Antidepressant 2 ... 3. Atypical antidepressants:
advertisement
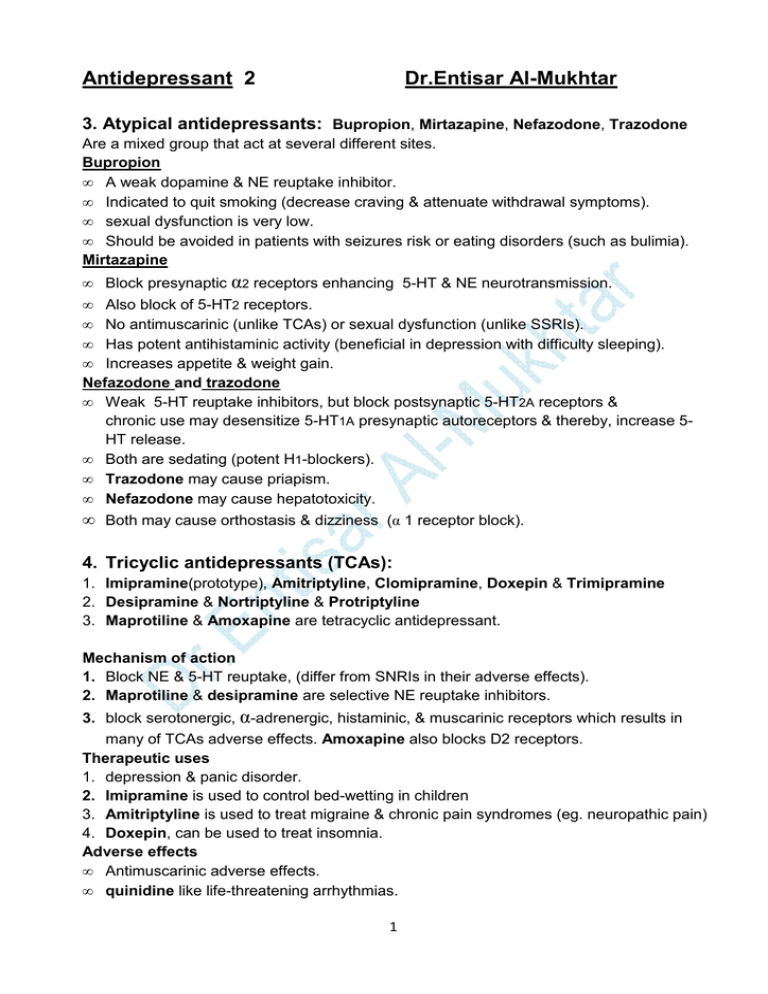
Antidepressant 2 Dr.Entisar Al-Mukhtar 3. Atypical antidepressants: Bupropion, Mirtazapine, Nefazodone, Trazodone Are a mixed group that act at several different sites. Bupropion • A weak dopamine & NE reuptake inhibitor. • Indicated to quit smoking (decrease craving & attenuate withdrawal symptoms). • sexual dysfunction is very low. • Should be avoided in patients with seizures risk or eating disorders (such as bulimia). Mirtazapine • Block presynaptic α2 receptors enhancing 5-HT & NE neurotransmission. • Also block of 5-HT2 receptors. • No antimuscarinic (unlike TCAs) or sexual dysfunction (unlike SSRIs). • Has potent antihistaminic activity (beneficial in depression with difficulty sleeping). • Increases appetite & weight gain. Nefazodone and trazodone • Weak 5-HT reuptake inhibitors, but block postsynaptic 5-HT2A receptors & chronic use may desensitize 5-HT1A presynaptic autoreceptors & thereby, increase 5HT release. • Both are sedating (potent H1-blockers). • Trazodone may cause priapism. • Nefazodone may cause hepatotoxicity. • Both may cause orthostasis & dizziness (α 1 receptor block). 4. Tricyclic antidepressants (TCAs): 1. Imipramine(prototype), Amitriptyline, Clomipramine, Doxepin & Trimipramine 2. Desipramine & Nortriptyline & Protriptyline 3. Maprotiline & Amoxapine are tetracyclic antidepressant. Mechanism of action 1. Block NE & 5-HT reuptake, (differ from SNRIs in their adverse effects). 2. Maprotiline & desipramine are selective NE reuptake inhibitors. 3. block serotonergic, α-adrenergic, histaminic, & muscarinic receptors which results in many of TCAs adverse effects. Amoxapine also blocks D2 receptors. Therapeutic uses 1. depression & panic disorder. 2. Imipramine is used to control bed-wetting in children 3. Amitriptyline is used to treat migraine & chronic pain syndromes (eg. neuropathic pain) 4. Doxepin, can be used to treat insomnia. Adverse effects • Antimuscarinic adverse effects. • quinidine like life-threatening arrhythmias. 1 • • • • • Orthostatic hypotension (most likely with imipramine & least likely with nortriptyline). Sedation Weight gain. Sexual dysfunction ( but lower than that associated with SSRIs). physical & psychological dependence are rare (withdrawal should be slowly). Drug interactions: 1. TCAs & MAOIs concomitant use result in HT, hyperpyrexia, convulsion & coma. 2. TCAs potentiate effects of direct-acting adrenergic drugs. 3. TCAs prevent indirect-acting sympathomimetic from reaching their sites of action. 4. TCAs used with ethanol or other CNS depressants may result in toxic sedation. Precautions : • TCAs (like all antidepressants) should be used with caution in patients with manicdepressive disorder (bipolar), since switch to manic behavior may occur . • TCAs have a narrow therapeutic index • Suicidal depressed patients should be given only limited quantities of TCAs with close monitoring. • TCAs may exacerbate unstable angina, BPH, epilepsy and preexisting arrhythmias. 5. Monoamine oxidase inhibitors (MAOIs) • • • MAO enzyme founds in nerve, gut & liver. MAOIs may irreversibly or reversibly inactivate the enzyme & this is may be responsible for the indirect antidepressant action of MAOIs. available MAOIs: Phenelzine, Tranylcypromine, Isocarboxazid & Selegiline (also used treat Parkinson’s disease) Mechanism of action • MAOIs, such as phenelzine, irreversibly inactivate MAO in the brain, increasing neuronal stores of NE, 5-HT & dopamine. • Liver & gut MAO enzymes ( which catalyze metabolism of drugs & potentially toxic substances such as tyramine founds in certain foods) are also inhibited, therefore MAOIs show a high incidence of drug-drug & drug-food interactions. • Selegiline transdermal patch may produce less inhibition of gut & hepatic MAO because it avoids first-pass metabolism. Actions • MAO is fully inhibited after several days of treatment, but antidepressant action is delayed several weeks. • Selegiline & tranylcypromine have an amphetamine- like stimulant effect that may produce agitation or insomnia. Therapeutic uses • Depressed patients unresponsive or allergic to TCAs & SSRIs or who experience strong anxiety. • Beneficial in patients with low psychomotor activity (due to stimulant properties). 2 • • Phobic states. Atypical depression (ccc by labile mood, rejection sensitivity & appetite disorders). Pharmacokinetics • Irreversibly inactivated MAO requires several weeks for regeneration Adverse effects MAOIs interfere with degradation of tyramine in the diet, resulting in hypertensive crisis. So, tyramine-containing foods should be avoided ( MAOIs are last-line agents due to drug-food & drug-drug interactions). • Phentolamine & prazosin are helpful for management of tyramine-induced HT. Note: MAOIs may be dangerous in severely depressed patients with suicidal tendencies. • Other possible side effects include drowsiness, orthostatic hypotension, blurred vision, dry mouth, dysuria & constipation. • MAOIs & SSRIs should not be coadministered due to the risk of the life-threatening serotonin syndrome & at least 2 weeks washout periods is required before the other type is administered, with the exception of fluoxetine, which should be discontinued at least 6 weeks before a MAOI is initiated. • Combination of MAOIs and bupropion can produce seizures. Treatment of mania and bipolar disorder A. Lithium • Lithium salts are used prophylactically to treat manic-depressive patients & manic episodes & thus, are considered as “mood stabilizers.” Note: Lithium interferes with the resynthesis (recycling) of phosphatidylinositol bisphosphate (PIP2), depleting it in the CNS. • Lithium is given orally & excreted by the kidney. • Lithium salts can be toxic (therapeutic index is comparable to that of digoxin). • Common adverse effects may include, dry mouth, polydipsia, polyuria, polyphagia, GI distress, tremor, dizziness, fatigue, dermatologic reactions & sedation. Note: Amiloride can be used to treat diabetes insipidus induced by lithium. • Lithium higher dose may cause ataxia, slurred speech, coarse tremors, confusion & convulsions. • Thyroid function may be decreased • Used cautiously in renally impaired patients, whereas it may be the best choice in patients with hepatic impairment. B. Other drugs The following drugs have been approved as mood stabilizers for bipolar disorder: 1. Carbamazepine, valproic acid & lamotrigine. 2. Older antipsychotics (eg. chlorpromazine & haloperidol) & the newer (atypical) antipsychotics (risperidone, olanzapine, ziprasidone, aripiprazole, asenapine, quetiapine & lurasidone) & the combination of olanzapine and fluoxetine. . 3