more you know - the more you can produce competent tools and drive change. 3) Standardize, standardize, standardize. Use a style guide that defines what words mean, where orders are found, in what order they appear, how they are name etc. Ordersets should be predictable - so that regardless of the clinical situation, providers can order safely and efficiently. 4) Know the technology - what it can do and can not do. 5) Test, test, test. Do exhaustive testing with complicated and high-risk workflows, like: blood transfusion, titrations, pre-ops and oncalls, sedation, lab based admins etc Page 26 of 28 DATA OR EVIDENCE? REFERENCE/SOURCE DATE Toolbox Questions – Answers - References REF # KEYWORDS QUESTIONS ANSWER REVIEWED BY (TASKFORCE MEMBER) DATA OR EVIDENCE? REFERENCE/SOURCE DATE 6) Ordersets and CPOE isnt just about physicians! The order/orderset must meet physician workflow AND the departments that complete them. 31 CPOE Nursing Process How are telephone or verbal orders handled in a CPOE environment? 7) Confusing or error prone paper based work flows make confusing and error prone CPOE workflows. Fix policy and workflow BEFORE going live with CPOE. No policy for telephone orders, the mandatory use of CPOE is in the orientation for the medical staff as well as the nursing staff. Connie Whittington Our workflow for this is as follows: 1. All orders are in CPOE - no exceptions 2. No verbal orders are taken for CPOE unless in an emergent situation with all hands needed on patient 3. no phone orders except in following case: a. RN calls with abnormal test result or patient care need and patient needs treatment related to this b. MD is in transit from one place to another and cannot access computer - no more than 6 orders is our guideline on this, just enough to get patient care initiated. Note that MD MUST remain on phone while RN is entering the orders so that they can reply to any alerts the RN encounters when entering orders c. if verbal orders are requested, we ask that pathway orders or order sets be accessed as orders are prechecked and RN can read the orders off to MD with rare/few changes Page 27 of 28 Oct 13-09 Toolbox Questions – Answers - References Page 28 of 28