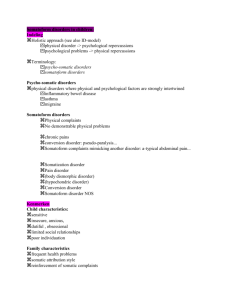
Somatoform Disorders
advertisement

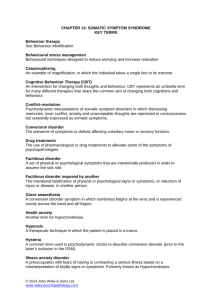
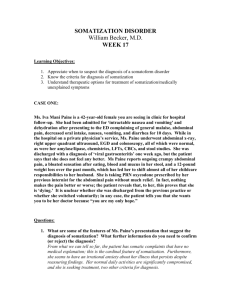
1 Somatoform Disorders An Outline: Psy 530 Carolyn R. Fallahi, Ph. D. Somatoform disorders: persons who are overly preoccupied with their health or body. All of these disorders share one thing in common = no identifiable medical condition causing the physical complaints. Hypochondriasis: physical complaints without a clear cause; anxiety focused on the possibility of having a serious disease. Shares many features with panic disorder Essential problem anxiety, but the expression is different from anxiety disorders Reassurance from a medical professional not lasting Differs in many ways from illness phobia Prevalence estimates DSM-IV common features of Somatoform Disorders Presence of physical symptoms that suggest a general medical condition Symptoms not fully explained by medical condition Not due to substances or other mental disorders Somatoform Disorders can be clustered into 2 larger categories: Classical hysterical disorders – somatization disorder, CD, pain disorder Preoccupation disorders – hypochondriasis, BDD Issues related to Somatoform Disorders No reliable information about prevalence rates Lobo et al (1996) 9.4% of a large primary care sample = somatizers Low base rate in the general population Ethnicity understudied; Farooq et al (1995) Asian patients Etiology: onset & risk factors obscure; systematic knowledge lacking Preliminary thoughts: parental rearing, childhood development, stressful life events, personality, and communication & relationship with professionals Research Studies: Torgerson (1986) genetic twin study – transmission environmental, esp sexual abuse. Somatization Disorder Multiple physical complaints without clear/known physical causes Condition can last years 2 4 pain symptoms (back, abdomen, joints) 2 gastrointestinal symptoms (diarrhea, food intolerance) 1 sexual symptom (irregular menses, indifference to sexual activity) 1 pseudoneurological symptom (poor balance, numbness, paralysis) before the age of 30 frequent and multiple medical consultations alters the person’s lifestyle full-blown somatization disorder rare - .2% men; .2 to 2.0% women; lifetime 0.1% in general population. Historical explanations: ancient Greeks – wandering uterus; 19th C Briquet polysymptomatic somatic condition = Briquet’s syndrome; Guze & Perley (1963) “somatization disorder”. Contemporary Thoughts: small subset of patients; functional symptoms; what happens? Somatosensory amplification Maintenance of the disorder Prognosis Conversion Disorder Symptoms look neurological, e.g. glove anesthesia. 4 subtypes: motor symptoms or deficits; seizures or convulsions; sensory symptoms or deficits; mixed presentation important requirement: temporal relation between symptoms & psychological stressor. Distress or la belle indifference Prevalence unknown, but estimates .001 and .3% population. Historical explanations: “neuroses”; Charcot & hysterical conversions under hypnosis; defense mechanisms; Freud’s explanation. Contemporary Theories: Ullman & Krasner (1975) learned via behaviorism; Folks, Ford, & Regan (1984) sociocultural influences; Kellner (1991) neurophysiological studies show patients with CD do not habituate in the same ways as other patients; the role of emotional arousal. Onset late childhood or early adulthood. Grief & sexual trauma often involved. Mace & Trimble (1996) 10 year follow-up. Pain Disorder Severe acute or chronic pain in one or more body parts is not entirely or adequately explained by a known medical condition Psychological factors involved. Acute versus chronic Prevalence unknown – relatively common Historical explanations: Aristotle; Descartes; Epicetus; Religious leaders; unidimensionality of pain. 3 After 20th C, integrated explanations that were organic & psychological. Fordyce (1976) behaviorist explanations Cognitive-behavioral explanations. High frequency trauma & personality disturbance. Engle (1959) pain-prone personality Occupational factors important Hypochondriasis: unjustified fears or convictions that one has a serious/fatal illness. 6 months & not of delusional intensity 3 to 14% medical patients (Kenyon, 1976); 16% general population illness phobia (Agras et al, 1969); 10% general practice (Palson, 1988); patients with increased exposure to medical settings Historical explanations: “Below the cartilage” – excess of black bile; 17thC Thomas Sydenham = equivalent to hysteria; Freud Contemporary Theories: behavioral theories; learned disorder; cognitive explanations; somatosensory amplification. Chronic condition. Children’s symptoms versus adult’s symptoms. Sexual trauma Body Dysmorphic Disorder Preoccupation with an imagined or exaggerated body disfigurement/excessive concern that there is something wrong with the shape/appearance of body parts. Examples. Cognitive features. Typical behaviors. Prevalence unknown, but…. Rosen (1995) & Connolly & Gipson (1978) Not equal to unhappiness about one’s appearance. Historical explanations: 19th C Enrico Morselli – sudden onset & persistence of an idea that the body is deformed with severe anxiety. Morselli – obsessive nature. Recent views = no to phobic anxiety. Core problem: perception of abnormality. Contemporary theories: Rosen (1995) cognitive-behavioral explanation. Gradual / sudden onset; course continuous & chronic. Only anecdotal evidence. Beings in adolescence. Sociocultural factors. Perfectioinstic features. Factitious Disorder Physical symptoms produced or feigned intentionally to assume the sick role. 4 Eager to undergo extensive medical procedures. Pathological compulsion to deceive medical professionals = pseudologia phantastica. Different from malingering. Munchhausen Syndrome; munchhausen-by-proxy. Historical explanation: Munchhausen syndrome coined by Asher (1951) to describe patients who sought hospitalization at different hospitals under often dramatic circumstances for self-induced or simulated illnesses. Etiology not well understood, many authors feel it is the patient’s need for being taken care of. Trauma & abuse early in life. Early experiences with medical procedures & grudge against medical profession. Onset adulthood & chronic. Poor prognosis if patient goes from hospital to hospital. Severe personality disorders associated with this diagnosis. Issues of differential diagnosis & comorbidity