Welk PA in Children for Measurement Class
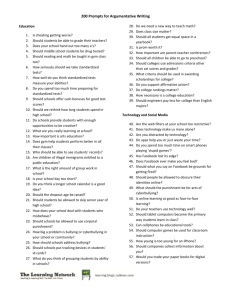
advertisement

Measurement Issues in the Assessment of Physical Activity in Children Keywords: self-report, activity monitors, observation, validity, activity patterns Gregory J. Welk, Charles B. Corbin and Darren Dale The health benefits of physical activity for adults have been well established (U.S. Department of Health and Human Services, 1996). Similar links with children are not as well established since it takes time for unhealthy behaviors to influence chronic disease. Nevertheless, there has been tremendous interest in assessing and promoting physical activity among children. Much of this interest stems from the highly publicized increases in the prevalence of pediatric obesity (Gortmaker, Dietz, Sobol, & Wehler, 1987; Troiano, Flegal, Kuczmarski, Campell, & Johnson, 1995; Troiano & Flegal, 1998). Studies have documented the important role that physical activity plays in weight control (Rippe & Hess, 1998) and significant tracking coefficients have been observed for obesity (Whitaker, Wright, & Dietz, 1997), coronary risk factors (Mahoney, Lauer, Lee, & Clarke, 1991) and physical activity/inactivity (Pate, Baranowski, Dowda, & Trost, 1996; Pate et al., 1999) among youth. To advance work in these (and other) areas, and further the promotion of physical activity in children, continued efforts are needed to improve our ability to assess this complex behavior. There are a number of different techniques that have been used to assess physical activity in a variety of populations (self-report, activity monitors, pedometers, heart rate monitors, doubly labeled water, and indirect calorimetry) and others that have been developed specifically for children (direct observation). Each of the measures has specific advantages and disadvantages that must be considered when selecting an instrument. A number of excellent reviews of physical activity assessments have described the relative merits of the different approaches for adults (Ainsworth, Montoye, & Leon, 1994; Melanson & Freedson, 1996; Wareham & Rennie, 1998) as well as for children (Baranowski & Simons-Morton, 1991; Baranowski et al., 1992; Pate, 1993; Riddoch & Boreham, 1995; Rowlands, Eston, & Ingledew, 1997). Detailed information on each of the assessment techniques is also available in other articles in this supplement. The purpose of this paper is to describe the measurement issues that complicate assessments of physical activity specifically in children. Some of the issues are common measurement challenges for any population but other factors stem from the unique developmental and behavioral aspects of children. Emphasis in this paper is on issues for pre-adolescent children since challenges in activity assessments are greater for younger children. While many issues remain for adolescents, they tend to become cognitively and behaviorally more similar to adults by the time they reach high school. By narrowing the focus to younger children we hope to address the substantive issues for assessments in young children in greater detail. Central to the understanding of accurate assessment techniques of any population is a clear understanding of the nature of the individual or individuals being studied. Therefore, we will first describe the unique aspects of children’s movement patterns and how these patterns influence the various measurement approaches used to assess physical activity. Next, we will review current physical activity guidelines for children and clarify why it is important to use appropriate criteria when making determinations about the physical activity levels of children. Finally, we will review some of the more common physical assessment tools to determine the usefulness of each in studying children’s physical activity. Table 1. Characteristics That Differentiate Children From Adults in Physical Activity Type Characteristic Implication Biological Need for high level of central nervous system arousal •High volume of physical activity is typical •Low tolerance for total inactivity •Spontaneous activity is common Cognitive Functioning More concrete (less abstract) thought process •Relatively short attention span on any given task •Less interest in continuous activity •Failure to see long term benefits of activity (e.g.health benefits) Less developed cognition •Less accurate recall •Inability to accurately estimate time Physiological Limited tolerance for vigorous •Activity typically intermittent in nature physical activity Weak relationship between fitness and physical activity •Effort (active behavior) does not necessarily result in increases in fitness thus positive feedback for active behavior is lacking Biomechanical Poorer economy and efficiency of movement •Quicker onset of fatigue, and need for frequent rest •Less interest in continuous activity Psychological: (the "kid" factor) More available free time •More time to try new activities Natural curiosity and desire for pursuing new tasks •Interest in exploring new activities Adapted from "Physical Activity for Children: A Statement of Guidelines for Physical Education for Children, 1998" (Council for Physical Education for Children, 1998) The Unique Nature of Children’s Physical Activity Patterns Several recent papers have provided insights as to the unique nature of children with respect to their propensity for physical activity. Rowland (1998) has suggested a biological basis for the differences in activity patterns between children and adults. Children, he notes, are inherently active primarily because it is physical movement that provides them with the necessary information required by the central nervous system for stimulation. Adults, on the other hand, achieve arousal of the central nervous system in a variety of non-locomotor activities such as reading, writing, artistic expression, problem solving, and vocational pursuits. The fact that children of nearly all animal species are more active than adult populations supports Rowland’s notion that children have an inherent biological need to be active. An observational study by Bailey et al. (1995) provides the most detailed insight into the nature of children’s activity habits. Using a coding system calibrated against indirect calorimetry, they recorded the intensity of children’s activity every 3 s over a 12-hour period. This frequent sampling allowed the authors to characterize the “tempo” of physical activity in children, which they described as the natural variation in rate and intensity of activity events as well as the intervals between activity events. The median duration of low and moderate intensity activities were 6 s while the duration for high intensity activities were 3 s. Nearly all bouts of vigorous activity (95%) lasted less than 15 s and only 0.1% of the bouts were longer than a minute. No bout of high intensity activity longer than 10 minutes was recorded. The median duration between high intensity activities was 18 seconds, but ranged between 3 s and 21 min. 15 s. Periods of rest were clearly long in proportion to periods of activity, but 95% of the ‘rest’ intervals were less than 4 min. and 15 s. This indicates that children do not remain inactive for extended periods of time. Collectively, these findings clearly document the highly transitory nature of children’s physical activity. The authors suggest that short, intermittent bouts of vigorous physical activity (with frequent rest periods of longer duration) are typical of children and, in fact, may be necessary for normal growth and development (Bailey et al., 1995). Table 2. A Summary of NASPE Physical Activity Guidelines for Children Guideline Elementary school children should accumulate at least 3060 minutes of age appropriate physical activity on all, or most days of the week. Implications •Children need longer periods of time in activity than adults (minimum standards). •Children are likely to accumulate activity in many intermittent activity bouts rather than single bouts of continuous activity. An accumulation of more than 60 minutes and up to several •Sixty minutes (see guideline 1) is a minimum hours per day of appropriate activities is encouraged for standard. school aged children. Some of the child's activity each day should be in periods lasting 10 to 15 minutes or more and include moderate to vigorous activity. This activity will typically be intermittent in nature involving alternating moderate to vigorous activity with brief periods of rest and recovery. •Some relatively long periods of time (at least 10-15 minutes) are necessary for children though activity need not be continuous or highly structured. •Both moderate and vigorous activity is necessary but is likely to be in intermittent spurts. Extended periods of inactivity are discouraged for children. •Activity sessions throughout the day are desirable and consistent with the developmental needs of children. A variety of physical activities from the Physical Activity Pyramid are recommended. •Children need variety to meet developmental needs and to retain interest in activity. Adapted from "Physical Activity for Children: A Statement of Guidelines for Physical Education for Children, 1998" (Council for Physical Education for Children, 1998) Consistent with Rowland’s and Bailey’s perspectives, the recent National Association for Sport and Physical Education (NASPE) guidelines on physical activity for children (Council for Physical Education for Children, 1998) focus on the volume of activity and emphasize that intermittent activity is more likely to characterize their behavior than continuous activity. This document also highlights a number of other cognitive and behavioral differences between adults and children that should be considered when studying or promoting physical activity in children (see Table 1). Each of the characteristics described in Table 1 also has implications for the assessment of physical activity. The fact that children have different patterns of activity (intermittent vs. continuous) necessitates that different intervals of assessment and/or outcome measures be used to assess their levels of activity. The less developed cognitive skills of children (characterized by concrete thinking) results in a lesser ability to effectively use self-report questionnaires. Biological differences in metabolism and biomechanical differences in efficiency and economy require different assumptions for measurement techniques that aim to estimate energy expended in physical activity. The implications of these various characteristics of children for each of the more common assessment techniques will be discussed later in this paper. Unique Activity Guidelines for Children Just as the unique characteristics of children should be considered when making decisions about the method of physical assessment so too should the unique expectations for children in activity be considered. The need to assess physical activity in any population is based on the desire to determine the current activity status of that population and to determine if that population is meeting activity criteria that are appropriate for optimal health and development. For years, the activity guidelines for children were assumed to be similar to those recommended for adults (American College of Sports Medicine, 1988; Rowland, 1985). These guidelines generally indicated that activity must be of vigorous intensity for continuous periods of time (20+ minutes) to provide benefits. Based on Karvonen’s method (at 60% of heart rate reserve), a heart rate of 159 or 160 was calculated as a target for children (Gilliam, Freedson, Geenen, & Shahraray, 1981; Sady, 1986). A consensus review of activity guidelines later indicated that heart rates of 139-140 were sufficient to define the threshold for activity in children (Simons-Morton, Parcel, O’Hara, Blair, & Pate, 1988). Both levels have been used in a number of studies to characterize children’s activity levels, but the level of 140 has had more widespread usage. Recently, there has been a shift toward the promotion of moderate-intensity physical activity for adults. This shift is based on the repeated observation that significant health benefits are obtained from modest levels of physical activity (U.S. Department of Health and Human Services, 1996). The concept of accumulating intermittent activity is clearly consistent with children’s normal movement patterns; however, most recommendations for ‘lifestyle physical activity’ are intended and designed for adults (e.g., incorporating stair climbing and yardwork activities into one’s daily routine). The Children’s Lifetime Physical Activity Model was proposed as an alternative for children (Corbin, Pangrazi, & Welk, 1994; Pangrazi, Corbin, & Welk, 1996). This model incorporates normal, intermittent free play as part of a child’s natural activity and specifies how much activity children need on a regular basis (see Table 2). The recent NASPE physical activity guidelines for children (Council for Physical Education for Children, 1998) are based conceptually and philosophically on this model. Similar guidelines for children have been developed in Europe (Health Education Authority, 1998). These guidelines should be considered by those interested in the study of physical activity in children. Those interested in the study of physical activity in adolescents are referred to guidelines established by a recent international consensus group (Sallis & Patrick, 1994). Table 3. Results of Selected Studies Characterizing Activity Levels in Children: A Comparison of Different Criteria and Measures. Lead Participants Methods Criterion Results Author Heart Rate Monitoring Studies Armstrong (1990) 163 boys and 107 girls ages 11-16 Continuous heart rate monitoring (12 hours) Armstrong (1991) 65 girls and 67 boys ages 10-11 Continuous heart rate monitoring (12 hours) Armstrong et 43 girls and 86 boys al. (1996) ages 10-11 Continuous heart rate monitoring (12 hours/day over 3 days) Gilliam (1982) 18 girls and 22 boys ages 6-7 Continuous heart rate monitoring (12 hours) Janz (1992) 76 girls and boys ages 6-17 Continuous heart rate monitoring (8-11 hours) % of children with HR > 139 for 20 consecutive minutes % of children with HR > 139 for 3, 5minute bouts Total number of minutes with HR > 139 (weekday) % of children with HR > 139 for 20 consecutive minutes % of children with HR > 139 for 3, 5minute bouts Total number of minutes with HR >139 (weekday) Girls: 12% active Boys: 23% active Girls: 53% Boys: 70% Girls: 32 minutes Boys: 45 minutes Girls: 34% active Boys: 39% Girls: 85% Boys: 90% Girls: 59 minutes Boys: 68 minutes % of children with HR > 139 for 20 consecutive minutes % of children with HR > 139 for 3, 5minute bouts % of children with HR > 159 for 3, 5minute bouts Total number of minutes with HR > 160 Total number of minutes with HR > 140 Girls: 9 minutes Boys: 21 minutes Girls: 30 minutes Boys: 56 minutes % of children with HR > 60% of age predicted max for 20 minutes Total number of minutes with HR > 60% of age predicted max ~ 155 bpm Total: 7% active Total: 15 minutes Girls: 37% Boys: 39.5% Girls: 88% Boys: 92% Girls: 70% Boys 79% Direct Observation Studies Baranowski (1987) 14 girls and 10 boys ages 8-12 Direct observation on two days (12 hours)1 Sleap (1992) 27 girls and 29 boys Direct observation2 % of children active for 20 consecutive minutes % of children active for 14 minutes with only 1 stop or break Total number of minutes of activity (reported for those who were "active") 8-13% of children 58-63% of children 61-71 total minutes of activity % of children active for 20 consecutive minutes % of children active for 10 consecutive minutes Total minutes of activity 14% of children active 46% of children active 88.5 minutes Self-Report Instruments Craig (1996) 49 girls ages 8-11 Self-report of previous year Average minutes per 96.7 minutes Minutes per day for treatment and control groups 1. 72-82 minutes 2. 89-99 minutes day in moderate activity ≥ 4 METs Gortmaker et al. (1999) 336 5th grade children Two activity assessments 1. 24 hr recall 2. 16-item survey Number of minutes of moderate physical activity ≥ 6 METs computed with two measures McMurray (1998) 45 children (25 girls and 20 boys) in grades 6-8 Computerized activity recall Number of minutes of physical activity (no specification of intensity) Girls: 85 minutes Boys: 67 minutes Myers (1996) 995 boys and girls ages 9-15 Self-Report of previous day (SAPAC) Number of minutes of physical activity Total: 168 minutes Ross (1985) National sample of 5th and 6th grade Parent report of child's activity3 % of children performing regular activity Number of minutes of physical activity Girls: 49% Boys: 56% Total: 102-120 minutes Number of minutes of moderate to vigorous activity a day Girls: 83 minutes Boys: 97 minutes Simons2410 3rd grade children Activity Interview with Morton (1997) a log Key for abbreviations: HR = heart rate; PA = physical activity, SAPAC = Self-Administered Physical Activity Recall 1 Activity defined as continuous slow or fast trunk movements 2 Activity defined as being commensurate with a heart rate of 140 bpm 3 Activity defined as "exercise involving large muscle groups in dynamic movement for periods of 20 minutes or longer 3 or more times a week." Characterizing Activity Levels in Children If the assessment of physical activity patterns of children is the goal, the standard used to define “being active” becomes highly relevant. Failure to use appropriate standards can lead to significant misinterpretations of both individual and group assessments of physical activity. Interpretations of studies on activity levels in children also can vary widely depending on what type of assessment is used. Some examples illustrating the importance of these issues for characterizing activity levels in children are provided below. Prior to the development of specific physical activity standards for children, many studies were conducted to evaluate the habitual activity levels of children. To provide objective information about activity patterns, a number of studies used heart rate monitors (Armstrong, Balding, Gentle, & Kirby, 1990; Armstrong & Bray, 1991; Armstrong, McManus, Welshman, & Kirby, 1996; Gilliam et al., 1981; Janz, Golden, Hansen, & Mahoney, 1992) or direct observation techniques (Baranowski, Hooks, Tsong, Cieslik, & Nader, 1987; Sleap & Warburton, 1992). While varying slightly across the studies, the criteria in nearly all studies emphasized sustained aerobic activity for at least 10 minutes in duration. The percentage of children defined as “physically active” ranged from 8 to 39% depending on gender and nationality of the sample (see Table 3) leading most authors to conclude that children do not perform enough activity to obtain significant health benefits. A different interpretation from these studies is possible when the data are examined using more current activity guidelines. In the two original studies by Armstrong and colleagues (1990, 1991), the majority of children (53-70% of 11-16-year-olds and 85-90% of 10-11-year-olds) had at least three 5-minute bouts of activity during the day. The total minutes spent at heart rates > 40 bpm ranged from 31-68 minutes. Using the criteria of minutes > 50% max heart rate (~ 149 bpm), other studies have reported means ranging from 29 minutes (MacConnie et al., 1982) to 70-80 minutes (Verschuur & Kemper, 1982). These mean levels of activity generally indicate that children perform a reasonable volume of activity during the course of the day. Table 4. Methods of Assessment and the Characteristics of Physical Activity That Can Be Assessed. Method of Measurement Questionnaire Units of Measurement Time segments (often 10, 15, 30 min segments Type of Output 1. 2. 3. 4. Frequency of PA Intensity of PA Duration of PA EE of PA Output Measure 1. 2. 3. 4. # of bouts > criterion level Number or % of bouts # minutes > criterion level Estimates based on METS Heart Rate Beats per minute 1. 2. 3. 4. Frequency of PA Intensity of PA Duration of PA EE of PA 1. 2. 3. 4. Motion Sensors Movement counts 1. 2. 3. 4. Frequency of PA Intensity of PA Duration of PA EE of PA 1. 2. 3. 4. Direct Observation Activity rating 1. 2. 3. 4. Frequency of PA Intensity of PA Duration of PA EE of PA 1. 2. 3. 4. Pedometers Step counts 1. 2. 3. 4. Frequency of PA Intensity of PA Duration of PA EE of PA 1. 2. 3. 4. # of bouts > criterion level Average HR per day or interval # minutes > criterion level Estimates from calibration equations. # of bouts > criterion level Average counts per day or interval # minutes > criterion level Estimates from calibration equations # of bouts > criterion level Number or % of bouts # minutes > criterion level Estimates based on METS NA NA Number of steps taken NA Doubly Labeled Water CO2 production 1. 2. 3. 4. Frequency of PA Intensity of PA Duration of PA EE of PA 1. 2. 3. 4. NA NA NA Total energy expenditure Indirect Calorimetry O2 consumption 1. 2. 3. 4. Frequency of PA Intensity of PA Duration of PA EE of PA 1. # of bouts > criterion level Average VO2 level Monitored time above threshold Total energy expenditure 2. 3. 4. Similar differences in interpretation are evident in the studies employing direct observation techniques. Baranowski et al. (1987) reported that only 8-13% of children were active continuously for 20 minutes, but 58-63% were considered active when less stringent criteria (14 minutes with one stop) were used. Sleap and Warburton (1992) found only 14% of children to be active for 20 consecutive minutes but 46% had at least one sustained bout for over 10 minutes. These discrepancies also suggest that children are more likely to perform more intermittent activity. If bouts of activity are used as a criterion measure, the duration to define a bout of activity should be no greater than 10 minutes. A number of studies have also used self-report instruments to characterize activity levels in the population, both for intervention and surveillance purposes. A number of studies reporting average minutes of activity per day are summarized to provide a comparison to the other studies using heart rate and direct observation (see Table 3). The mean minutes of activity in these studies ranged from 67 to 168 min. per day (Craig, Goldberg, & Dietz, 1996; Gortmaker et al., 1999; Myers, Strikmiller, Webber, & Berenson, 1996; Ross & Gilbert, 1985; Simons-Morton et al., 1997). Because the activity levels reported in these (and other) studies are consistently higher than those reported with other instruments, the general consensus is that there is a consistent overestimation of activity using self-report instruments. This tendency was described in a comprehensive review of different surveillance instruments (Pate, Long, & Heath, 1994). It has also been noted in other studies comparing self-reports to other objective measures (McMurray, Harrell, Bradley, Webb, & Goodman, 1998; Simons-Morton, Taylor, & Huang, 1994). While some degree of overestimation from self-report forms may be attributed to an exaggerated perception of time and effort, a certain amount can also be attributed to the sporadic nature of children’s activity patterns and the nature of children themselves. Children may indicate that they were active while playing a sport or game but may have only been moving for a portion of the time. This is a more typical pattern of activity for children and the concrete thought processes cause them to view even short bouts of activity as significant. It is difficult to speculate on the degree of overestimation in children and it is also not clear if it is a consistent trend for all children or just some. Specific efforts in some studies have been made to avoid this type of overestimation (Simons-Morton et al., 1997); however, it is not clear how they influenced the results. Collectively, these comparisons reveal that the results of activity monitoring studies can vary greatly depending on how activity is measured and interpreted. This variability makes it difficult to make any firm conclusions about activity levels in children. Generalizing information about activity levels from group data is also complicated by the large inter-individual variability in activity habits among children. Using the studies reviewed in Table 3, the coefficients of variation (SD / mean) were generally found to range from 50%-93% for the various studies employing self-report measures (these values were not calculated for the heart rate and observation studies due to small sample sizes). Activity patterns from children also tend to be positively skewed. Thus, the mean values for an assessment may be biased by a few children performing a lot of physical activity or a large number performing very little. To provide a more comprehensive view of activity patterns, investigators are encouraged to report the median as well as the inter-quartile ranges in their data, in addition to traditional descriptive statistics. A number of specific measurement issues influencing each of the assessments will be described in more detail in the subsequent section. Measurement Issues for Assessing Physical Activity in Children As conventionally defined, the term ‘physical activity’ refers to “any bodily movement produced by skeletal muscles that results in energy expenditure” (Caspersen, Powell, & Christenson, 1985). In actual practice, the specific operational definition of physical activity depends on how it is measured and scored. The variables of frequency, intensity, and duration are commonly used to characterize activity patterns; another variable of interest is energy expenditure that is a summary variable that incorporates all of the other indicators. Table 4 lists the various methods and highlights the units of measurement and the conversions required for calculation of these components. The frequency of physical activity participation is typically reported as number of bouts per day or week or the percentage of children being active on a given day. Obtaining these values requires an appropriate criterion to define what constitutes “regular activity” and what counts as a ‘bout’ of activity. As previously described, criteria that are based on more structured, adultpatterns of activity (3 or more bouts of continuous activity for 10 or 20 minutes) are not appropriate for children. A better criterion to define frequency would emphasize the accumulation of intermittent activity throughout the day. Depending on the approach used, an appropriate criterion for children may be the percentage that report 2-3 bouts of short, intermittent activity totaling 30-60 minutes on at least 5 days a week. Because of the large intraindividual variability in activity, conclusions about typical activity patterns should not be drawn from 1 or 2 isolated days of measurement. The intensity of physical activity is often used to categorize physical activity but is not commonly used as an outcome measure. Several studies have reported mean heart rates or mean activity counts during the day or portion of the day (Janz et al., 1992; Janz, 1994). While this may be useful for statistical comparisons, the values themselves are difficult to interpret. Because the majority of a child’s day is spent in resting or light activities, mean values would be low and would not provide meaningful information about their true activity level. If mean levels were reported for a group, the large intra-individual variability in activity patterns in children would make interpretations of the data even more difficult. The duration of activity is generally reported in minutes or percentage of time spent being active. Alternately, the amount of activity may be calculated in conjunction with intensity categories. For example, it is common to see breakdowns of the number of minutes spent in different activity categories (light, moderate, or vigorous). With observational measures and self-report instruments, the distinctions among activity levels are established a-priori according to a specific coding strategy or established categories on a questionnaire. For heart rate and motion sensing devices, cutpoints must be established by comparing the activity values against data from other measures (e.g., heart rate or VO2). Obtaining energy expenditure estimates from physical activity requires information about the metabolic costs of the activities that are performed. For indirect calorimetry and doubly labeled water techniques, these measures are made directly according to established metabolic calculations. For observation and self-report measures, estimates are typically made using multiples of resting metabolic rate (METS). Because the MET values for various activities are not well established for children (Ainsworth et al., 1993), the estimates using these calculations may not be highly accurate. For heart rate and motion sensors, a calibration equation is needed to convert the raw unit of measurement into energy expenditure values. These equations are typically developed under lab situations using structured activities and may not generalize to field-based activities. Thus, these estimations must also be interpreted with caution. It is apparent from Table 4 that a number of different approaches can be used to obtain a similar outcome measure. The ease and accuracy of assessing these different components varies among each of the instruments. The advantages, disadvantages, and specific measurement issues for assessing children’s activity behaviors will be described below. Self-Report Instruments Self-report instruments provide a convenient way to assess activity patterns on large populations. While they have been commonly used for a variety of research purposes, there is widespread concern about the accuracy of self-report data from children. Most validation studies with children have reported only moderate correlations between various self-report forms and other objective criteria (Sallis, 1991). The lack of strong correspondence and the described tendency for overestimation have led to the consensus that children can not provide accurate self-report information about their activity patterns. Efforts have been made to describe the cognitive and methodological issues plaguing self-report instruments (Baranowski et al., 1984), but little is known about the specific cognitive skills required for children (or adults) to accurately complete self-reports (Baranowski, 1985; Baranowski, 1988; DuRant & Ainsworth, 1996). While a number of different approaches have been tested, the consensus from several reviews (Pate, 1993; Sallis, 1991; Sallis, Buono, Roby, Micale, & Nelson, 1993) is that previous-day recall instruments offer the most promise for use with children. A number of different instruments are now available for this type of assessment (Garcia, George, Coviak, Antonakos, & Pender, 1997; Sallis et al., 1996; Weston, Petosa, & Pate, 1997). A limitation of this format is that data must be obtained on multiple days in order to take into account the normal intraindividual variability in activity patterns. Because these instruments typically rely on a checklist of activities and coded intervals of time these instruments may be more susceptible to overestimation than other more general measures of activity. To avoid this type of error, some investigators recommend recording the number of “activity blocks” recorded by the participant rather than the time (Trost et al., 1996; Weston et al., 1997). Others have converted the data into an activity index that incorporates intensity and duration (Going et al., 1999). If the intent is to characterize general activity habits, alternative formats that do not require estimates of time or amounts of activity may be useful. The Physical Activity Questionnaire for Children (Crocker, Bailey, Faulkner, Kowalski, & McGrath, 1997), for example, uses a series of questions about general activity patterns to calculate an overall activity score. While the score does not allow for estimations of frequency, intensity, or duration, it may be useful in discriminating between active and inactive children. While self-report instruments have inherent limitations, there is considerable room for improvement in the way they are validated, scored, and interpreted (Baranowski, 1985). The increased use of computerized instruments offers promise to assist with recall and coding of activity. A computerized activity assessment (ACTIVITYGRAM) is now available with the recently released version of FITNESSGRAM software (Cooper Institute for Aerobics Research, 1999). The use of electronic beepers may also be useful to prompt recall of activity in children. Regardless of what format is used, results will likely be improved if more attention is given to the setting for the assessment and the training needed for children to accurately complete the assessment. A description and copy of a number of different self-report instruments for children have recently been published to facilitate their use by both researchers and teachers (Welk & Wood, 2000). Heart Rate Monitors Heart rate monitors provide an objective indicator of the physiological effect of physical activity. They have been found to provide a valid measure of heart rate in children (DuRant et al., 1993; Treiber et al., 1989), and heart rate has been shown to be linearly related to VO2 and energy expenditure during physical activity. However, the numerous other factors that influence heart rate under resting conditions contribute considerable error when heart rate monitors are used for extended periods of monitoring. In a recent study (Welk, Corbin, & Kampert, 1998), we found that heart rate indicators were highly correlated with a direct observation measure under active conditions in physical education (r = .79), but weakly correlated under inactive conditions in the classroom (r = .49). While this type of error would bias measures of mean heart rate, they would not affect estimates of total minutes of activity (e.g., minutes > 140 bpm). Still, there are a number of difficulties inherent in using heart rate monitors for field-based research (Riddoch & Boreham, 1995). Problems with 60-cycle interference and lost data from signal interruptions make data collection and data processing challenging. Delayed heart rate responses and the influence of other factors can add considerable error to heart rate recordings. Discomfort from wearing a transmitter device can also reduce participant compliance. Figure 1. Hypothetical diagram illustrating the potential variability in activity patterns within a minute for a child. Because children's activity is highly sporadic and intermittent, short bouts of activity would be averaged with rest breaks to represent the activity level for the minute. If activity cutpoints based on steady-state activity are used, the minute may be scored as "inactive" despite the presence of some vigorous activity. A promising application of heart rate monitoring techniques is for estimations of energy expenditure and for studies on obesity and weight control (Livingstone, 1997). Using individualized HR: VO2 regression equations and techniques that control for errors caused by variability in resting heart rate, a number of studies have demonstrated strong predictions for energy expenditure in children (Livingstone et al., 1992; Spady, 1980; Treuth, Adolph, & Butte, 1998). Another promising option is the potential use of heart rate along with a motion sensing device. Several studies have demonstrated that this can improve prediction of energy expenditure in both adults (Haskell, Yee, Evans, & Irby, 1993; Luke, Maki, Barkey, Cooper, & McGee, 1997; Moon & Butte, 1996) and children (Eston, Rowlands, & Ingledew, 1998). Activity monitors Activity monitors provide an objective indicator of total body movement. Because most contemporary monitors feature time sampling capability, they can be used to assess the frequency, intensity, duration, and energy expenditure of physical activity. Numerous studies have examined the reliability and validity of these devices in children, under both lab (Trost, Ward, & Burke, 1998) and field conditions (Eston et al., 1998; Janz, 1994; Welk & Corbin, 1995). Similar to studies with adults, the general consensus is that they provide valid measures of physical activity but more questionable estimates of energy expenditure. A well-described limitation of activity monitors is the inability to assess upper body activities such as throwing, catching, carrying, or lifting. Recent studies have documented that activity monitors significantly underestimate energy expenditure of common lifestyle activities in adults (Bassett et al., in press; Hendleman, Miller, Bagget, Debold, & Freedson P.S., in press; Welk, Blair, Wood, Jones, & Thompson, in press). While similar studies have not been conducted specifically in children, it is likely that activity monitors would also underestimate the energy expenditure estimates of children’s intermittent activities. The use of 3-dimensional devices (e.g., Tritrac) would appear to offer advantages over 1-dimensional devices but the results have been equivocal (Bouten, Verboeket-Van De Veene, Westerterp, Verduin, & Janssen, 1996; Bouten, Koekkoek, Verduin, Kodde, & Janssen, 1997; Welk & Corbin, 1995). Field-based calibration equations may improve the predictive accuracy of monitors; however, the large individual errors associated with these estimates would make individual comparisons problematic. By reporting raw movement counts or using a different outcome variable (e.g., minutes of activity), the errors associated with energy expenditure estimations would be avoided. One of the most common approaches for field-based research is to use “cutpoints” to determine the amount of time spent in different intensity categories (Janz, 1994). While this is a useful approach, it is important to recognize that cutpoints will underestimate activity levels in children if they are established based on the number of counts recorded during a continuous bout of activity. Because most accelerometry-based devices use an integrative procedure to summarize movement counts, the value at the end of the minute reflects the total counts within that time. Thus, short periods of vigorous activity may be obscured by alternating periods of rest when the total value for the minute is computed (Dale, 1999). Activity values for these minutes could be interpreted as “inactive” time periods if the cutpoints are based on how many counts would accrue during continuous activity (see Figure 1). To avoid this potential error, cutpoints must account for the intermittent nature of children’s physical activity behavior. From this perspective, direct observation techniques using momentary time sampling procedures may provide the best criterion measure since they can address changes in activity levels within a minute. Another option is to process activity monitor data using time intervals less than 1 minute. Currently the CSA monitor is the only device that allows settings in this range. While there are limitations, activity monitors are one of the most useful tools to assess physical activity over extended periods of time. The cost and administrative time may be too high for large-scale studies, but they can be useful for smaller intervention studies, cross sectional comparisons, or validation of other assessment techniques. Pedometers Pedometers provide an objective indicator of step counts, a marker of total volume or duration of activity. They possess similar benefits and weaknesses to motion sensors but with less accuracy and precision. Because pedometers do not have time sampling capabilities, they cannot provide detail on frequency or intensity of physical activity. Energy expenditure estimates would likely be inaccurate due to the many assumptions needed to calculate this from step counts. Still, in terms of practicality, pedometers may offer the best solution for a low cost, objective monitoring tool. Recently, similar correlations with fitness and fatness measures were reported between pedometers and a Tritrac monitor (Rowlands, Eston, & Ingledew, 1999). The correlations between pedometer counts and the Tritrac measure ranged from .85 to .88. Similar findings have been reported in several other studies (Eston et al., 1998; Kilanowski, Consalvi, & Epstein, 1999). A recent study in adults (Welk et al., in press) suggested that 10,000 steps is a reasonable daily target for adults but similar studies are needed to determine guidelines for children. Direct Observation Direct observation techniques evaluate the behavioral aspects of physical activity and are well suited to studies on children. The merits of various instruments and coding strategies have been previously described (McKenzie, 1991). While considerable time and effort is required to conduct direct observation studies, the detail provided can be highly useful for characterizing children’s activity. Direct observation techniques provide one of the best criterion measures to validate other assessment tools. For further information, readers should consult the specific protocols published with each instrument. Indirect Calorimetry and Doubly-Labeled Water Indirect calorimetry and doubly-labeled water techniques are considered to be the respective gold standard assessments for lab and field-based studies on physical activity. Under controlled conditions, indirect calorimetry can be used to partition energy expenditure associated with resting metabolic rate (RMR), the thermic effect of food (TEF), and the thermic effect of exercise (TEE). These variables are useful for understanding relationships between energy expenditure and weight control. Doubly-labeled water assessments yield a direct measure of carbon-dioxide production that, when combined with the food quotient of the diet, yields highly accurate estimates of energy expenditure. Doubly-labeled water has several advantages for assessing total daily expenditure in children. It is non-invasive, can measure activity over 1-2 week periods, and does not interfere with normal activity patterns. The limitations are the cost and the difficulty in obtaining the stable isotopes of water. It is also not useful for examining patterns of activity or for partitioning energy expenditure associated with physical activity. Interested readers are referred to more detailed descriptions of these techniques and their applicability for research on children (Goran, 1995; Hill, Johnson, Melby, & Peters, 1995; Westerterp & Goran, 1997). Summary This paper reviewed the nature of children’s physical activity patterns and how the unique nature of children can impact the assessment of physical activity. To accurately assess children’s activity patterns, an instrument must be sensitive enough to detect, code, or record sporadic and intermittent activity. Care also must be used to select criterion measures that reflect appropriate physical activity guidelines for children. A number of different measurement approaches have been described for assessing children’s activity, but no specific method can be identified as the best option for all studies. Selection of an appropriate instrument depends on the specific research question being addressed as well as the relative importance of accuracy and practicality (Baranowski & Simons-Morton, 1991). For example, accurate measures of energy expenditure using doubly-labeled water, indirect calorimetry, or heart rate calibration equations may be needed for certain clinical studies, but the cost and inconvenience would make them impractical for field-based assessments on larger samples. The “accuracy-practicality” trade-off presents a more challenging predicament with children than for adults. In adults, a number of self-report instruments have been found useful for large epidemiological studies or interventions where less precision is needed. Because of developmental differences, especially in ability to think abstractly and perform detailed recall (Going et al., 1999; Sallis, 1991), children are less likely to make accurate self-report assessment than adults. Though self-report methods are still likely to be a principal source of information for many studies, other approaches (or the use of combined measures) may be needed to better characterize children’s activity levels. While objective instruments (e.g., direct observation or activity monitoring) require more time and resources than self-report, there are options available to simplify data collection. One approach may be to focus assessments on key times or places that allow children to be active. The time after school, for example, appears to be a critical period that defines their propensity for physical activity (Hager, 1999). Monitoring of entire groups for discrete periods of time (e.g., recess or physical education) may also be useful to understand variability in activity patterns since children would all be exposed to the same stimulus or opportunity to be active. Proxy measures may also be useful in studying activity in children. For example, several studies (Baranowski, Thompson, DuRant, Baranowski, & Puhl, 1993; Sallis et al., 1993) have demonstrated that time spent outside is strongly predictive of activity in children. Involvement in community sports programs may also be a useful proxy measure as sports programs have been found to account for approximately 55-65% of children’s moderate to vigorous activity (Katzmarzyk & Malina, 1999). Another option for improving assessments in children is to employ multiple measures of physical activity. A number of studies (Coleman, Saelens, Wiedrich-Smith, Finn, & Epstein, 1997; McMurray et al., 1998; Sallis et al., 1998; Simons-Morton et al., 1994) have reported differences in levels of activity when activity monitors were compared with self-report data. The method of measurement has also been shown to influence the results of studies on the determinants of physical activity in children (Epstein, Paluch, Coleman, Vito, & Anderson, 1996). While we do not currently know which measure is most accurate, reporting the results with different instruments provides a more complete description of children’s activity and permit a triangulation of outcomes. In summary, there remains no single way of obtaining a highly accurate account of physical activity or energy expenditure in children. The nature of children’s movement patterns, the various types of activities engaged in, and the inherent limitations of each assessment tool limit the ultimate accuracy of these measurements. Future research should continue to characterize children’s movement patterns so that better assessment techniques can be developed. Wareham and Rennie (1998) provided a strong rationale for continued efforts to improve assessment techniques for epidemiological research. They point out that relatively weak measures were probably sufficient to demonstrate general health benefits of physical activity, but that more sophisticated techniques are needed to answer the more complex research questions currently facing the field. This is especially true for research with children since links with specific health outcomes are difficult to establish and variability in cognition and maturation complicate other outcomes. A review of physical activity interventions in children (Stone, McKenzie, Welk, & Booth, 1998) also highlighted the importance of valid and reliable measures to assess change in physical activity behaviors over time. To advance research in pediatric exercise science it is important to continue work to improve current physical activity assessment techniques. REFERENCES Ainsworth, B.E., Haskell, W.L., Leon, A.S., Jacobs, D.R., Jr., Montoye, H.J., Sallis, J.F., & Paffenbarger, R.S., Jr. (1993). Compendium of physical activities: classification of energy costs of human physical activities. Medicine and Science in Sports and Exercise, 25, 71-80. Ainsworth, B.E., Montoye, H.J., & Leon, A.S. (1994). Methods of assessing physical activity during leisure and work. In C. Bouchard, R.J. Shephard, T. Stephens, J. R. Sutton, & B. D. McPherson (Eds.), Assessing Physical Activity During Leisure and Work (pp. 146-159). Champaign, IL: Human Kinetics. American College of Sports Medicine. (1988). Physical fitness in children and youth. Medicine and Science in Sports and Exercise, 20, 422-423. Armstrong, N., Balding, J., Gentle, P., & Kirby, B. (1990). Patterns of physical activity among 11-16-year-old British children. British Medical Journal, 301, 203-205. Armstrong, N., & Bray, S. (1991). Physical activity patterns defined by continuous heart rate monitoring. Archives of Disease in Childhood, 66, 245-247. Armstrong, N., McManus, A., Welshman, J., & Kirby, B. (1996). Physical activity patterns and aerobic fitness among prepubescents. European Physical Education Review, 2(1), 19-29. Bailey, R.C., Olson, J., Pepper, S.L., Porszaz, J., Barstow, T.L., & Cooper, D.M. (1995). The level and tempo of children’s physical activities: An observation study. Medicine and Science in Sports and Exercise, 27, 1033-1041. Baranowski, T. (1985). Methodologic issues in self-report of health behavior. Journal of School Health, 55(5), 179182. Baranowski, T. (1988). Validity and reliability of self-report measures on physical activity: An information processing perspective. Research Quarterly for Exercise and Sport, 59, 314-327. Baranowski, T., & Simons-Morton, B.G. (1991). Children’s physical activity and dietary assessments: Measurement issues. Journal of School Health, 61, 195-197. Baranowski, T., Bouchard, C., Bar-Or, O., Bricker, T., Heath, G., Kimm S.YS., Malina, R., Obarzanek, E., Pate, R., Strong, W.B., Truman, B., & Washington, R. (1992). Assessment, prevalence, and cardiovascular benefits of physical activity and fitness in youth. Medicine and Science in Sports and Exercise, 24(suppl.), S237-S247. Baranowski, T., Dworkin, R.J., Cieslik, C.J., Hooks, P., Clearman, D.R., Ray, L., Dunn, J.K., & Nader. P.R. (1984). Reliability and validity of self-report of aerobic activity: Family health project. Research Quarterly for Exercise and Sport, 55, 309-317. Baranowski, T, Hooks, P., Tsong, Y., Cieslik, C., & Nader, P.R. (1987). Aerobic physical activity among third to sixth-grade children. Developmental and Behavioral Pediatrics, 8(4), 203-206. Baranowski, T., Thompson, W.O., DuRant, R., Baranowski, J., & Puhl, J. (1993). Observations on physical activity in physical locations: Age, gender, ethnicity, and month effects. Research Quarterly for Exercise and Sport, 64, 127-133. Bassett, D.R., Jr., Ainsworth, B.E., Swartz, A.M., Strath, S.J., O’Brein, K.O., & King, G.A. (in press). Validity of four motion sensors in measuring moderate intensity physical activity. Medicine and Science in Sports and Exercise. Bouten, C.V.C., Koekkoek, K.T.M., Verduin, M., Kodde, R., & Janssen, J.D. (1997). A triaxial accelerometer and portable data processing unit for the assessment of daily physical activity. IEEE Transactions on Biomedical Engineering 44(3), 136-147. Bouten, C.V.C., Verboeket-Van De Veene, W.P.H.G., Westerterp, K.R., Verduin, M., & Janssen, J.D. (1996). Daily physical activity assessment: Comparison between movement registration and doubly labeled water. Journal of Applied Physiology, 81, 1019-1026. Caspersen, C.J., Powell, K.E., & Christenson, G.M. (1985). Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research, Public Health Reports, 100, 126-131. Coleman, K.J., Saelens, B.E., Wiedrich-Smith, M.D., Finn, J.D., & Epstein, L.H. (1997). Relationships between TriTrac-R3D vectors, heart rate, and self-report in obese children. Medicine and Science in Sports and Exercise, 29, 1535-1542. Cooper Institute for Aerobics Research. (1999). The Fitnessgram test administration manual (6th ed.). Champaign, IL: Human Kinetics. Corbin, C.B., Pangrazi, R.P., & Welk, G.J. (1994). Toward an understanding of appropriate physical activity levels for youth. Physical Activity and Fitness Research Digest, 1(8), 1-8. Council for Physical Education for Children. (1998). Physical Activity for Children: A Statement of Guidelines. Reston, VA: NASPE Publications. Craig, S., Goldberg, J., & Dietz, W.H. (1996). Psychosocial correlates of physical activity among fifth and eighth graders. Preventive Medicine, 25, 506-5 13. Crocker, P.R.E., Bailey, D.A., Faulkner, R.A., Kowalski, K.C., & McGrath, R. (1997). Measuring general levels of physical activity: preliminary evidence for the Physical Activity Questionnaire for older children. Medicine and Science in Sports and Exercise, 29, 1344-1349. Dale, D. (1999). Using the GSA activity monitor to determine if children compensate for restricted periods of physical activity. Unpublished doctoral dissertation, Arizona State University, Tempe, AZ. DuRant, K., & Ainsworth, B.F., (1996). The recall of physical activity: using a cognitive model of the questionanswering process. Medicine and Science in Sports and Exercise, 28, 1282-1291. DuRant, R.H., Baranowski, T., Davis, H., Rhodes, T., Thompson, W.O., Greaves, K.A., & Puhl, J. (1993). Reliability and variability of indicators of heart-rate monitoring in children. Medicine and Science in Sports and Exercise, 25, 389-395. Epstein, L.H., Paluch, R.A., Coleman, K.J., Vito, D., & Anderson, K. (1996). Determinants of physical activity in obese children assessed by accelerometer and self-report. Medicine and Science in Sports and Exercise, 28, 11571164. Eston, R.G., Rowlands, A.V., & Ingledew, D.K. (1998). Validity of heart rate, pedometry, and accelerometry for predicting the energy cost of children’s activities. Journal of Applied Physiology, 84, 362-371. Garcia, A.W., George, T.R., Coviak, C., Antonakos, C.L., & Pender, N.J. (1997). Development of the Child/Adolescent Activity Log: A comprehensive and feasible measure of leisure-time physical activity. International Journal of Behavioral Medicine, 4, 324-329. Gilliam, T.B., Freedson, P.S., Geenen, D.L., & Shahraray, B. (1981). Physical activity patterns determined by heart rate monitoring in 6-7 year-old children. Medicine and Science in Sports and Exercise, 13, 65-67. Going, S.B., Levin, S., Harrell, J., Stewart, D., Kushi, L., Cornell, C.E., Hunsberger, S., Corbin, C., & Sallis, J. (1999). Physical activity assessment in American Indian schoolchildren in the Pathways study. American Journal of Clinical Nutrition, 69 (4 Suppl.), 788S-795S. Goran, M.I. (1995). Variation in total energy expenditure in humans. Obesity Research, 3, 59-66. Gortmaker, S.L., Cheung, L.W.Y., Peterson, K.E., Chomitz, G., Crade, J.H., Dart, H., Fox, M.K., Bullock, R.B., Sobol, A.M., Colditz, G.A., Field, A.E., & Laird, N. (1999). Impact of a school-based interdisciplinary intervention on diet and physical activity among urban primary school children: eat and keep moving. Archives of Pediatric and Adolescent Medicine, 153, 975-983. Gortmaker, S.L., Dietz, W.H., Sobol, A.H., & Wehler, C.A. (1987). Increasing pediatric obesity in the U.S. American Journal of Diseases in Children, 1, 535-540. Hager, R. (1999). The effect of television on children’s opportunities for physical activity. Unpublished doctoral dissertation, Arizona State University, Tempe, AZ. Haskell, W.L., Yee, M.C., Evans, A., & Irby, P.J. (1993). Simultaneous measurement of heart rate and body motion to quantitate physical activity. Medicine and Science in Sports and Exercise, 25, 109-115. Health Education Authority. (1998). Young and Active? Policy framework for young people and health-enhancing physical activity. London, England: HEA Publishing. Hendleman, D., Miller, K., Bagget, C., Debold, E., & Freedson P.S. (in press). Validity of accelerometry for the assessment of moderate intensity physical activity in the field. Medicine and Science in Sports and Exercise. Hill, J.O., Johnson, S.L., Melby, C., & Peters, J.C. (1995). Physical activity and energy requirements. American Journal of Clinical Nutrition, 62 (Suppl.), 1059S-1066S. Janz, K.F. (1994). Validation of the CSA accelerometer for assessing children’s physical activity. Medicine and Science in Sports and Exercise, 26, 369-375. Janz, K.F., Golden, J.C., Hansen, J.R., & Mahoney, L.T. (1992). Heart rate monitoring of physical activity in children and adolescents: the Muscatine study. Pediatrics, 89, 256-261. Katzmarzyk, P.T., & Malina, R.M. (1999). Contribution of organized sports participation to estimated daily energy expenditure in youth. Pediatric Exercise Science, 10, 378-386. Kilanowski, C., Consalvi, A., & Epstein, L.H. (1999). Validation of an electronic pedometer for measurement of physical activity in children. Pediatric Exercise Science, 11, 63-68. Livingstone, M.B. (1997). Heart-rate monitoring: the answer for assessing energy expenditure and physical activity in population studies? The British Journal of Nutrition, 78, 869-871. Livingstone, M.B.E., Coward, W.A., Prentice, A.M., Davies, P.S.W., Strain, J.J., McKenna, P.G., Mahoney, C.A., White, J.A., Stewart, C.M., & Kerr, M.J. (1992). Daily energy expenditure in free-living children: Comparison of heart-rate monitoring with the doubly labeled water (2H2180) method 1-3. American Journal of Clinical Nutrition, 56, 343-352. Luke, A., Maki, K.C., Barkey, N., Cooper, R., & McGee, D. (1997). Simultaneous monitoring of heart rate and motion to assess energy expenditure. Medicine and Science in Sports and Exercise, 29, 144-148. MacConnie, S.E., Gilliam, T.B.G.D.L., & Pels, A.E. (1982). Daily physical activity patterns determined by heart rate monitoring in 6-7 year-old children. International Journal of Sports Medicine, 3, 202-207. Mahoney, L.T., Lauer, R.M., Lee, J., & Clarke, W.R. (1991). Factors affecting tracking of coronary heart disease risk factors in children. The Muscatine Study. Annals of the New York Academy of Sciences, 623, 120-132. McKenzie, T.L. (1991). Observational measures of children’s physical activity. Journal of School Health, 61(5), 224-227. McMurray, R.G., Harrell, J.S., Bradley, C.B., Webb, J.P., & Goodman, E.M. (1998). Comparison of a computerized physical activity recall with a triaxial motion sensor in middle-school youth. Medicine and Science in Sports and Exercise, 30, 1238-1245. Melanson, E.L., Jr., & Freedson, P.S. (1996). Physical activity assessment: A review of methods. Critical Reviews in Food Science and Nutrition, 36, 385-396. Moon, J.K., & Butte, N.F. (1996). Combined heart rate and activity improve estimates of oxygen consumption and carbon dioxide production rates. Journal of Applied Physiology, 81, 1754-1761. Myers, L., Strikmiller, P.K., Webber, L.S., & Berenson, G.S. (1996). Physical and sedentary activity in school children grades 5-8: The Bogalusa Heart Study. Medicine and Science in Sports and Exercise, 28, 852-859. Pangrazi, R.P., Corbin, C.B., & Welk, G.J. (1996). Physical activity for children and youth. Journal of Physical Education, Recreation and Dance, 67(4), 38-43. Pate, R.R. (1993). Physical activity assessment in children and adolescents. Critical Reviews in Food Science and Nutrition, 33(4-5), 321-326. Pate, R.R., Baranowski, T., Dowda, M., & Trost, S.G. (1996). Tracking of physical activity in young children. Medicine and Science in Sports and Exercise, 28, 92-96. Pate, R.R., Long, B.J., & Heath, C. (1994). Descriptive epidemiology of physical activity in adolescents. Pediatric Exercise Science, 6, 434-447. Pate, R.R., Trost, S.C., Dowda, M., Ott, A.E., Ward, D.S., Saunders, R., & Felton, G. (1999). Tracking of physical activity, physical inactivity, and health-related physical fitness in rural youth. Pediatric Exercise Science, 11, 364376. Riddoch, C.J., & Boreham, C.A. (1995). The health-related physical activity of children. Sports Medicine, 19(2), 86102. Rippe, J.M., & Hess, S. (1998). The role of physical activity in the prevention and management of obesity. Journal of the American Dietetic Association, 98(10 suppl. 2), S31 Ross, J.G., & Gilbert, G.G. (1985). NCYFS: A summary of findings. Journal of Physical Education, Recreation and Dance, 56(1) 45-50. Rowland, T.W. (1985). Aerobic response to endurance training in prepubescent children: a critical analysis. Medicine and Science in Sports and Exercise, 17, 493-497. Rowland, T.W. (1998). The biological basis of physical activity. Medicine and Science in Sports and Exercise, 30, 392-399. Rowlands, A.V., Eston, R.G., & Ingledew, D.K. (1997). Measurement of physical activity in children with particular reference to the use of heart rate and pedometry. Sports Medicine, 24(4), 258-272. Rowlands, A.V., Eston, R.G., & Ingledew, D.K. (1999). Relationship between activity levels, aerobic fitness, and body fat in 8- to 10-yr-old children. Journal of Applied Physiology, 86, 1428-1435. Sady, S.P. (1986). Cardiorespiratory exercise training in children. Clinics in Sports Medicine, 5, 493-514.Sallis, J.F. (1991). Self-report measures of children’s physical activity. Journal of School Health, 61(5), 215-219. Sallis, J.F., Buono, M.J., Roby, J.J., Micale, F.G., & Nelson, J.A. (1993). Seven-day recall and other physical activity self-reports in children and adolescents. Medicine and Science in Sports and Exercise, 25, 99-108. Sallis, J.F., McKenzie T.L., Elder, J.P., Hoy, P.L., Galati, T., Berry, C.C., Zive, M.M., & Nader, P.R. (1998). Sex and ethnic differences in children’s physical activity: discrepancies between self-report and objective measures. Pediatric Exercise Science, 10, 277-284. Sallis, J.F., Nader, P.R., Broyles, S.L., Berry, C.C., Elder, J.P., McKenzie, T.L., & Nelson, J.A. (1993). Correlates of physical activity at home in Mexican-American and Anglo-American preschool children. Health Psychology, 12, 390-398. Sallis, J.F., & Patrick, K. (1994). Physical activity guidelines for adolescents: consensus statement. Pediatric Exercise Science, 6, 302-314. Sallis, J.F., Strikmiller, P.K., Harsha, D.W., Feldman, H.A., Ehlinger, S., Stone, E.J., Williston, J., & Woods, S. (1996). Validation of interviewer and self-administered physical activity checklists for fifth grade students. Medicine and Science in Sports and Exercise, 28, 840-851. Simons-Morton, B., Parcel, G.S., O’Hara, N.M., Blair, S.N., & Pate, R.R. (1988). Health-related physical fitness in childhood: Status and recommendations. Annual Review of Public Health, 9, 403-425. Simons-Morton, B.C., McKenzie, T.J., Stone, E., Mitchell, P., Osganian, V., Strikmiller, P.K., Ehlinger, S., Cribb, P., & Nader, P.R. (1997). Physical activity in a multiethnic population of third graders in four states. American Journal of Public Health, 87, 45-50. Simons-Morton, B.G., Taylor , W.C., & Huang, I.W. (1994). Validity of the physical activity interview and Caltrac with preadolescent children. Research Quarterly for Exercise and Sport, 65, 84-88. Sleap, M., & Warburton, P. (1992). Physical activity levels of 5-11 year-old children in England as determined by continuous observation. Research Quarterly for Exercise and Sport, 63, 238-245. Spady, D.W. (1980). Total daily energy expenditure of healthy, free ranging school children. American Journal of Clinical Nutrition, 33, 766-775. Stone, E.J., McKenzie T.L., Welk, G.J., & Booth, M.L. (1998). Effects of physical activity interventions in youth: Review and synthesis. American Journal of Preventive Medicine, 15, 298-315. Treiber, F.A., Musante, L., Hartdagan, S., Davis, H., Levy, M., & Strong, W.B. (1989). Validation of a heart rate monitor with children in laboratory and field settings. Medicine and Science in Sports and Exercise, 21, 338-342. Treuth, M.S., Adolph, A.L., & Butte, N.F. (1998). Energy expenditure in children predicted from heart rate and activity calibrated against respiration calorimetry. American Journal of Physiology, 275 (Endocrinology Metabolism), El2-E18. Troiano, R.P., & Flegal, K.M. (1998). Overweight children and adolescents: Description, epidemiology, and demographics. Pediatrics, 101, 497-504. Troiano, R.P., Flegal, K.M., Kuczmarski, R.J., Campell, S.M., & Johnson, C.L. (1995). Overweight prevalence and trends for children and adolescents. Archives of Pediatric and Adolescent Medicine, 149, 1085-1091. Trost, S.G., Pate, R.R., Dowda, M., Saunders, R., Ward, D.S., & Felton, G. (1996). Gender differences in physical activity and determinants of physical activity in rural fifth grade children. Journal of School Health, 66, 145-150. Trost, S.G., Ward, D.S., & Burke, J.R. (1998). Validity of the Computer Science and Application (CSA) Activity Monitor in children. Medicine and Science in Sports and Exercise, 30, 629-633. U.S. Department of Health and Human Services. Physical Activity and Health: A Report of the Surgeon General. (1996). U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, & National Center for Chronic Disease Prevention and Health Promotion. Atlanta, GA. Verschuur, R., & Kemper, H.C. (1982). Habitual physical activity in Dutch teenagers measured by heart rate. In R.A. Binkhorst, H.C. G. Kemper, & W.H.M. Sails (Eds.), Children & Exercise XI (pp. 3-25). Champaign, IL: Human Kinetics. Wareham, N.J., & Rennie, K.L. (1998). The assessment of physical activity in individuals and populations: Why try to be more precise about how physical activity is assessed? International Journal of Obesity and Related Metabolic Disorders, 22, S30-S38 Welk, G.J., Blair, S.N., Wood, K., Jones, S., & Thompson, K.W. (in press). The validity of physical activity monitors for the assessment of lifestyle physical activity. Medicine and Science in Sports and Exercise. Welk, G.J., & Corbin, C.B. (1995). The validity of the Tritrac-R3D activity monitor for the assessment of physical activity in children. Research Quarterly for Exercise and Sport, 66, 202-209. Welk, G.J., Corbin, C.B., & Kampert, G.B. (1998). The validity of the Tritrac-R3D activity monitor for the assessment of physical activity: II. Temporal relationships among objective assessments. Research Quarterly for Exercise and Sport, 69, 395-399. Welk, G.J., Differding, J.A., Thompson, R.W., Blair, S.N., Dziura, J., & Hart, P. (in press). The utility of the DigiWalker step counter to assess daily physical activity patterns. Medicine and Science in Sports and Exercise. Welk, G.J., & Wood, K. (2000). Physical activity assessments in physical education: A practical review of instruments and their use in the curriculum. Journal of Physical Education, Recreation and Dance, 71(1), 30-40. Westerterp, K.R., & Goran, M.I. (1997). Relationship between physical activity related energy expenditure and body composition: a gender difference. International Journal of Obesity, 21, 184-188. Weston, A.T., Petosa, R., & Pate, R.R. (1997). Validation of an instrument for measurement of physical activity in youth. Medicine and Science in Sports and Exercise, 29, 138-143. Whitaker, R.G., Wright, J.A., Pepe, M.S., Seidel, K.D., & Dietz, W.H. (1997). Predicting Obesity in Young Adulthood from Childhood and Parental Obesity. The New England Journal of Medicine, 337, 869-873.