Somatization
advertisement
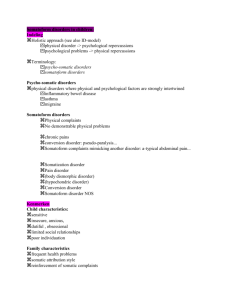
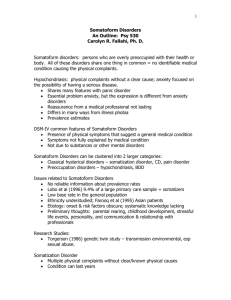
SOMATIZATION DISORDER William Becker, M.D. WEEK 17 Learning Objectives: 1. Appreciate when to suspect the diagnosis of a somatoform disorder 2. Know the criteria for diagnosis of somatization 3. Understand therapeutic options for treatment of somatization/medically unexplained symptoms CASE ONE: Ms. Iva Mani Paine is a 42-year-old female you are seeing in clinic for hospital follow-up. She had been admitted for ‘intractable nausea and vomiting’ and dehydration after presenting to the ED complaining of general malaise, abdominal pain, decreased oral intake, nausea, vomiting, and diarrhea for 10 days. While in the hospital on a private physician’s service, Ms. Paine underwent abdominal x-ray, right upper quadrant ultrasound, EGD and colonoscopy, all of which were normal, as were her amylase/lipase, chemistries, LFTs, CBCs, and stool studies. She was discharged with a diagnosis of ‘viral gastroenteritis’ one week ago, but the patient says that she does not feel any better. Ms Paine reports ongoing crampy abdominal pain, a bloated sensation after eating, blood and mucus in her stool, and a 12-pound weight loss over the past month, which has led her to shift almost all of her childcare responsibilities to her husband. She is taking PRN oxycodone prescribed by her previous internist for the abdominal pain without much relief. In fact, nothing makes the pain better or worse; the patient reveals that, to her, this proves that she is ‘dying.’ It is unclear whether she was discharged from the previous practice or whether she switched voluntarily; in any case, the patient tells you that she wants you to be her doctor because “you are my only hope.” Questions: 1. What are some of the features of Ms. Paine’s presentation that suggest the diagnosis of somatization? What further information do you need to confirm (or reject) the diagnosis? From what we can tell so far, the patient has somatic complaints that have no medical explanation; this is the cardinal feature of somatization. Furthermore, she seems to have an irrational anxiety about her illness that persists despite reassuring findings. Her normal daily activities are significantly compromised, and she is seeking treatment, two other criteria for diagnosis. At this point, obtaining a complete review of systems and past medical history is required. It should be recognized that there might be a temptation to limit these questions due to time-constraints and negative countertransference towards somatisizing patients; nonetheless, the importance of making the diagnosis requires a thorough approach. Also, of note, excluding depression is not required to make a diagnosis of somatization; in fact, most experts believe co-occurrence of the two disorders approaches 50%. CASE ONE CONTINUED: Probing her past medical history reveals dysmenorrhea with menorrhagia including two dilations and curettages and a vaginal hysterectomy at age 28. Also, seronegative arthritis with normal ESR since her 20s, untreated “thyroid problems (normal TSH during admission),” negative exploratory laparotomy one year ago for similar presentation resulting in resolution of symptoms for several months, intractable vomiting throughout all three pregnancies Allergies: Erythromycin, codeine, PCN, lactose, latex, peanuts Social History: Unemployed since first episode of abdominal pain one year ago. High school graduate. Three children, married for 20 years, negative domestic violence screen. Former smoker, quit at first pregnancy; no alcohol, drugs. Family History: Unrevealing. Review of Systems: Weekly tension headaches, back, hip, knee pain. Heart palpitations, weakness, dry skin, shortness of breath, numbness and tingling of all 4 extremities, difficulty swallowing, fatigue, vaginal dryness, dyspareunia, amnesia for one week eight months ago. Physical exam notable for normal vital signs and an otherwise normal exam except for diffusely tender abdomen with hysterectomy, laparotomy scars (no rebound or rigidity, heme negative rectal exam) and decreased pinprick sensation in right arm. Mental status exam reveals a well-developed woman in no acute distress. Pleasant, cooperative, alert/oriented with good eye contact. She is dressed in pajamas from home. Mood is described as “Fair;” affect displays full emotional range. Thought process is logical; content remarkable for multiple somatic complaints and preoccupation with their implications. No suicidal/homicidal ideation, hallucinations. Average intelligence, fair judgment. Insight is minimal. 2. Can you make the diagnosis of somatization now? What are the other somatoform disorders, and how are they distinguished from somatization? Yes. As stated above, patient has preoccupation with medically unexplained symptoms that has led to significant decline in function and increased use of medical resources. Other criteria now fulfilled include: a persistence of complaints over several years starting before the age of 30, as well as, at least four pain symptoms, two gastrointestinal symptoms, one sexual symptom, and one pseudoneurologic symptom. The other somatoform disorders include factitious disorder, malingering, conversion disorder, pain disorder, hypochondriasis, body dysmorphic disorder, and undifferentiated somatoform disorder. The decision-tree from DSM-IV (included) shows a straightforward algorithm for differentiating these disorders. N.B. – though the criteria for diagnosing somatoform disorders are often the subject of ABIM certification-exam questions, their utility for primary care practice is questioned by some authors. RC Smith, among others, places an emphasis on the term “medically-unexplained symptoms” or MUS to broadly encompass most of the somatoform disorders and to emphasize the uniform approach to treatment of them. 3. Using Smith and colleagues’ review article, please discuss potential approaches for the treatment of Ms. Paine. Specific issues to consider include the following: appropriate treatment modalities for the primary care setting, frequency of visits, labeling of illness, use of narcotics, use of antidepressants, and referral to other specialists. The backbone of Smith et al’s approach involves a patient-centered method of communication listed in Table 1 (p. 480) that relies on open-ended questioning and the development of an emotional context for the physical symptoms, as well as provider support for those emotions. The more specific “cognitive behavioral treatment plan” offers specific evidence-based modalities for changing the patient’s “explanatory model” of his/her disease to one that is less likely to lead to maladaptive behaviors. Table 2 (p.482) highlights specific points that may affect this change. Of note, Smith et al. recommend providing a diagnosis for the patient that has a somatic basis (e.g. chronic muscle strain, or even recognized diagnoses – fibromyalgia, irritable bowel syndrome) but simultaneously maintaining a greater emphasis on the interaction of depression and anxiety with the somatic component. Medical therapy should target affective disorders; opioids should be tapered and discontinued whenever possible. Frequency of visits is a less important issue than maintaining efforts to make each visit productive. To this end, Smith et al. offer two other tenets of management: obtaining an explicit commitment, even a contract, from the patient to follow a specific treatment regimen and negotiating the details of that regimen. Table 3 (p.483) is menu of evidence-based treatment options that providers may use. Smith et al. argue the effectiveness of their approach for primary care providers, though a team-oriented approach enlisting the support of a case manager, nutritionist, physical therapist, social worker, etc. may also be effective. Any patient with whom the primary care provider cannot achieve a therapeutic alliance after several visits or any patient with co-occurring serious mental illness or substance abuse should be referred to a psychiatrist. References: 1. Smith, RC et al. Treating patients with medically unexplained symptoms in primary care. JGIM 2003;18:478-489. 2. Differential diagnosis of somatoform disorders. DSM IV-TR. 2000. American Psychiatric Association Press. 756-57. Additional References: 1. McWhinney, IR et al. Rethinking somatization. Ann Intern Med. 1997; 126: 747750.