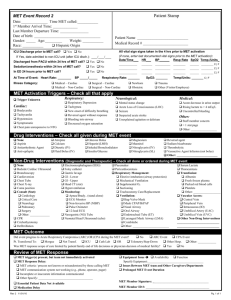
Examination findings
advertisement

Emergency Medicine Teach the Teacher EMTTT - Case Studies List 1-14 Case 1 Chest Pain Synopsis A 59 year old patient presents with ischaemic chest pain and pulmonary oedoma. An ECG is performed which shows an acute anterior myocardial infarction. Case 2 Respiratory Distress in a Child Synopsis A 3 year old boy is brought to the hospital by his parents with an 8 hour history of fever, lethargy, anorexia, noisy breathing and increasing respiratory distress. A diagnosis of possible epiglottitis is made. The course is complicated by the development of acute airway obstruction. Case 3 The Poisoned Patient Synopsis A 15 year old female presents unconscious to the local (rural) hospital after suspected poisoning. Her condition is complicated life-threatening cardiac toxicity due to cyclic antidepressant poisoning. Case 4 Paediatric Trauma Synopsis A three year old boy presents as a result of severe chest injuries following a pedestrian versus car accident. The case is complicated by severe shock, respiratory distress and possible head and abdominal injury. Case 5a The Fitting Patient a Synopsis A 25 year old patient presents in status epilepticus which is not controlled with benzodiazepines necessitating consideration of alternative therapies. Case 5b The Fitting Patient b Synopsis A 25 year old patient presents in status epilepticus which is not controlled with benzodiazepines necessitating consideration of alternative therapies. Case 6 Sick Child Synopsis A 12 month old child presents a high fever (>39 degrees), vomiting, decreased oral intake and deteriorating neurological status. A diagnosis of bacterial meningitis is considered likely. The progress is complicated by a deterioration in neurological status and development of focal neurological deficit. Case 7 Diabetic Coma Synopsis A 70 year old man presents with altered conscious state and fever. Initial assessment identifies diabetic ketoacidosis / hyperosmolar coma. A diagnosis of bacterial meningitis is also considered in view of positive findings on examination. Case 8 Altered Conscious State Synopsis A 75 year old female is brought to the local (rural) hospital by ambulance after being found collapsed at home. Examination confirms an extensive stroke (likely to be the result of an acute intracerebral bleed). Management is conservative and focused on counselling of the family. Case 9 Abdominal Pain Synopsis A 75 year old woman presents with shock requiring resuscitation. History and examination identifies an acute abdomen requiring urgent surgical intervention. Case 10 Headache -1- Synopsis A 38 year old man presents complaining of a severe headache. Although the examination is normal the history is highly suggestive of a SAH. Case 11 Adult Trauma Synopsis A 22 year old woman is brought to the local (rural) hospital by the ambulance following a fall from a horse. She is experiencing respiratory distress and is hypotensive. Deterioration in her neurological status occurs during the examination. Case 12 Dysrhythmia Synopsis A 48 year old patient presents with ischaemic chest pain which is complicated by the development of ventricular tachycardia and subsequently has a cardiac arrest. Case 13 Violent Patient Synopsis A 25 year old man is brought to the local hospital by police after acting strangely. He is extremely agitated and appears to be experiencing visual hallucinations. The management focuses on controlling for the risk of violence and identifying / managing the underlying cause. Case 14 Gynaecological Emergency Synopsis A 19 year old female who is 7 weeks pregnant presents to the local (rural) hospital with acute lower abdominal pain and PV bleeding. She is in shock and requires fluid resuscitation. Examination identifies POC in the cervical os. -2- Chest Pain # 1 Aims 1. Review the essential historical findings and examination features that must be considered in patient's with chest pain. 2. Review the ECG findings in myocardial ischaemia 3. Review the management of myocardial ischaemia (unstable angina and AMI) 4. Review the possible complications in IHD and their management Synopsis A 59 year old patient presents with ischaemic chest pain and pulmonary oedoma. An ECG is performed which shows an acute anterior myocardial infarction. Full Case Study # 1 A 59 year old male patient presents to the local (rural) hospital with acute onset of 2 hours of severe central chest pain which is described as like severe indigestion. The pain is constant, not related to movement or breathing and radiates to left arm and to jaw. There is associated dyspnoea and sweatiness. He reports a recent history of several weeks of similar but less severe pain which lasts 3 to 5 minutes comes on with exercise and is relieved by rest. In the last 24 hours he has had several prolonged episodes lasting 30 to 60 minutes that came on at rest. He has a past medical history of an Inguinal Hernia operation (5 years previously) and has recently been diagnosed with hypertension. He continues to smoke a pack / day. His brother (aged 52 years) has recently had a CABG. His only medication is Enalapril. Examination findings Vital signs Pulse BP Resp rate Temp Oximetry 2HS no bruits Clear to auscultation Chest JVP not raised Carotid pulse normal character and volume Abdomen Soft and non tender to palpation No ankle oedoma, No calf tenderness Foot / Ankle / swelling Foot pulses present 85 / min regular / normal volume in both arms 170 / 110 (checked in both arms) 28 / minute 36.8 degrees C 97% Q1 What immediate management is required for this patient Answer 1 The patient is likely to have myocardial ischaemia (unstable angina / AMI). Initial management will focus on stabilising the ABCDs, commencing preliminary treatment for the possible ischaemia, treating associated complications and initiating relevant investigations to confirm the diagnosis. The basic approach to the initial management of this patient would therefore include the following : Placement of an Oxygen mask (eg Hudson mask @ 10 l / min) Administration of Sublingual GTN (may be repeated once if pain persists and BP remains > 100 mm Hg systolic) Aspirin may be given bases of the suggestive history Attach cardiac and other monitoring devices (eg BP, oximetry) Establish IV access Draw routine bloods particularly baseline cardiac enzymes. (Others bloods generally performed include -3- CBP, EUC, Coags) Arrange an ECG Treat associated complications where identified eg pulmonary oedoma, cardiac dysrhythmia. Case Study 1 con't Management The patient is placed on oxygen and cardiac monitoring commenced. SL GTN and aspirin are administered. IV access is established and blood taken for CBP, EUC, Cardiac enzymes, Coags. The patient continues to experience severe pain. An ECG is performed which shows an acute anterior myocardial infarction. Q2 What are the characteristic changes of AMI on the ECG? Answer 2 Identify the significant changes on the ECG and discuss the sequence of ECG findings in AMI ie initial raised ST segments, flattening and inversion of the T wave and finally formation of the Q waves. Review the principle leads to examine for an inferior, septal, anterior and lateral AMI. It is also worth discussing the features of a posterior AMI (and use of posterior leads where this is suspected). Discuss the importance of considering right ventricular leads in a patient with inferior AMI to identify a right ventricular AMI and the clinical significance of this finding (ie possible hypotension and dramatic deterioration with nitrates, good response to cautious fluid loading to raise RV filling pressure) Q3 Describe further management of this patient Answer 3 IV GTN (if available and provided BP > 100mg Hg systolic. Requires frequent BP monitoring : an external "dynamap" is generally sufficient) : A second IV access is generally required. Heparin (after checking for contraindications). Nb. Low MW Heparin (eg Clexane) may be used. IV Heparin is preferred in major centres where angiography/angioplasty are available and may be initiated urgently. Assess patient for indications and contraindications with respect to thrombolysis (where this is an option) Consider IV Morphine to control pain A CXR is preferable if this can be arranged to confirm pulmonary odeoma and assess mediastinum (for evidence of enlargement suggesting aortic dissection). Admission/transfer for continuous cardiac monitoring (including serial ECGs and cardiac enzymes) Discussion Point - Discuss the indications and contraindications to the use of thrombolysis Q4 If the ECG did not show any of the characteristic changes of acute AMI how would this change your management Answer 4 Identify the range of possible findings on the ECG of a patient with AMI (normal in 3%, non specific ST/T wave changes, Bundle branch block, ST segment elevation / T wave inversion). Emphasize that the classic early changes of ST segment elevation are only found in 50% initial ECGs of patients with AMI ie the ECG does not exclude an AMI. -4- Where the ECG is nondiagnostic there are three possibilities : 1. One of the 50% of cases where the ECG is nondiagnostic in AMI (often a subendocardial AMI) 2. Unstable angina 3. Old changes unrelated to the presentation If an old ECG is available this can be extremely valuable to compare with the present ECG to determine if the changes are new. One or two serial ECGs (at 30 to 60 minute intervals) may also assist in identifying evolving ECG changes. In these cases management is always based on the history (in this highly suggestive of myocardial ischaemia) and therefore where the ECG is "normal" or nondiagnostic the patient should be managed on the basis of the history alone - if suggestive of ischaemia the following management is appropriate (and is identical to scenario #1 with the exception of the use of thrombolysis. Consider other causes (eg Aortic dissection) and exclude where possible IV GTN (if available and provided BP > 100mg Hg systolic. Low MW Heparin (after checking for contraindications). If the ECG shows new LBBB assess for indications and contraindications of thrombolysis Consider IV Morphine to control pain CXR if this can be arranged (particularly to identify other causes such as lung pathology, aortic dissection) Admission/transfer for continuous cardiac monitoring (including serial ECGs and cardiac enzymes) Respiratory Distress in a Child # 2 Aims 1. Identify priorities in management of the child with upper airway obstruction 2. Review the differential diagnosis of stridor in the young child 3. Discuss the management of acute airway obstruction Synopsis A 3 year old boy is brought to the hospital by his parents with an 8 hour history of fever, lethargy, anorexia, noisy breathing and increasing respiratory distress. A diagnosis of possible epiglottitis is made. The course is complicated by the development of acute airway obstruction. Full Case Study # 2 You are on call for a local (rural) hospital located about 4 hours by road (and at least one hour by air) from the nearest major hospital. The registered nurse on duty at the hospital calls at 2300 to inform you that a 3 year old boy has been brought in by his parents with an 8 hour history of fever, lethargy, anorexia, noisy breathing and increasing respiratory distress. His parents have given him 3 doses of nebulised salbutamol, the last 30 minutes ago. He has a past history of recurrent otitis media and asthma. His only medication is Salbutamol PRN. On arrival you find the child is alert, appears markedly anxious with saliva dribbling from the side of his mouth and sitting up on his mothers lap with his chin forward and neck slightly extended. There is an inspiratory stridor, marked intercostal and supraclavicular soft tissue recession and no wheeze on auscultation of the lungs. -5- Vital signs: T = 38.9 RR = 38/min PR = 150/min Sat 94% (air) Q1 What diagnoses need to be considered in this child and how may these be distinguished clinically? Answer 1 (Inspiratory) stridor is a sign of upper airway obstruction whereas (expiratory) is characteristic of lower airway obstruction. Although rare since the introduction of the HIB vaccination, epiglottitis is the most likely possibility in this child. The major differential diagnosis is generally croup (see table 1 below). Other possible causes in this case include retropharyngeal abscess, bacterial tracheitis and diphtheria. Table 2 lists causes of stridor. Epiglottitis generally occurs in children 2 - 7 years old. The usual history is of the abrupt onset (within hours) of fever, sore throat, dysphagia and drooling. On examination the child appears toxic, anxious, breathing quietly with little air movement. There is No hoarseness or cough and the child speaks in a whispering voice. Characteristically the child is sitting upright and refuses to lie flat. When examined closely they are found to be in the sniffing position (Chin forward / neck slightly extended). Table 1. Comparison of the clinical features of Croup and Epiglottitis Feature Onset Preceding coryza Cough Able to drink Drooling saliva Appearance Fever Stridor Voice Croup Over days Yes Severe, Barking Yes No Unwell < 38.5 C Harsh, rasping Hoarse Epiglottitis Over hours No Absent or slight No Yes Toxic, Very ill > 38.5 C Soft Reluctant to speak, muffled Table 2. Differential diagnosis for Stridor Incidence Very common Common Uncommon Rare Diagnosis Viral Croup Recurrent or spasmodic Croup Epiglottitis, Laryngeal Foreign body Retropharyngeal Abscess, Anaphylaxis, Diphtheria, Bacterial tracheitis, Trauma, Smoke inhalation Q2 Outline how you would proceed to manage this child. Answer 2 This child is at high risk of acute airway obstruction. The intubation will be extremely difficult -6- because of the swelling and loss of landmarks. A clinician experienced in paediatric airway management / anaesthesia is urgently required if the medical officer does not have these skills. A retrieval team is also needed to transfer the child to a paediatric ICU (and may in fact also be the only option of getting a clinician skilled in intubating in this situation). They should be notified immediately! The best management in the current situation would be to leave the child undisturbed sitting on the parents lap (never attempt to look into the mouth using a tongue depressor). An oxygen mask can be held as close to the face as is tolerated without upsetting the child. Equipment of urgent airway management should be checked and set up beside the child and the medical officer should not leave as the child may suddenly obstruct their airway. Critical Interventions 1 Leave the child undisturbed Do not attempt to look in the mouth Call for an experienced anaesthetist / retrieval team Prepare equipment for possible airway obstruction Case Study 2 con't The retrieval team has been called and will arrive in about 15 to 20 minutes. Unfortunately the child’s breathing has deteriorated becoming slow and the saturations have fallen to 90%. He has become drowsy and difficult to rouse. Q3 Outline how will you manage this situation? Answer 3 The child’s airway has become severely compromised resulting in the development of respiratory failure. Unless immediate intervention is initiated complete airway obstruction will rapidly result and the child will die. There is no option but to intervene. The most appropriate intervention in this situation is NOT to attempt intubation – the child is already seriously hypoxic and it will be extremely difficult to intubate and even if successful the attempt will likely take considerable time resulting in prolonged hypoxia. The most appropriate response is to first try to bag and mask the child with 100% oxygen. In most cases this will be possible and result in clinical improvement. Depending on the experience of the medical officer an intubation attempt could be then tried or alternately continued bag and masking until the retrieval team arrived (15 to 20 mins away). If this fails an attempted intubation may be tried but is unlikely to be successful due to the distortion in structures. Needle cricothyrotomy and jet insufflation is preferred but acts only as a temporising measure and may be used for a maximum of 30 mins before definitive airway management is required. Critical Interventions 2 Critical interventions Bag mask with 100% oxygen Needle cricothyrotomy if this fails The Poisoned Patient # 3 Aims 1. Discuss the approach to a patient presenting with poisoning 2. Illustrate the importance of using an ABCDE approach in the stabilisation of the critically ill patient -7- 3. Discuss the recognition and management of cardiac toxicity in cyclic antidepressant poisoning 4. Discuss the referral of a critically ill patient Synopsis A 15 year old female presents unconscious to the local (rural) hospital after suspected poisoning. Her condition is complicated life-threatening cardiac toxicity due to cyclic antidepressant poisoning. Full Case Study # 2 A 15 year old female presents to the local (rural) hospital after her parents found her collapsed on the floor at home with an empty packet of amitryptline (a cyclic antidepressant) on a nearby table. She had last been seen 2 hours previously by her mother and had recently been upset following breaking up with her boyfriend. On examination the patient is lying with her eyes closed on the bed. Her breathing is noisy and stridorous. The peripheries are cool. She is unresponsive to voice but withdraws to painful stimulation Vital signs : BP 80/40. PR = 140 / min RR = 8 / min Sat = 91% Q1 What are your immediate priorities in management of this patient ? Answer 1 1. Relief of airway obstruction and respiratory depression Administer oxygen. Basic airway manoeuvres should be used initially to clear the airway (such as extending the head, suction, jaw thrust, Guedel airway) and a bag and mask used to ventilate the patient. This should be followed by intubation to protect the airway from aspiration and allow effective ventilation. 2. Correct shock The patient is in shock. Management requires IV access and administration of a fluid bolus 500 ml NS (and repeated if required). Cardiac monitoring should be arranged to identify an associated dysrhythmia and an ECG performed to identify cardiac toxicity from the cyclic antidepressants. 3. Altered conscious state Although it seems most likely that the altered conscious state is due to an overdose other immediately treatable causes of coma need to be considered including hypoglycaemia, raised intracranial pressure and narcotic overdose. A blood glucose level should be performed (or where not available 50% dextrose should be given) Naloxone should be administered IV. A search for evidence of raised intracranial pressure should also be performed. Thiamine is also often administered particularly if there is a history of alcohol abuse. A check for possible head injury is also important. Critical Interventions 1 Intubation and ventilation IV access and fluids Cardiac monitoring Blood glucose level Case Study 3 con't A guedel airway is inserted and assisted ventilation with a bag and mask commenced and continued by one of the nursing staff. An IV line is established and a 500 ml bolus of IV normal saline is administered. This is repeated a short while later. Intubation is performed without complication. Vital signs are repeated -8- PR = 140 / min BP = 110 / 60 RR (ventilated) Sat = 98% The ECG shows a RBBB and a sinus tachycardia characteristic of cyclic antidepressant toxicity. Q2 Outline any further management and disposition of the patient Answer 2 Although the patient’s BP has responded to the fluid bolus the ECG shows the presence of significant cardiac toxicity placing the patient at great risk for dysrhythmia or a further deterioration in blood pressure. Sodium bicarbonate is a useful agent in cyclic antidepressant poisoning and acts by antagonising the cardiac toxicity of these agents. It is required if fluids do not correct hypotension or the patient has evidence of cardiac toxicity on the ECG (Early subtle but highly significant changes are a Terminal S wave in Lead I and Terminal R wave in AVR. Later changes are the prolongation of conduction : Widened QRS > 100 msec in RBBB pattern). As this patient has significant cardiac toxicity sodium bicarbonate should be administered in a dose beginning with 1 mmol / kg and followed by an infusion of 100 to 150 mmol in 1000 mls 5% dextrose over 4 to 6 hours ( Nb. An ongoing bicarbonate infusions usually follows the bolus dose and titrated against pH to maintain pH = 7.50. As ABGs will not be available in many rural centres the infusion may need to be either titrated against width of QRS / clinical response or repeated boluses given at the sign of further deterioration) Other important management will include Placement of an orogastric tube and administration activated charcoal. Bloods eg CBP, Biochemistry, Coags and serum paracetamol / alcohol IDC CXR Disposition The patient will require ICU management. Depending on the rural centre this will generally involve retrieval/transfer to a major hospital facility. If there is time discuss the specific circumstances of the participants and who/where they would call to arrange retrieval of the patient. Paediatric Trauma # 4 Aims 1. Review the steps in the immediate assessment of the trauma patient 2. Discuss the resuscitation of the seriously injured child. 3. Compare how the injured child differs from the adult Synopsis A three year old boy presents as a result of severe chest injuries following a pedestrian versus car accident. The case is complicated by severe shock, respiratory distress and possible head and abdominal injury. Full Case Study # 2 While reviewing one of your inpatients at the local (rural) hospital you are called urgently to assess a 3 year old boy who has just been the victim of a hit an run accident immediately outside the hospital. An oxygen mask has been placed and is running at 10 l / min. The mother is extremely -9- distressed and being comforted by a nurse. On examination there is marked tachypnoea and soft tissue recession but no evidence of airway obstruction. The child appears pale with blue mottled cold peripheries and delayed capillary refill (> 4 secs). The child groans and localises a painful stimulus. Pupils are size 4 and reactive to light. Vital signs are: Respiratory rate = 50 /min Pulse > 150 / min Blood pressure = 95 systolic Saturation = unobtainable BSL = 4 mmol/l Several attempts to obtain IV access fail. Q1 What are the immediate priorities in the management of this child? Answer 1 The immediate management priorities are respiratory distress, shock and altered conscious state. It is of great concern that no IV access has yet been established despite several attempts as it is clear this child is in shock and will require IV fluid resuscitation. A suggested plan of management is shown below. 1. Call for additional medical assistance (is there another medical officer in the hospital (eg in theatre) or nearby at a GP surgery. 2. Place a cervical collar 3. Increase oxygen mask to maximal (15 l / min). Be prepared to bag and mask if respiratory assistance is required. 4. IV access must be established. Options include femoral IV access, venous cutdown and intraosseous (unsuitable at present as he is withdrawing to pain). Collect blood for Group and match. 5. Administer rapid fluid bolus 20 ml/kg normal saline (or colloid if preferred). Send for O neg blood and request urgent Type specific blood. Reassess after 20ml/kg bolus and administer a second bolus followed by O neg blood (10ml/kg) titrated to response Critical Interventions 1 Cervical collar Oxygen Establish IV access and give 20 ml / kg fluid bolus Case Study 4 con't An IV access is established and firmly secured. (A second IV line is obtained a short while later). Blood is drawn for CBP, EUC/LFT’s, G&M. A bolus of 280 ml (20ml/kg) of normal saline is given rapidly and repeated. O negative blood (10ml/kg) is commenced. Reassessment of vital signs following administration of IV fluids : BP 95 systolic, PR = 120. Capillary refill < 2 secs. The child remains tachypnoeic (50/min). Sat = 95%. There is marked bruising and a “crunching” feel over the left chest wall. There is an absence of breath sounds on the left and it is dull to percussion. Neurological status : crying and asking for “mum”, localising painful stimuli, eyes open to verbal stimulus. Pupils equal and reactive. Q2 Outline any further immediate management - 10 - Answer 2 The child has a haemothorax. A CXR will confirm this although his respiratory status is borderline (sat 95%) but with improving conscious state and circulation a CXR could be performed first if this will not delay insertion of a thoracostomy tube. Where Xray is immediately available this could be performed while the thoracostomy tray is being set up and the procedure explained to the mother. Continued close monitoring of the child’s respiratory status is critical. Consideration may also be given to administration of IV analgesia given the extent of the chest wall injury (presumably numerous rib fractures and a flail chest) although this must be weighed against the possibility of causing respiratory depression and exacerbating CNS depression masking a deterioration in neurological status. Continued close monitoring of the patient will be required. A secondary survey is necessary and should include a thorough “head to toe” examination to identify all other injuries, the trauma series of xrays (CXR, Cspine, pelvis) and other relevant xrays and a urinalysis. Considerable attention should also be placed on identifying a possible abdominal injury (in view of the fractured ribs a splenic or renal injury is highly likely), lung contusion (resulting from the blunt chest trauma evidenced by the flail chest) and head injury (evidenced by the altered conscious state initially although this may have been due to the severe hypovolaemia). Critical Interventions 2 Insertion of a Chest tube Disposition This child will require paediatric ICU management, may require ventilation if their respiratory status deteriorates (eg due to associated lung contusion) and possible thoracic surgery if the bleeding does not settle. Further investigation to rule out splenic/renal injury and head injury will also be required. Retrieval to a paediatric ICU should be arranged as soon as practical. The Fitting Patient - Case Study # 5a Aims Review the management priorities for the convulsing patient. Discuss treatment options for the controlling seizures. Discuss the management of patients in whom first line agents do not control the seizure. Synopsis A 25 year old patient presents in status epilepticus which is not controlled with benzodiazepines necessitating consideration of alternative therapies. Full Case Study # 5a A 25 year old male is brought by ambulance to the local hospital after collapsing at a party and reportedly having a seizure. He is well known to you and has a past history of seizures following a head injury as a child. His only medication is carbamazepine. Shortly after arrival at hospital he becomes stiff and apnoeic and then begins to thrash his arms and legs violently. He froths at the mouth, makes gurgling sounds and becomes a blue – gray colour. The ECG monitor shows a sinus tachycardia = 130/min. Questions What are the priorities in the management of this man? What options are available if IV access is not possible? Answer 1 The priorities are the airway, breathing, circulation and to abort the seizure activity. It is critical that attention is paid to ensuring the airway is patent (eg vomitus is cleared and tongue is not obstructing the - 11 - airway), oxygen is applied, bag and masking is not usually required but should be available and circulation is checked (hypoxic seizures secondary to arrest or arrhythmias may occur). Benzodiazepines are the first line of management. Midazolam, Clonazepam and Diazepam are options for IV use. Where IV access is not available IM Midazolam or PR Diazepam may be used. Ongoing priorities are to ensure an unobstructed airway, observe for possible respiratory depression (as a result of Midazolam), check BSL, consider use of longer acting anticonvulsants to control further seizure activity and identify contributing factors to the seizure (eg noncompliance, use of illicit drugs etc). Critical Interventions Apply Oxygen Clear the airway : Suction, Jaw thrust Control seizure using a Benzodiazepine Case Study # 5a con't Oxygen is applied. The patient is rolled into the left lateral position, the airway is suctioned to remove secretions and a jaw thrust performed to open the airway. The patient’s colour improves and an oximeter reading shows 98% a short time later. The patient is given IM Midazolam 10 mg (0.15 mg / kg) is administered but fails to control the seizure. An IV line is established. A blood sugar level is performed (5 mmol/l). IV Clonazepam 0.25 mg is administered without effect. A further 0.25 mg is administered 5 minutes later. The patient continues to convulse. The patients airway is maintained and oxygen delivered via a Hudson mask. His respirations are shallow and his respiratory rate 10 / minute. Oximetry reading remains at 95%. Questions The nursing staff ask if you wish for him to have another dose of Clonazepam. Do you agree ? How will you manage the patient if benzodiapzepines do not control the seizure ? Answer 2 The patient appears to be developing significant respiratory depression. The respiratory rate alone is not a good guide to respiratory depression as it is the effectiveness of the respiratory effort that is critical and as his respiratory effort appears shallow this suggests significant respiratory depression. The oximetry readings are not useful, only likely to fall when the patient is profoundly depressed. The ppCO2 (available on an ABG or end tidal CO 2 monitor) provides a much better guide to respiratory depression. No further benzodiazepines should be given. As other anticonvulsant agents will exacerbate the respiratory depression and the patient has an unprotected airway the best option under this circumstance is to induce anaesthesia / muscle relaxation and intubate the patient. This will protect the airway and allow assisted ventilation which is likely to be required. Critical Interventions Rapid sequence induction Endotracheal intubation Assisted ventilation Case Study # 5a con't Using a rapid sequence induction procedure and cricoid pressure, the patient is given Thiopentone 350 mg (5mg/kg) and Suxamethonium 100mg (1.5 mg /kg) and successfully intubated with an 8.0 ETT. The tube location is verified by auscultation and a CXR. Although ceasing for a brief period during the intubation procedure after 10 minutes the patient shows evidence of further convulsions. Question Why have the seizures recurred and how should they be managed ? Is the use of a long acting muscle relaxant an option for controlling the seizure ? - 12 - Answer 3 Thiopentone is a very effective anticonvulsant but its duration of effect is brief equivalent to its sedation time (< 10 mins). In addition the use of a muscle relaxant (Suxamethonium) will mask underlying seizure activity for the period of effect (5 mins usually). The seizures recurred as a result of the wearing off of effect of these two drugs therefore. Long acting muscle relaxants should generally not be used as they mask seizure activity allowing the damaging CNS overactivity to continue untreated and result in possible severe CNS injury that complicate status epilepticus. The seizures should be controlled with the use of further anticonvulsants such as Midazolam, Propofol, Thiopentone or Phenobarbitone. As the patient is intubated and ventilated there are no problems with causing respiratory depression / apnoea. Doses of the respective agents are shown below. Midazolam infusion : 0.75 to 2 microgram / kg / min Propofol : 1mg / kg bolus + Infusion: 50 microgram / kg / min Thiopentone infusion : 1 to 7 mg / min Phenobarbitone : 15 to 18 mg / kg loading dose. No infusion required Critical Interventions Commence infusion of anticonvulsant agent eg midazolam, propofol, thiopentone or phenobarb. Avoid long acting muscle relaxants Case Study # 5a con't Two bolus doses of Midazolam 5 mg and 5mg are given and control the seizure. This is followed by a Midazolam infusion commencing at .75 microgram /kg / min is commenced and increased to 4 microgram / kg / minute over 20 minutes. No further seizure activity is evident. The patient is ventilated with IPPV at a rate of 14 / minute Question In the context of where you practice, discuss the disposition of a patient such as the one above. The Fitting Patient Case 5b Aims Review the management priorities for the convulsing patient Discuss treatment for the control of seizures Discuss the management of patients in whom first line agents do not control the seizure Synopsis A 25 year old patient presents in status epilepticus which has not been controlled with benzodiazepines, necessitating consideration of alternative therapies Full Case Study # 5b A 25 year old male is brought in by ambulance to the local hospital after collapsing at a party and reportedly having a seizure. He is well known to you and has a past history of seizures following a head injury as a child. His only medication is carbamazepine Shortly after arrival at hospital he becomes stiff and apnoeic, and then begins to thrash his arms and legs violently. He froths at the mouth, makes gurgling sounds, and becomes a blue-grey colour. The ECG monitor shows a sinus bradycardia = 130/min Questions What are the priorities in the management of this man? What options are available if IV access is not possible? Critical Interventions O2 Clear airway – suction, jaw thrust Seizure control – IM midazolam IV access - 13 - BSL IV clonazepam Full Case Study # 5b con't After these interventions, the patient continues to convulse, his respirations are shallow, and his respiratory rate 10/min. Oximetry remains 95% Question What critical interventions are required at this stage? Critical Interventions Rapid sequence induction Endotracheal intubation Assisted ventilation Sick Child - Case 6 Aims Review the differential diagnosis of the febrile child Discuss the presentation of the child with bacterial meningitis Discuss the role of investigations in the assessment of bacterial meningitis Review the timing of administration and choice of antimicrobial agents Recognise and treat raised intracranial pressure complicating meningitis Synopsis A 12 month old child presents a high fever (>39 degrees), vomiting, decreased oral intake and deteriorating neurological status. A diagnosis of bacterial meningitis is considered likely. The progress is complicated by a deterioration in neurological status and development of focal neurological defici t. Full Case Study # 6 You are called to the local hospital late one evening to assess an 12 month old girl who has been unwell for several days with a high fever (>39 degrees), vomiting and decreased oral intake. The child had been seen by a colleague earlier in the day but the mother is anxious to have the child reviewed. The child had slept most of the day, vomited once, refused any fluids, and became irritable if picked up preferring to be left alone. Apart from 4 hourly paracetamol the child has not received any medications The child has no significant past medical history and normal neurological development. On examination you note the child to be lying curled up and apparently asleep on the examination bed. The child is difficult to arouse (opening eyes only with loud verbal and gentle physical stimuli) and begins to moan when you try to examine her. ENT, chest and abdominal examination are unremarkable. The mucous membranes appear moist and there are no other signs of significant dehydration. Vital signs PR = 140/min T = 40.1 degrees C RR = 35 / min Questions What diagnoses need to be considered in this child? How would you proceed in managing this child? This child is at high risk of bacterial meningitis. Encephalitis is also a possibility. Other causes of severe sepsis need to be considered but can often be identified on examination and include complicated urinary tract infection, osteomyelitis/septic arthritis, pneumonia, gastrointestinal sepsis (eg perforated appendicitis). In addition many children may appear ill and lethargic with a high fever and improve as the fever is controlled. It is tempting to hypothesize that this may be the case in this child, however the history of progressive deterioration and other clinical features (such as wanting to be left alone or preferring to “curl” up) are suggestive of more severe illness. - 14 - Management would centre on confirming the diagnosis of meningitis and commencing antimicrobial therapy. Urgent IV access is required and the drawing of blood cultures. (A CBP may also be drawn but the result will not influence immediate management.) To LP or not? : Controversy exists as the precise timing of the lumbar puncture and it needs to be seriously considered whether this should be postponed in view of the altered conscious state of the child which may be an early sign of raised intracranial pressure. In a small rural centre where resources (and back up) are limited it would seem appropriate to postpone the lumbar puncture, provided blood cultures had been drawn, and administer the antimicrobials. Attempts also to control the temperature may also help to clarify whether the altered conscious state is due to the fever or the result of raised intracranial pressure. An improvement in conscious state would allow a lumbar puncture to be safely performed Antimicrobials currently recommended for the initial treatment of bacterial meningitis are a third generation cephalosporin (Cefotaxime or Ceftriaxone) plus Vancomycin (due to rising pneumococcal resistance to third generation cephalosporins). Critical interventions IV access Blood cultures IV Cefotaxime / Ceftriaxone + Vancomycin Case Study # 6 con’t An oxygen mask is placed on the child (and well tolerated) and a paracetamol suppository administered. Attempts to establish an IV in the cubital fossa and hands are not successful. An attempt to perform a venous cutdown is unsuccessful although blood is drawn for blood cultures. As bacterial meningitis is considered likely a dose of Ceftriaxone is administered IM. The paediatric ICU consultant is contacted and agrees that the child will require retrieval. He suggests the administration of IM dexamethasone in addition to the Ceftriaxone. It is estimated that the team will arrive in 2 hours. The child’s neurological status continues to deteriorate. At one hour the child is no longer responding to voice and the left eye is noted to be turned outward. His breathing has also become rapid and shallow. Questions What has happened? How is this managed? There is no IV access. What are the options? The child has raised intracranial pressure and is in the process of “coning”. Unless immediate intervention in the form of intubation/ventilation is instituted the child will rapidly deteriorate and proceed to respiratory arrest and brain death. An intraosseous needle should be placed, as this will provide rapid IV access. Intubation should be performed using sedation and muscle relaxation (eg Thiopentone / Suxamethonium) and rapid sequence induction procedure. Following intubation the child should be gently hyperventilated to assist with lowering intracranial pressure. Mannitol may also be required but this should be discussed with the ICU consultant before use. Critical interventions Intraosseous Insertion to establish IV access Endotracheal Intubation Diabetic Coma - Case 7 Aims - 15 - Describe the presentation of diabetic coma Review the assessment and management of diabetic coma Discuss precipitating factors for diabetic coma Synopsis A 70 year old man presents with altered conscious state and fever. Initial assessment identifies diabetic ketoacidosis / hyperosmolar coma. A diagnosis of bacterial meningitis is also considered in view of positive findings on examination. Full Case Study # 7 While you are mid-way through a busy morning of consulting following the Easter holiday long weekend, the receptionist notifies you that she has just received a distraught call from a woman. She is concerned that when she checked her father today he won’t wake up and appears not to have taken his tablets for a few days. She has requested you come urgently to the house to see him. You saw the woman’s father for a chest infection the week previously. He is aged 70 years, has a long history of ischaemic heart, COAD and type 2 Diabetes mellitus. He continues to smoke despite your advice to the contrary. You suspect he is non compliant with his medications and often delays seeking medical assistance until he is quite ill. On his most recent visit to you he presented because his daughter ‘made” him. Apparently she was worried about his cough and as she was going away for the Easter weekend, insisted he see a doctor and have it treated before she went away. You prescribed him Rulide and a 10 day course of Prednisolone 50 mg daily. His other medications include Salbutamol, Becloforte, Imdur, Aspirin and Glicazide. You advice that the daughter call an ambulance immediately to bring the patient to the local rural hospital situated a short distance from the surgery. The nurse informs the surgery of the patient’s arrival 45 mins later and has a high BSL. You leave the surgery to review the patient. Vital signs : BP = 110 / 80 PR = 130 / min RR = 28/min Sat = 96% T = 38.5 degrees C BSL = Hi On examination He appears severely dehydrated with dry mucous membranes and decreased tissue turgor. He groans to verbal stimuli. Pupils equal (size 4) and reactive to light. Reflexes are symmetrical and generally decreased. Chest and abdominal examination are unremarkable apart from moderately decreased air entry and a few scattered expiratory rhonchi (normal for him) There are no signs of head injury. There is possible meningism. Questions What are the immediate priorities in management ? The immediate priorities in the management of the patient with altered conscious state is airway, breathing, circulation and disability. In this context this would translate as the following Check airway : Stable at present Apply oxygen mask Check breathing : Tachypnoeic. Sat 96% Check circulation : Severe Dehydration Immediate IV fluid Cardiac monitoring Check disability : Hyperglycaemia Confirm result Draw blood for EUC, CBP, Cultures. ABG if available - 16 - Commence insulin Critical interventions IV access Rapid IV fluid replacement IV insulin Case Study # 7 con’t 1 The patient is placed on a cardiac monitor (sinus tachycardia) and IV access established. Blood is taken for biochemistry, blood picture and blood cultures. A repeat BSL is Hi. A 1000 ml of normal saline is commenced at a rate of 1000 ml / hour. A bolus of 10 U Actrapid is administered and an infusion commenced at 6 U/ hour. Question What further management will be required ? Close monitoring of the patient’s status will be essential. This will include frequent monitoring of the BSL, insertion of an IDC to monitor fluid output, continuous cardiac monitoring and commencement of potassium replacement to second and subsequent bags of fluid. In general these patients require 4 to 5 litres of normal saline over the first 8 to 12 hours, potassium replacement and insulin infusion @ 2 to 6 u / hour. When the BSL falls below 15 mmol/l the insulin infusion is decreased to 2 to 3 U/hour and the normal saline replaced by 5% dextrose. Further management must also focus on identifying a precipitating factor such as an infection (likely in this patient), silent myocardial infarction, acute surgical illness (eg appendicitis) etc. This will require an ECG, CXR, U/a (sent for MC&S) (and blood cultures in this case because of the fever). The white cell count is unreliable at identifying infection as the stress of the hyperglycaemic state is sufficient to cause a raised WCC. There is a dilemma in this patient as the fever, apparent meningism and altered conscious and meningitis needs to be excluded. A lumbar puncture is contraindicated in view of the altered conscious state. The best approach is to ensure blood cultures are taken (and a urine for microscopy if possible) and then administer antibiotics (eg cefotaxime) to cover possible meningitis. Antigen testing of urine can be used to identify the organism at a later stage. Should the patients conscious state improve with treatment of the hyperglycaemia (as would be expected if hyperglycaemia were the predominant cause for the altered mental state) then a lumbar puncture may not be necessary. As Herpes encephalitis is also a possibility treatment with acyclovir may be considered if the patients conscious state does not improve. Critical interventions Continuous Cardiac monitoring Potassium replacement Exclude precipitating factors Commence antibiotics in view of possible meningitis Case Study # 7 con’t 2 There is a good response to the initial management with evidence of improving conscious state. The fever remains at 38.5 despite the administration of paracetamol. The patient does not complain of a headache and the apparent meningism has resolved. He is orientated to place and person but remains a little confused to the time. He reports recent polyuria and feeling very thirsty. Urine microscopy reveals a urinary tract infection. His initial blood results become available later that day. They are shown below. EUC Glucose 85 mmol/l Na+ 150 mmol/l K+ 4 mmol/l HCO3 20 mmol/l - 17 - CBP Urea Creat WCC Hb 30 mg/dl 0.20 21,000 16.5g/dl Questions What is your final diagnosis ? Identify possible contributing factors. This man developed (Diabetic) Nonketotic Hyperosmolar coma. Precipitating factors for this episode are likely to include recent chest infection/exacerbation of COAD, concomitant urinary tract infection and use of prednisolone. Altered Conscious State Aims Discuss the approach to a patient presenting with altered mental state Illustrate the importance of using an ABCDE approach in the stabilisation of the unconscious patient Discuss the differential diagnosis of altered mental state Discuss the management of the patient with a large intracerebral bleed Synopsis A 75 year old female is brought to the local (rural) hospital by ambulance after being found collapsed at home. Examination confirms an extensive stroke (likely to be the result of an acute intracerebral bleed). Management is conservative and focused on counselling of the family. Full Case Study # 8 A 75 year old female is brought to the local (rural) hospital by ambulance after being found collapsed at home. On examination Vital signs : BP = 200 / 120. PR = 110 / min RR = 20 / min T = 35.9 degrees She is drowsy and lying with her eyes closed. She is unresponsive to verbal or painful stimulation. Questions What are the management priorities in the first 10 minutes ? What diagnoses need to be considered ? What are the management priorities in the first 10 minutes ? Initial management of the patient with altered conscious state is focused on the completion a primary survey/resuscitation (ABCDEs). This will involve ensuring a clear airway, placement of an oxygen mask, monitoring (cardiac, oximetry, BP), establishment of IV access, checking the BSL and consideration given to the administration of IV dextrose, thiamine and naloxone. Bloods are also often routinely drawn at this time (EUC& calcium, CBP, serum alcohol) and an ECG performed. Critical intervention : primary survey/resuscitation Identify Airway Compromise Listen/feel for air movement/obstructive sounds Check Look for chest rise with inspiration Place oxygen mask - 18 - Identify Ineffective Ventilation (Breathing) Respiratory rate Check Auscultation and percussion of lungs Attach Oximeter Identify Shock (Circulation) Pulse rate and Blood pressure Check Capillary refill and perfusion of extremities Attach cardiac monitor Establish IV access Identify impaired conscious state (Disability) Conscious state Check Pupillary reaction and equality Movement of limbs / Seizure activity Check temperature/ Blood Glucose level. Consider giving Naloxone, Dextrose, Thiamine Expose the patient for further assessment Avoid causing Hypothermia What diagnoses need to be considered ? Diagnoses that need to be considered in the unconscious patient include infection (especially CNS such as meningitis/encephalitis), vascular (eg SAH, CVA, intracerebral bleed), trauma (eg subdural haematoma), endocrine/metabolic (eg hypoglycaemia, renal or liver failure), drug related (eg withdrawal, overdose, drug abuse), seizure/postictal, hypertensive encephalopathy, hypoxia/hypercapnia, hypo/hyperthermia and hypovolaemic shock. Case Study # 8 con’t 1 A guedel airway is inserted and an oxygen mask is placed. An oximeter is attached (Sat = 98%). The peripheries demonstrate normal capillary refill. An IV access is secured and the patient placed on a monitor (Sinus tachycardia 110 / min). The pupils equal, size 4 and reactive to light. The BSL = 12 mmol / l Further history is available from the daughter with whom she has been living for the past 3 months. Apparently she has been well and got out of bed that morning, had a shower and ate breakfast without commenting that was feeling unwell. She had last been seen an hour previously by the daughter who had gone to fetch some groceries from the shops nearby. She has a past history of exertional angina, type 2 diabetes mellitus and hypertension. Her medications include Isosorbide mononitrate, Verapamil, Aspirin and Glibenclamide. Questions What is the most likely diagnosis/diagnoses ? Outline how you would confirm your suspicions in this patient ? The sudden deterioration makes a vascular cause (stroke) a high possibility. Given that the patient is unconscious and has a history of hypertension an intracerebral bleed is more likely that a thrombotic or embolic cause. A neurological examination should be performed looking for focal neurological findings suggesting a primary CNS cause. Less likely causes that need to be considered include trauma (eg h ead injury due to a fall) and self poisoning. Critical intervention In the patient with altered consciousness the following should always be checked ABCDs Vital signs Oximetry Blood Glucose - 19 - Pupils (signs of raised ICP, toxic ingestion) Reflexes Signs of head injury (or other injury suggesting a fall) Meningism (provided trauma is first excluded) Urinalysis Case Study # 8 con’t 2 An examination is performed. Her breathing is irregular with periods of rapid breathing followed by short pauses. Her chest is clear to auscultation. She has dual HS and a systolic murmur consistent with mitral incompetence (documented previously). Her reflexes are unequal with decreased reflexes noted on her left arm and leg associated with an upgoing plantar reflex. Her eyes are turned toward the left side. Her pupils are size 4 and reactive to light. There is no evidence head trauma. Meningism is not assessed. ECG : Sinus tachycardia. Unchanged from previous ECGs An IDC is placed and drains 200 ml urine. U/a shows glucose and a trace of protein. Questions Outline your management of this patient in the circumstances of your practice ? What will you tell the daughter ? The examination confirms that the patient has had stroke (likely to be the result of an intracerebral bleed). The management in this circumstance is conservative. Although a CT scan is always useful to confirm suspicions it will not change the outcome and must be weighed against the fact that this is likely to require transfer of the woman denying the family time with her during her last hours. (Nb. Although the patient is hypertensive (200/120) this is commonly found in stroke and is a secondary event rather than a primary cause. No treatment should be instituted in this case for the raised BP.) The daughter should be told the diagnosis (an extensive stroke) and the prognosis (she will likely die in the next 12 to 24 hours as the pressure builds up in the brain). She will not be in any pain or suffer. There is no treatment possible except to make her comfortable. The daughter should advise her family and they will be free to spend as a long as they want with the patient. Abdominal Pain - Case 9 Aims Review the initial management of the patient with shock Identify the common causes for acute abdomen in the adult Discuss the assessment and management of a patient with an acute abdomen Synopsis A 75 year old woman presents with shock requiring resuscitation. History and examination identifies an acute abdomen requiring urgent surgical intervention. Full Case Study # 9 A 75 year old woman is brought in by ambulance to the local (rural) hospital on Sunday morning after collapsing on the way to the toilet. On examination the patient is confused and appears pale. The peripheries are cool to touch and abdominal examination reveal marked lower abdominal tenderness and possible guarding. There are no masses palpable and no organomegaly. PR examination is normal and faecal testing fails to identify blood or melaena. Chest examination is unremarkable. Her initial observations are PR = 68/ min, BP = 60/40. Questions How would you proceed to manage this patient ? - 20 - Discuss the differential diagnosis ? The patient presents in severe shock and features suggesting the possibility of an acute abdomen. Initial management will focus on stabilising the patient and follows the ABCD approach to resuscitation. In this case the airway and breathing seem to be intact (but still always need to be formally assessed). The circulation seems to be major concern and requires immediate management with insertion of an IV, drawing of blood for G&M (and other testing) and IV fluid resuscitation with a 20ml/kg bolus of normal saline or colloid. Where possible O negative blood should be sent for so that it readily available should it be required. Reassessment of the patient after the bolus will indicate if a further 20ml/kg bolus will be required followed by 10ml/kg blood. Important considerations in the diagnosis include Abdominal Aortic Aneurysm, Acute GI bleed, Perforation of the bowel, Acute (haemorrhagic) Pancreatitis, Mesenteric infarction, Sepsis (eg acute cholecystitis, pyelonephritis) and trauma (eg splenic or liver injury from a fall). Non abdominal causes need also to be considered most importantly acute myocardial infarction, cardiac dysrhythmia, poisoning and septic shock. Critical Interventions IV access IV fluid resuscitation Case Study # 9 con’t 1 The patient is placed on oxygen and cardiac monitoring shows a narrow complex, sinus tachycardia. IV access is established using two large bore cannulae. A 20ml/kg (1500ml) Normal Saline bolus is commenced. Blood is sent for CBP, EUC, Amylase and G&M. The conscious state of the patient improves following the IV fluid and a history can be obtained. The patient reports a three day history of malaise, anorexia, frequent bowel actions (4 to 5 brown loose motions / day) and constant increasing severe central abdominal pain. She denies experiencing any nausea or vomiting, no fever or chills, no PR bleeding or melaena and no chest pain. She reports that the day previously she had felt faint on several occasions as she got up from bed and almost collapsed. She does not recall the collapse that morning but does remember trying to get out of bed in the night to go to the toilet. Her daughter who visits three times week, found her lying on the floor of her bedroom in the morning and called the ambulance. She past has a past history of hypertension and arthritis. Her medications include Atenolol, Natrilix and Voltaren. Vital signs are PR 60 / min BP 90/ 70 RR 24 / min T 35.6 degrees C BSL 6.5 mmol/l Oximetry could not be obtained Re-examination of the abdomen reveals marked lower quadrant tenderness and guarding. Questions What further assessment / management is required ? She requests something for the pain. How will you respond ? - 21 - Although further investigations (such as a decubitus AXR) may assist the diagnosis, it is clear the patient will require urgent laparatomy. Management should be focused toward arranging surgical intervention (either at the hospital where resources permit of by medical transfer to a suitable facility). As the patient remains hypotensive following completion of the fluid bolus, reassessment should be undertaken – is this primarily a hypovolaemic problem eg an acute bleed or a septic shock (vasodilation) problem ? An examination of the JVP will assist with this determination. In the absence of obvious bleed (ie no clinical AAA, no PR blood or haematemesis) septic shock seems more likely. The fluid resuscitation should be continued but with careful monitoring of the JVP and lungs (for pulmonary oedema). Repeat bolus dosing of 250ml normal saline and reassessment seems reasonable. Inotropic agents may be required (eg adrenaline) where evidence of fluid overload develops and hypotension persists. Case Study # 9 cont 2 Following the initial 1500 ml bolus of normal saline a further 500 ml of normal saline is administered. An abdominal Xray is ordered. A decubitus film demonstrates free gas below the right diaphragm. Vital signs are reassessed PR 65 / min BP 110/ 70 RR 24 / min Oximetry 97% Questions What further management is required ? In the context of where you practice discuss disposition of a patient such as this case ? This patient requires urgent laparotomy. IV antimicrobial agents should be administered (eg Amoxycillin + Gentamicin + Metronidazole ). Questions Discuss how and who will transfer this ‘unstable’ patient. Is retrieval the best option ? Critical Interventions IV antimicrobials Urgent laparotomy A note of interest At operation a gangrenous and perforated appendix was identified with pus in the peritoneal cavity. This case illustrates that elderly people may present atypically with appendicitis (and other acute abdominal conditions), often developing less obvious signs and presenting late. Headache - Case 10 Aims Identify the common life-threatening causes for headache Discuss the historical and examination findings that need to be considered in patients presenting with headache Describe the priorities in management of the patient with suspected Subarachnoid haemorrhage Synopsis A 38 year old man presents complaining of a severe headache. Although the examination is normal the history is highly suggestive of a SAH. Full Case Study # 10 - 22 - A 38 year old man presents to your rooms first thing on a Monday morning complaining of a severe headache. He has no significant past medical history. He reports that he has only the occasional headache from time to time but never “as bad as this”. He wonders if it is due to overdoing things on the weekend digging a pond in the garden. On examination his vital signs PR = 100 / min BP 140/70 RR = 15 / min Questions What other historical and examination features are vital to exclude a possible life-threatening cause for this man’s presentation ? Two life-threatening conditions need to be considered in this case : Subarachnoid haemorrhage (SAH). Bacterial meningitis. (In an older patient Giant cell arteritis needs also to be considered in view of the risk to vision). Critical to the assessment is the history of onset of the headache – a sudden, severe (worst ever) headache often associated with a collapse is characteristic of SAH. Onset during exertion (including sexual intercourse) is also important. A recent history of a similar sudden severe headache (a premonitory bleed) should also be asked about. Bacterial meningitis is associated with the more gradual onset of headache and associated with fever and meningism. Photophobia/sonophobia, nausea, dizziness, blurring of vision are commonly associated with these and the more benign types of headache and do not provide useful features to help distinguish the type of headache. A past or family history of migraine is likely to be significant and should be asked about. Any transient neurological symptoms (particularly involving the eyes) prior to the headache is also important clue to possible migraine. Examination aims to identify the presence of meningism, focal neurological findings and raised intracranial pressure. The vital signs including BP and Temp should always be checked as should the conscious state and orientation to TPP. (Where doubt exists a formal minimental may need to be performed). A focal neurological examination should examine the cranial nerves (including pupils) and check power, tone and reflexes in all limbs. The neck should be assessed for evidence of meningism and the fundi for papilloedoma. Critical interventions Examine for focal neurological findings Identify raised intracranial pressure Look for meningism Case Study # 10 con’t The headache began while he was having a shower that morning. At the time he thought he must have hit his head whilst in the shower because it he remembers finding himself on the floor and had a stinking headache which he had not had before. He also reports feeling nauseous and has vomited several times. He feels faint if he tries to stand and tries to avoid the light. He is alert and orientated to time, person and place. A brief screening neurological examination of the cranial nerves, power, tone and reflexes is normal. His pupils are size 4 and equal. Both react normally to light. He is able to move his neck without difficulty. T = 36.5 degrees C. ECG : Sinus tachycardia. No other abnormalities Questions - 23 - Outline further management ? This history is highly suggestive of a SAH. This needs exclusion. As this man is in a rural setting the management will depend on the availability of a CT scan. Management will require CT scan (most major country centres now have this available). This should be performed in the first 12 hours as the sensitivity decreases after this time. Nb. A normal CT scan does not exclude SAH. Where the CT scan is normal a Lumbar puncture will be required to rule out SAH. This should be performed at least 12 hours after the onset of the headache as it takes this time for Xanthochromia to reliably develop in the CSF. (Xanthochromia is the straw coloured appearance of the CSF due to the breakdown of RBCs in the CSF and is diagnostic of SAH). Discuss how this scenario could be managed in the setting each of the participants in the group. Have they experienced a similar situation ? How did they manage it ? Was it a satisfactory outcome ? What problems are they likely to encounter in management of this type of situation ? How should this patient be transferred if no CT is available ? Is lumbar puncture alone an option in an alert patient with no evidence of raised intracranial pressure ? What problems does this present if it is positive with transfer of the patient ? Critical interventions Transfer / arrange urgent CT scan Lumbar puncture after 12 hours is negative CT scan Adult Trauma Case Study 11 Aims Review the steps in the immediate assessment of the trauma patient Discuss the resuscitation of the seriously injured adult Review the signs and management of raised intracranial pressure Synopsis A 22 year old woman is brought to the local (rural) hospital by the ambulance following a fall from a horse. She is experiencing respiratory distress and is hypotensive. Deterioration in her neurological status occurs during the examination. Full Case Study # 11 A 22 year old woman is brought to the local (rural) hospital by the ambulance following a fall from a horse. The accident happened at a local farming show. She was attended to promptly by the ambulance crew on site. They report that she was knocked unconscious in the accident and appears to be experiencing difficulties breathing. Management by the ambulance has included administration of oxygen via a mask, immobilisation of the neck with a cervical collar, establishment of an IV access and administration of 500 ml normal saline. They assess the patient as having a closed head injury and chest injuries. On arrival she is noted to be in respiratory distress. Auscultation of the chest reveals absent breath sounds over the left hemithorax and a hyperresonant percussion note. The trachea is displaced to the right. The peripheries feel cool to touch. She opens her eyes to voice, localises pain but is disorientated to time and place. Pupils are mid position and reactive to light. There is a large scalp laceration over the left temple and a bloody discharge noted to be oozing from the left ear. Vital signs: BP = 80/40 PR = 145/min - 24 - RR = 40/min Sat = 89% BSL = 4.5 mmol/l Question Discuss the immediate priorities in the management of this patient Answer 1 Immediate management follows the ABCD approach and in this case will focus on the respiratory distress, shock and altered conscious state of this patient. The ambulance has commenced the initial management with administration of oxygen via a mask, immobilization of the neck with a cervical collar, establishment of an IV access and administration of 500 ml normal saline. The airway should be assessed and any obstruction cleared using basic airway manoeuvres such as jaw thrust, suction of any foreign material / blood / vomitus and insertion of a guedel airway. Immediate decompression of the tension pneumothorax is required and this should be followed by insertion of a chest tube. Although the hypotension may be due to the tension pneumothorax IV fluid resuscitation should be commenced and if the hypotension does not improve following relief of the pneumothorax a 20ml/kg bolus of fluid should be given rapidly and the patient reassessed. Other interventions required will include : A second (large bore) IV access Drawing bloods for CBP, EUC, G&M Monitoring – cardiac, BP, oximetry Critical Interventions Decompression of the tension pneumothorax Insertion of a chest tube IV fluid resuscitation Case Study 11 con't A large bore IV cannulae is placed in the left second intercostal space, midclavicular line and a sudden rush of air escapes from the chest. The respiratory distress and saturations of the patient are markedly improved. Arrangements are made to place a chest tube. The patient’s circulatory status shows no sign of improvement and an IV bolus of 1500 ml (20 ml/ kg) of normal saline is rapidly infused. A second IV access is inserted and blood drawn for CBP, EUC and G&M. Routine monitoring is attached. The patient’s vital signs are checked. PR = 90 / min BP=120/80 Saturation = 98%. Following insertion of the chest tube the patient becomes irritable and tries to pull out her IV lines before eventually “calming down” after 5 minutes . A short while later her blood pressure is noted to be 180/120 and her pulse 40 / min. When the nurse checks her pupils the left pupil is noted to be much larger than the right and unresponsive to light. A painful stimulus fails to illicit a response from the patient. Question What immediate management is necessary ? Answer 2 The patient has a severe head injury (a base of skull fracture and a possible extradural is likely) with evidence of critically raised intracranial pressure Discuss the signs of raised intracranial pressure. Often only one or two of the signs are present early on and include - 25 - Unilateral dilated pupil - not reactive to light Depressed conscious state Asymmetrical reflexes Altered respiratory pattern (eg hyperventilation, irregular) Hypertension and bradycardia (unreliable and occurs late) Immediate management of the head injury will involve intubation and assisted ventilation (to protect the airway and lower raised intracranial pressure). Mannitol (2.5 ml / kg over 20 to 30 minutes) may be necessary if the pupil remains dilated despite ventilation but often is administered in consultation with the neurosurgeon. Urgent decompression of the extradural/ subdural haematoma will be requi red. How and where this happens depends on the resources and location of the rural hospital. Other priorities in management will be to identify other injuries, however the head injury requires immediate priority and there should be no delay for any necessary transfer / retrieval to a neurosurgical facility. The cause of the hypovolaemic shock has yet to be identified with abdominal injury the most likely cause although long bone fracture, pelvic fracture (and retroperitoneal bleed) or haemopneumothorax are other possibilities. In view of the head injury a cervical spine injury is also a high risk. Critical Interventions Immediate intubation and assisted ventilation Rapid transfer to a neurosurgical facility Dysrhythmia Case Study 12 Aims Discuss the priorities in assessment of a patient presenting with a dysrhythmia Review the ECG features and management of ventricular tachycardia Discuss the management of cardiac arrest Synopsis A 48 year old patient presents with ischaemic chest pain which is complicated by the development of ventricular tachycardia and subsequently has a cardiac arrest. Full Case Study # 12 You are contacted by the nurse from the local (rural) hospital to review a 48 year old male patient who has presented to the local (rural) hospital with a thirty minute history of acute severe central chest pain. An ECG is performed and shows sinus rhythm and an acute anterior myocardial infarction. In accordance with the hospital protocol the patient has been given SL GTN and Aspirin, an oxygen mask is applied and the patient placed on a cardiac monitor. Before you reach the hospital he complains of feeling dizzy and appears very pale. A second ECG is performed. You arrive as the ECG is being completed. Vital signs BP 80 / 40 PR > 150 / min RR = 32 / min Question Interpret the ECG. Outline how you would manage this patient. Answer 1 ECG shows a broad complex regular tachycardia, (most likely Ventricular Tachycardia) Ensure oxygen mask is placed. Insert IV. Check cardiac monitor. The patient needs urgent treatment as in the setting of ischaemia this rhythm may rapidly deteriorate to VF. The patient’s haemodynamic status needs to be urgently assessed to determine management of the dysrhythmia. Where the patient shows evidence of instability urgent cardioversion is required. - 26 - Instability is suggested by an altered conscious state (suggesting in adequate CNS perfusion), hypotension, severe respiratory distress (due to pulmonary oedema) or severe chest pain (suggesting myocardial ischaemia). If the patient is stable drug management of this arrhythmia may be considered. A variety of antiarryhthmic agents may be chosen for stable VT including lignocaine, sotalol, procainamide, amiodarone. In this case the patient is unstable (BP = 80/40) and the patient requires immediate cardioversion. Critical Interventions Assess stability of the patient Immediate cardioversion Case Study # 12 con't While preparations are made for cardioversion the patient becomes unresponsive and the monitor shows a completely chaotic irregular rhythm. The patient is unresponsive, apneic and has no pulse palpable carotid pulse. Question Interpret the ECG. Outline how you would manage this patient. Answer 2 The patient is in cardiac arrest (likely VF). CPR should be commenced and immediate defibrillation performed using 200J (repeat 200J and then 360 J if unsuccessful) Follow standard CPR protocols Question If your resuscitation is successful and the patient has returned to a normal conscious state outline your management and disposition of the patient ? Answer 3 As a further cardiac arrest is a high risk, the patient will require continued monitoring in a coronary care environment with nursing staff trained in the recognition and treatment of cardiac arrhythmias. Discussion of the case with a cardiologist would also be appropriate to determine further management and whether transfer is warranted to a major hospital for invasive cardiology. Use this opportunity to discuss the individual circumstances of the participants with respect to sources of referral and assistance available to them if faced with a case such as the one under discussion. Violent Patient Case Study 13 Aims Describe the presentation of a potentially violent patient Review the options in managing a violent patient Review the assessment of organic brain syndrome in the patient with altered behaviour Synopsis A 25 year old man is brought to the local hospital by police after acting strangely. He is extremely agitated and appears to be experiencing visual hallucinations. The management focuses on controlling for the risk of violence and identifying / managing the underlying cause. Full Case Study # 13 One Saturday evening the nurse from the local hospital informs you of the arrival of a 25 year old psychiatric patient who has been brought in by the police for psychiatric review. He had been found wandering across the park with his trousers down shouting out obscenities. Although the patient is not known to you and lives outside the area, he has visited the hospital on a previous occasi on two years ago. At this visit he was noted to have schizophrenia and managed with antipsychotic depot injections. No other history is known. - 27 - On examination you find the man to be alert but extremely agitated. He is diaphoretic and appears to be experiencing visual hallucinations. Question How will you approach the initial management of this patient? Answer 1 There is a real potential for an outbreak of violence and initial management should be to control the situation and protect staff (and the patient) from the risk of injury. The patient’s condition may not allow control through discussion or reason (ie talking down) although provided he is not openly aggressive/threatening this should always be attempted first. The principles in this situation is to fi rstly ensure other personnel/assistance are immediately available if required, always to keep a safe distance, never allow the patient to get between you and the door, take a nonthreatening posture, avoid looking the patient in the eye, offer a drink or a meal, attempt to diffuse the anger by encouraging the patient to verbalise their concerns and explain you would like to help him and wish to understand the way he is feeling at the moment. A show of force should be tried if talking the patient down is unsuccessful in achieving co-operation. Where talking fails to achieve co-operation or the patient becomes threatening or physically violent, physical restraint will be required. Optimally at least four (preferably five) people are required to undertake the restraining procedure. If available, shackles may assist the physical control of the patient while pharmacological restraint is being initiated. Discussion with the “team” before the procedure will ensure everyone is familiar with their role. Completion of a detention order will also be required. After explaining to the patient what will happen the patient should physically restrained and IV/IM sedation (eg midazolam) administered. Critical Interventions Control the violence Case Study # 13 con't After an explanation to the patient and completion of a detention order, the patient is physically restrained and an IV inserted. IV Midazolam titrated at 1 to 2 mg at a time every 2 – 3 mins is administered to a total of dose of 7 mg. The patient relaxes and lies quietly with their eyes closed but opens them with a gentle physical stimulus. Question How will you proceed to assess this patient? Answer 2 An underlying organic cause for the patient’s altered behaviour needs to be excluded. The following should therefore always be checked ABCDs Vital signs Oximetry Blood Glucose Pupils (signs of raised ICP, toxic ingestion) Reflexes Signs of head injury (or other injury suggesting a fall) Meningism (provided trauma is first excluded) Urinalysis Organic causes for altered behaviour / violence / agitation that need to be considered include infection (especially CNS such as meningitis/encephalitis), intracerebral bleed (eg SAH), trauma (eg subdural haematoma), endocrine/metabolic (eg hypoglycaemia) and drug related (eg withdrawal, overdose, drug abuse). Management of the patient with organic brain syndrome should generally include ABCDs, oxygen mask, monitoring (cardiac, oximetry, BP), establishment of an IV line / fluids, drawing of routine - 28 - bloods (EUC & calcium, CBP, serum alcohol), ECG and consideration given to the administration of IV dextrose (depending on the clinical circumstances). Critical Interventions ABCDs Vital signs Blood Glucose level Pupillary examination Urinalysis Gynaecological Emergency - Case 14 Aims Review the assessment and treatment priorities in a patient presenting with first trimester bleeding Discuss differential diagnosis of first trimester bleeding Discuss the management of life-threatening PV bleeding in early pregnancy Synopsis A 19 year old female who is 7 weeks pregnant presents to the local (rural) hospital with acute lower abdominal pain and PV bleeding. She is in shock and requires fluid resuscitation. Examination identifies POC in the cervical os. Full Case Study # 14 A 19 year old female presents to the local (rural) hospital with acute lower abdominal pain and PV bleeding. A urine pregnancy test performed a fortnight ago was positive. Her last period was 7 weeks previously and she reports that her periods have been regular with a 28 day cycle. This is her first pregnancy and she has no significant past medical history. She reports that she had been experiencing a small amount of dark PV spotting over the past two days which had then become increasingly heavy over the past 12 hours to a bright red loss with clots. She had also simultaneously developed moderately severe crampy abdominal pain worse on the right side. She reports that she feels faint if she tries to stand. Vital signs are PR 120/ min BP 100/60 RR 30/min T 36.5 On examination the patient is pale and is distressed by the pain. The peripheries are cool to touch and there is delayed capillary refill. Abdominal examination reveals a tender lower abdomen but no obvious guarding. Questions Outline the immediate management priorities What diagnoses need to be considered? Answer 1 The patient is showing signs of haemodynamic instability and this requires Oxygen mask Immediate establishment of IV access (preferably two large bore cannulae). Bloods should be taken for CBP, G&M and ßHCG (and possibly coagulation studies to identify DIC). Assess haemodynamic status (check for cool peripheries, decreased capillary refill, postural hypotension) Where haemodynamic instability is confirmed give 20 ml / kg fluid bolus. Proceed to examination including a VE to identify state of the cervical os, cervical excitation, presence of adnexal tenderness or palpable mass. - 29 - There are many causes for PV bleeding in first trimester. The major diagnoses to be considered in this patient however are incomplete/inevitable abortion and ectopic pregnancy. Case Study # 14 con't An oxygen mask is placed on the patient. An IV access is established and an initial bolus of normal saline 20 ml/kg administered rapidly. Bloods for CBP, G&M and ßHCG are taken. The patient is placed on a cardiac monitor. When the vaginal examination is attempted a large amount of fresh blood pours out from the vagina and products of conception noted in the open cervical os. The patient is very pale. Question What is the diagnosis? How would you control the PV bleeding? Answer 2 This patient has an incomplete abortion. Massive bleeding may sometimes occur and usually due to retention of the POC in the cervical os preventing it from closing. The management consists of IV fluid resuscitation, removal of the POC from the cervical os and administration of IV Oxytocin 10 Units (or Ergometrine 0.5 mg) followed by an Oxytocin infusion (40U oxytocin in 1000 ml NS over 4 hours). Urgent D&C will be required. Rhesus status should also be checked and if negative anti D administered. - 30 -