50 Questions in Psychiatry
advertisement

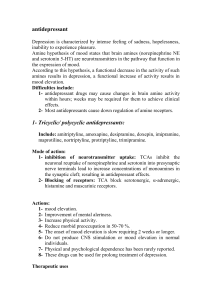
Pre-registration training 50 Questions in Psychiatry Mental health Act 1. Why do we need this act? 2. Briefly outline what we are allowed to do under section 2 of the mental health act. 3. To apply Section 3 what needs to be done? Why should this section be applied to a patient and what happens if they cannot consent? Psychosis and schizophrenia 4. Describe the theories of the aetiology of schizophrenia? 5. Describe the positive and negative symptoms of schizophrenia? 6. What are the aims of drug treatment in schizophrenia? 7. What are the two main groups of antipsychotics and what are their main differences? 8. List the five forms of extra-pyramidal side-effects. 9. In a patient with extrapyramidal side effects–which antipsychotic (s) would be a good choice? 10. What is tardive dyskinesia? a. List the risk factors. b. How can drug therapy be manipulated to improve the condition? 11. What is akathisia? What are the advantages and disadvantages of the various treatment options? 12. What is the current thinking on using long-term antimuscarinic treatment? 13. Why may clients on antipsychotic medication become non-compliant with their medication? a. What options are available to them in order to improve compliance? 14. What do the NICE guidelines for the use of atypical antipsychotics recommend for the treatment of schizophrenia? 15. When should clozapine be initiated and what precautions must be taken when prescribing? 16. Answer true or false. Clozapine a. Has affinity for both D1 and D2 receptors b. Causes agranulocytosis in 1-2% of patients treated c. Rarely causes drowsiness 1 17. List three reported adverse events due to clozapine? Affective disorders 18. What is meant by affective disorder? 19. What is bipolar disorder? 20. What are the treatment options in a client experiencing an acute manic phase? 21. What are the drug options for preventing relapse in a patient with bipolar disorder? 22. What tests need to be carried out before initiating lithium and how often should these tests be repeated? 20. Describe the interaction between lithium and a. NSAID b. Diuretic c. What recommendations would you make to the prescriber in each case? 23. What counselling would you give to a patient on lithium? 24. How should a patient who is on lithium admitted for elective surgery be managed? 25. A patient on valproate develops acute abdominal pain. What potentially serious adverse event would you consider? What blood test should be conducted? 26. When should ECT be used? 27. What are the main symptoms of depression? 28. How is drug therapy targeted at treating depression? 29. How could you assess and quantify the severity of depression? 30. What are the NICE recommendations on treating a first episode of mild depression? What is the first line drug treatment? 27. Which antidepressant(s) and why would you use in c. The elderly d. An epileptic e. liver disease f. an agitated patient g. someone so depressed that they are neither eating nor drinking. 31. Describe the symptoms of antidepressant discontinuation syndrome and how should it be managed? 2 32. Ward staff report a patient as having tremor, blurred vision and confusion. The patient has been taking 300mg phenytoin for some time and started Fluoxetine 20mg OM 12/7 ago. What is happening to this patient and what would you recommend? 33. Why would you advise using reboxetine in the elderly? 34. Answer true or false. Amitriptyline a. Is associated with sudden death in patients with pre-existing cardiac arrhythmias b. Is metabolised to two active metabolites nortriptyline and protriptyline c. Is extensively bound to plasma protein d. Can be given once daily because of a half life of over 36 hours 35. Which of the following are the agreed delay times before re-prescribing with respect to transfer from one drug to another? a. Fluoxetine to MAOIs 5 weeks b. TCAs to MAOIs 2 weeks c. MAOIs to TCAs 2 weeks d. Paroxetine to Venlafaxine 1 week e. Sertraline to mirtazepine cross taper cautiously Sleep 36. Describe the sleep cycle? 37. What non-pharmacological methods need to utilised first before using drug treatment to help sleep? 38. Briefly describe how the Z-drugs work. 39. What are the advantages of Z-drugs over the benzodiazepines? 40. What are the NICE recommendations on the Z-drugs? Anxiety 41. Describe the psychological and autonomic symptoms a person with GAD may describe? 42. What is the role of beta-blockers in anxiety? 43. What is the role of benzodiazepines? 44. List the advantages/disadvantages of SSRIs. Prescribing in the elderly 45. A patient is admitted to an elderly assessment ward suffering from confusion and short-term memory loss. What are the possible diagnoses? 3 46. What drug treatment can be used for a patient suffering from an organic disorder (dementia)? 47. NICE have issued guidelines on the treatment of Alzheimers disease. a. What should the MMSE score be before initiation of drug treatment? b. What assessments and how often should these be carried out once drug treatment is initiated? 48. List the adverse events of acetyl cholinesterase inhibitors such as donepezil? 49. How does schizophrenia present in the elderly and what treatments are used? 50. What precautions should be taken when prescribing for the elderly? 4