Epithelium Histo Review
advertisement

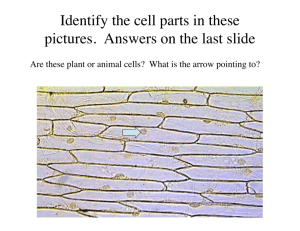
Thursday, July 28, 2011 8:07 PM 1. Discuss the characteristics of epithelium that make it a unique tissue. 1. Closely opposed; close proximity and adhere to each other by cell junctions, cell to cell adhesion molecules 2. Exhibit polarity; they have an apical, lateral, and basal domain 3. Their basal surface is attached to a non-cellular basement membrane 2. Describe the composition and functions of the basement membrane. Composed of Collagen (mostly type IV), Laminin (initiates basal lamina assembly and has binding sites for integrin), and Proteoglycans (cross-links Collagen to Laminin and is mostly made up of Perlecan). Fibronectin is an additional protein cross-linking collagen to laminin. Function of basement membrane is to anchor epithelium to underlying connective tissue. 3. Describe the structural features and functions of intercellular junctions. (Lateral Junctional Complexes) - Connect via Cell Adhesion Molecules (CAM) 1) Occluding Junctions I. Zonula Occludin (tight junction) - Occludins and claudins seals adjacent cells together near apical zone. Function is: i. Barrier - limits movement of water and other molecules between cells; maintains physiochemical separation of tissue compartments ii. Recruits signal molecules iii. Paracellular transport - Claudins transport H2O, ions, and small molecules 2) Anchoring Junctions I. Zonula Adherens - reinforcement of junction below tight junction. Cadherin connects adjacent cell membranes; is anchored to intracellular actin filaments. Protein interaction from adjacent cells is mediated by Calcium. II. Macula Adherens (desmosome) - localized to lateral domain, very strong linkage, and provides anchoring sites for intermediate filaments via dense, desmosomal attachment plaque on cytosomal (cytoplasmic) side. On extracellular side are Cadherins that interact like a zipper and require Calcium for binding. III. Cell to Extracellular Matrix Junctions - (Cell to Extracellular Matrix Junctions) i. Focal Adhesions - anchor actin filaments of cytoskeleton to basement membrane. Interact with basement membrane via integrin molecules. Coordinate remodeling of actin cytoskeleton. And alter adhesion-mediated functions in response to external mechanical stimuli (demonstrate mechanosensitivity). ii. Hemidesmosomes - anchor intermediate filaments of cytoskeleton to basement membrane. Attachment plaque on cytoplasmic side similar to desmosome, but integrin molecules form transmembrane proteins distinct from desmosomes. Provides strong connection preventing separation from underlying connective tissue. 3) Communicating Junctions I. Gap Junctions - permits direct passage of signaling molecules between cells for coordinated activity via transmembrane channels consisting of 2 half channels (connexons); 6 connexins make up one connexon; 2 connexons form a gap junction. Connexon conformational changes (opening and closing) are mediated by Calcium, or other mechanisms. 4. Describe the microscopic criteria used to classify covering epithelium. 1) By layer I. Simple- One layer of cells II. Stratified - One or more layers of cells i. Keratinized -(for stratified squamous) Most apical layer of cells are dead and lose their nucleus and cytoplasm. However, they contain a tough, resistant protein called Keratin, which makes the epithelium waterproof. ii. Transitional - Term applied to the epithelium lining the lower urinary tract. Is stratified epithelium with specific morphologic characteristics that allow it to distend. 2) By cell shape I. Squamous - width of the cell is greater than its height, can appear tear-drop shaped II. Cuboidal - square-shaped III. Columnar - Tall, thin rectangular (can be ciliated) i. Pseudostratified Columnar -simple columnar epithelial cells whose nuclei appear at different heights giving the misleading impression that the epithelium is stratified when viewing a cross-section. 6. Describe the structure and function of microvilli, cilia and stereocilia. (Apical Domain Specializations) 1) Microvilli - Cytoplasmic projections from the apical surface (of epithilia) that vary in number, length, and density. Are filled with actin filaments that bind to a web of actin filaments below the base of the microvilli, called a terminal web. Microvilli can contract, decreasing the diameter of villus and increasing intervillous space. The presence of myosin II and tropomyosin in the terminal web allows the microvilli to contract. 2) Stereocilia - look like thin, irregularly distributed microvilli. Because of their length they were initially mistaken for cilia. They are non-motile and are found only in the epididymis, ductus deferens, and sensory (hair) cells of the inner ear (where they function as mechanoreceptors in hearing). 3) Cilia- are present on nearly every cell of the body and most are designed for motility (but not all). Epithelia that need to move substances across their surface, like mucous in the air passages, have cilia inserted in the cytoplasm by basal bodies. Consist of an internal core of microtubules arranged in a 9+2 pattern; axoneme (9 doublets of circularly arranged microtubules with 2 central microtubules). Cilia beat in synchronous movement coordinated by orientation of basal foot. I. Primary Cilia -are non-motile, arranged in a 9+0 pattern, and passively bend to flow of fluid. They also transduce various signals from environment into internal chemical signals that modify the cell's response to stimuli. 7. Describe the functions of the various epithelial cells and examples of where they are found 1) Secretion - columnar epithelium of the stomach and gastric glands 2) Absorption - in the columnar epithelium of the intestines and proximal convoluted tubules of the kidney 3) Transportation - transport of materials or cells along the surface of an epithelium by motile cilia or in the transport of materials across an epithelium to and from connective tissue 4) Protection - stratified squamous epithelium of the skin (epidermis) and the transitional epithelium of the urinary bladder 5) Receptor Function - receive and transduce external stimuli; e.g. taste buds of the tongue, olfactory epithelium of the nasal mucosa, and the retina of the eye 8. Characterize endocrine vs exocrine glands. 1) Endocrine gland - Lacks a duct system and secretes hormones into connective tissue which travels via bloodstream to reach target tissue, however paracrine secretions only affect neighboring cells. 2) Exocrine gland - Secretes products onto a surface directly or through epithelial ducts connected to surface. 9. Compare the three modes of exocrine gland secretion. 1) Merocrine - no loss of cytoplasm; most common mode (MN: mero/zero). Found in the 2) Holocrine - entire cell lost (MN: holo/whole) 3) Apocrine - apical cytoplasm lost (MN: apo/apical side/half) 10. Describe/identify the various structures of exocrine glands See Slide 61 for Chart 11. Describe clinical correlates of epithelial tissue discussed in lecture or otherwise indicated