methods - European Respiratory Journal
advertisement

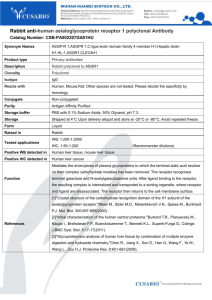
METHODS Subjects Sixteen mild asthmatic subjects were screened for this study and twelve went on to complete bronchial provocation challenge with AMP and bronchoscopy. All subjects had mild asthma (forced expiratory volume in 1 second (FEV1) > 70% of predicted) and a history of atopy. Each subject had infrequent symptoms, controlled with occasional inhaled short-acting ß2-agonists alone. No subject was taking any regular anti-asthma therapy and none had taken inhaled corticosteroids for at least 3 months prior to entry. None of the subjects had an exacerbation of asthma or respiratory infection in the preceding 6 weeks and all subjects were non-smokers. demographics are summarised in Table I. Patient For comparison, biopsies from eight healthy age-matched non-smoking subjects obtained in a separate but recent previous study under the same conditions were also analysed. The demographics from these subjects are described in Table 1. Written informed consent was obtained from each subject and the study was approved by the Ethics Committee of King's College Hospital. Study design Procedures at Visit 1 for all subjects included medical history and physical examination, an asthma characterisation questionaire, intradermal skin prick tests, spirometry and methacholine challenge to determine provocative concentration (PC)20 values. After approximately 1 week, asthmatic subjects returned for Visit 2 where they underwent AMP challenge to determine the PC20 to AMP. All subjects refrained from using rescue medication and caffeinated beverages for at least 8 hours before each visit. After a period of 3-4 weeks, all subjects returned for Visit 3 at which bronchoscopy was performed. Intradermal Skin Prick Tests Stock solutions of allergen extract (10,000 U/ml) for Dermatophagoides pteronyssinus, mixed grass pollen or cat dander (ALK Abello, Horsholm, Denmark) and saline control were applied intradermally to the volar aspect of the forearm. The wheal and flare response was measured after 15 minutes and results recorded. A skin response greater than 3 mm in comparison to saline control was considered to be a positive reaction. Bronchial provocation challenge with AMP/methacholine and pulmonary function measurement On each challenge day a fresh stock solution of 800 mg ml-1 AMP (Sigma Biochemicals, Poole, U.K) was prepared using 0.9% saline as a diluent. Doubling dilutions from 800 mg ml-1 to 0.39 mg ml-1 were then prepared by sequential 2-fold dilution with saline. In a similar manner a fresh solution of 32 mg ml-1 methacholine (Sigma Biochemicals, Poole, U.K) was made up in 0.9% saline and doubling dilutions from 32 mg ml-1 to 0.0625 mg ml-1 were prepared. Each solution was administered from a hand-held nebuliser attached to a breathactivated dosimeter (Mefar, Brescia, Italy) with a delivery time of 1s per breath. The nebuliser delivers particles with an aerodynamic mass median diameter of 3.5-4.0 m and an output of 14 l per breath. Spirometry was assessed by measurement of FEV1 with a dry wedge spirometer (Vitalograph, Buckingham, U.K.). A standard protocol was followed for all AMP/methacholine provocational challenges. Following a 15minute rest period, subjects wearing a nose-clip, performed three FEV1 measurements one minute apart, the best of which was taken as baseline. Subjects then inhaled 5 breaths of saline as a control with an inhalation time of one second from functional residual capacity (FRC) to total lung capacity (TLC) and a breath-hold time of 6 seconds. Provided FEV1 remained within 10% baseline, subjects continued by inhaling 5 breaths of the lowest concentration of AMP/methacholine followed by doubling increments, at 3-minute intervals. FEV1 was measured at 1.5 and 2.5 minute intervals following inhalation of each of each dilution and the highest value was recorded for analysis. Challenges were terminated when at least a 20% fall in FEV 1 from post-saline was recorded or the maximum concentration had been given. A logarithmic concentration-response curve was conducted and the PC20 calculated by linear interpolation. Fiberoptic bronchoscopy All subjects underwent bronchoscopy in the same manner. Supplemental nasal oxygenation and intravenous sedation with alfentanil (0.2-1 mg) (Janssen-Cilag Ltd, High Wycombe, U.K.) and midazolam (1-10 mg) (CP Pharmaceuticals, Wrexham, U.K.) was given to each subject. Topical anaesthesia was achieved with the application of 4% lignocaine (Astra-Zeneca, Sweden) to the nasal passages, pharynx, vocal chords and trachea followed by 2% lignocaine to the carina, right main bronchus and right middle lobe and lower lobe bronchi. The bronchoscope was passed transnasally or orally with the subject at 45 degrees. Following inspection of the airways and administration of any additional topical anaesthetic (lignocaine gel, Bio-rex, Enfield, U.K.) to control cough, biopsies were taken under direct bronchoscopic vision from the right middle, upper and lower lobe segmental and/or subsegmental carinae. Immunohistochemistry Using the methods described below to validate the adenosine receptor subtype specificity of an antibody, we found that the specificity of commercially available antibodies against all adenosine receptor subtypes was unsatisfactory, hence an antibody against the adenosine A1 receptor was created specifically for the present study (the costs involved in obtaining a custom-made antibody was also a contributing factor when deciding not to concurrently profile expression of the other adenosine receptor subtypes). Thus, the custom-made affinity purified A1 receptor polyclonal antibody was raised in the rabbit against a synthetic peptide corresponding to the amino acid sequence 309-326 (CQPAPPIDEDLPEERPDD) of the COOH-terminus of the human A1 receptor (Cambridge Research Biochemicals, Cleveland, U.K.). Biopsies were lightly fixed in 4% paraformaldehyde for 1-2 hours and then cryoprotected in 15% w/v sucrose solution overnight at 4ºC. Biopsies were then embedded in Optimal Cutting Temperature Compound (OCT, Agar Scientific Ltd, Stansted, U.K.), snap frozen in isopentane cooled by immersion in dry ice and then stored at -80ºC until required for sectioning. In addition to immunohistochemical analysis of healthy and asthmatic bronchial biopsies with the A1 receptor antibody, brain and cardiac tissue sections were concurrently analysed as a positive control, as it is well established that these tissues highly express A1 receptors. Cadaveric brain cortex and cardiac tissue samples were obtained from the Institute of Psychiatry Brain Bank and Peterborough Tissue Bank respectively, following GlaxoSmithKline and United Kingdom guidelines for the acquisition and use of human tissues, including ethical approval and the use of appropriate consent forms. Brain cortex and cardiac tissue biopsies from a total of 3 subjects were analysed. A Shandon cryotome cryostat was used to section biopsies at 6 µm. Sections were placed on Vectabond™ (Vector Laboratories, Peterborough, UK) coated slides and the brain cortex and cardiac tissue sections post-fixed in ice-cold 4% w/v paraformaldehyde. Sections were then immunostained for the A1 receptor using an Optimax automatic immunostaining machine (Biogenex, San Ramon, CA, USA). In summary, non-specific protein staining was blocked by treatment with Power Block™ prior to incubation with the A1 receptor antibody (1 µg ml-1) or rabbit IgG isotype control antibody (1 μg ml-1) at room temperature for 1 hour. After primary antibody incubation, sections were then incubated with a goat anti-rabbit secondary antibody labelled with horseradish peroxidase-streptavidin and positive staining detected with diaminobenzidine. With the exception of the adenosine A1 receptor antibody, all immunohistochemistry antibodies and substrates were obtained from Vector Laboratories, Peterborough, U.K. The sections were also counterstained with Mayer’s haematoxylin (Pioneer Research Chemicals Ltd, Colchester, U.K.). Image analysis Fully automated densitometry of A1 receptor expression was developed with the Zeisss Vision KS400 system (Carl Zeiss, Gottingen, Germany). After a 30-minute warming up of the microscope (X1000 magnification) the images were digitised with a three-chip colour camera, which was connected to a personal computer with a 2.66 GHz Pentium 4 processor and frame grabber with appropriate corrections for nonuniform illumination (shading correction) and settings of the black and white camera signal (white balance). Descriptive data for each compounded image were stored in a corresponding image database. The image processing was based on the red-greenblue (RGB) colour model. Custom macros were written in KS300 interpreter language to separate the brown-red staining from the blue counter-stain. Four images from each endobronchial biopsy section (1 section per subject) were randomly selected in epithelial and smooth muscle regions. Positive staining colour intensity data were stored in a corresponding database. Stain intensity was described in arbitrary units (A.U.). All image analysis and measurements were performed blind by one observer. Antibody validation-generation of adenosine receptor transfectant cells In addition to immunohistochemical analysis of brain and cardiac tissue, further antibody validation experiments were to be performed through comparing the binding of the A1 receptor antibody to each adenosine receptor subtype expressed on Chinese hamster ovary (CHO)-K1 cells (which lack any known subtype of adenosine receptor) transfected with the human recombinant A1, A2A, A2B or A3 receptor. These cell lines were also to be used in a separate study and so for that purpose, were first stably transfected with a reporter plasmid designated CRE-SPAP-Hyg. For this reason, hygromycin B was present in the medium. Therefore, in order to further transfect the CRE-SPAP-Hyg host with the human recombinant A1, A2A, A2B or A3 receptor, the host cells were cultured to 50% confluence in 6-well 9cm2 plates in M1 medium (Dulbecco's modified Eagle's medium/Hams F-12 (1:1) mix (Sigma Biochemicals, Poole, U.K) supplemented with 2 mM Glutamax, 10% foetal calf serum) containing 500 µg ml-1 hygromycin B (all Gibco, Paisley, U.K.). Cultures were maintained at 37°C in a 5% CO2/humidified air atmosphere). The cells were then washed twice in DMEM/Ham’s F-12 and left in the same medium for 3-4 hours. Each DNA construct was linearised with SspI in Boerhinger Buffer H, and then sterilised with Phenol:Chloroform:Isoamyl alcohol (PCI) (25:24:1) and washed in CI (24:1) using phase lock tubes (CP laboratories, Saffron Walden, U.K.). 8 µl of each construct was placed in a sterile microcentrifuge tube with 42 µl of DOTAP (Roche Diagnostics, Lewes, U.K.):Hepes buffered saline (HBS) (300:950). After very gentle mixing, the tubes were left for 15 minutes at room temperature. While the tubes were incubating, most of the medium on the cells was removed to leave to 1 ml. Each DNA construct was then added to one well. The cells were incubated for 5 hours after which time 3ml of M1 medium containing 500 µg ml-1 hygromycin B was added. The cells were then incubated for 24 hr before each well before applying further selection pressure. After this period the cells were passaged into M1 and 500 µg ml-1 hygromycin B and 1 mg ml-1 G418. The cells transfected with the A1 receptor were scaled up in 175 cm2 and then 500 cm2 flasks. The expression level of the receptor within this pool remained consistent over several months as judged by flow cytometric analysis of the HA tag on the N-terminus of the receptor. The cells transfected with the A 2A, A2B or A3 receptor did not have an HA tag. These recombinants were cloned as follows: The transfected cells were passaged and diluted and plated into microtitre plates at 0.3 and 1 cell per well. The medium was changed after 5 days. After 10-12 days selection pressure, wells under the microscope that had 1 colony per well were identified. These were maintained until confluent and then scaled up into 9 cm2 wells. Once confluent 90% of the cells were passaged off, spun down and made into small membrane preparations to identify high expressors via binding assays (data not shown). Those identified as such were scaled up further into 175 cm2 or 500 cm2 flasks for banking. For experiments, all the cell lines were cultured with M1 medium supplemented with 500 µg ml-1 hygromycin B and 500 µg ml-1 G418 and harvested when approximately 70% confluent. Extraction of total RNA In order to compare expression of the transfected receptor, total RNA was purified from the cell preparations using a RNeasy midi kit (Qiagen, U.K.) according to the manufacturer’s instructions. The RNA was then dissolved in nuclease free water and quantified using a spectrophotometer, the quality of RNA was assessed by running the samples in an agarose gel (1%). Reverse transcription and specific amplification by Polymerase Chain Reaction (PCR) cDNA was generated from 1µg of total RNA per sample using a SuperScript FirstStrand Synthesis System for RT-PCR kit (Invitrogen, Paisley, U.K.) according to the manufacturer’s instructions. The samples were directly amplified by quantitative real-time RT-PCR using a 7900HT Sequence Detector (Applied Biosystems, Warrington, U.K.). Primer pairs (Sigma Genosys Haverhill, U.K.) and internal probe sequences (Applied Biosystems, Warrington, U.K) are described in Table II. DNA contamination of RNA samples was checked for by including samples to which no reverse transcriptase had been added. The resulting data were analysed using the sequence detector system software (Applied Biosystems, Warrington, U.K.) with TAMRA as the reference dye. Data are expressed as gene copy number per 50 ng cDNA. Flow cytometry A comparison of the A1 receptor antibody binding to the A1, A2A, A2B and A3 receptors expressed on the transfected CHO-K1 cells was performed by using flow cytometric analysis. Cells were cultured as described above until approximately 70% confluent and then fixed and permeabilised using Fix and Perm® (Caltag Laboratories, Burlingame, CA, USA), according to the manufacturer’s instructions (1 x 105 cells per sample). Cells were then incubated at room temperature with the 1 µg of the A 1 receptor antibody in 100 µl or pre-immune serum for 15 min. Cells were washed with PBS containing 3% heat-inactivated foetal calf serum and incubated at room temperature with an R-phycoerythrin (PE)-conjugated goat anti-rabbit polyclonal antibody (2 µg per sample) (Sigma Biochemicals, Poole, U.K) for a further 15 min. After washing, cells were finally resuspended in Cell Fix™ (BD Biosciences, Erembodegem, Belgium) and analyzed by appropriate gating for immunofluorescence using a FACS Calibur flow cytometer (Beckton Dickinson, Oxford, U.K.) after excitation at 488 nm. At least 3,000 events were collected and mean fluorescence intensity values recorded. Values obtained following labelling with the A1 receptor antibody were corrected for non-specific staining with values obtained with control cells incubated with pre-immune serum. Statistical analysis Data were analysed by unpaired Student’s t-test, and unless stated otherwise, are expressed as mean standard error of the mean (SEM). Table II Primer pairs and internal probe sequences for human adenosine receptors Gene Sequences A1 receptor Sense Antisense Probe 5’-CTGCCTTTGCACATCCTCAAC-3’ 5’-GATGGCAATGTAGGTAAGGATGCT-3’ FAM-TGCCCGTCCTGCCACAAGCC A2A receptor Sense Antisense Probe 5’-GGGTGTCTATTTGCGGATCTTC-3’ 5’-CAGAGGCTGGCTCTCCATCT-3’ FAM-CGGCGCGACGACAGCTGAAG A2B receptor Sense Antisense Probe 5’-GAACCGAGACTTCCGCTACACTT-3’ 3’-CCTGACCATTCCCACTCTTGA-3’ FAM-TCACAAAATTATCTCCAGGTATCTTCTCTGCCAA A3 receptor Sense Antisense Probe 5’-TTCGGAACAAACTCAGTCTGAACT-3’ 5’-AACAAGGACTTAGCCGTCTTGAAC-3’ FAM-CAAAGAGACAGGTGCATTTTATGGACGGG
![Shark Electrosense: physiology and circuit model []](http://s2.studylib.net/store/data/005306781_1-34d5e86294a52e9275a69716495e2e51-300x300.png)