韩鸿玲-glomerulonephritis
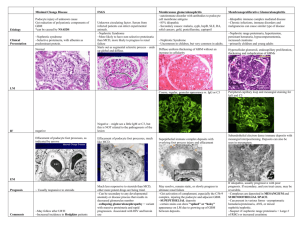
advertisement
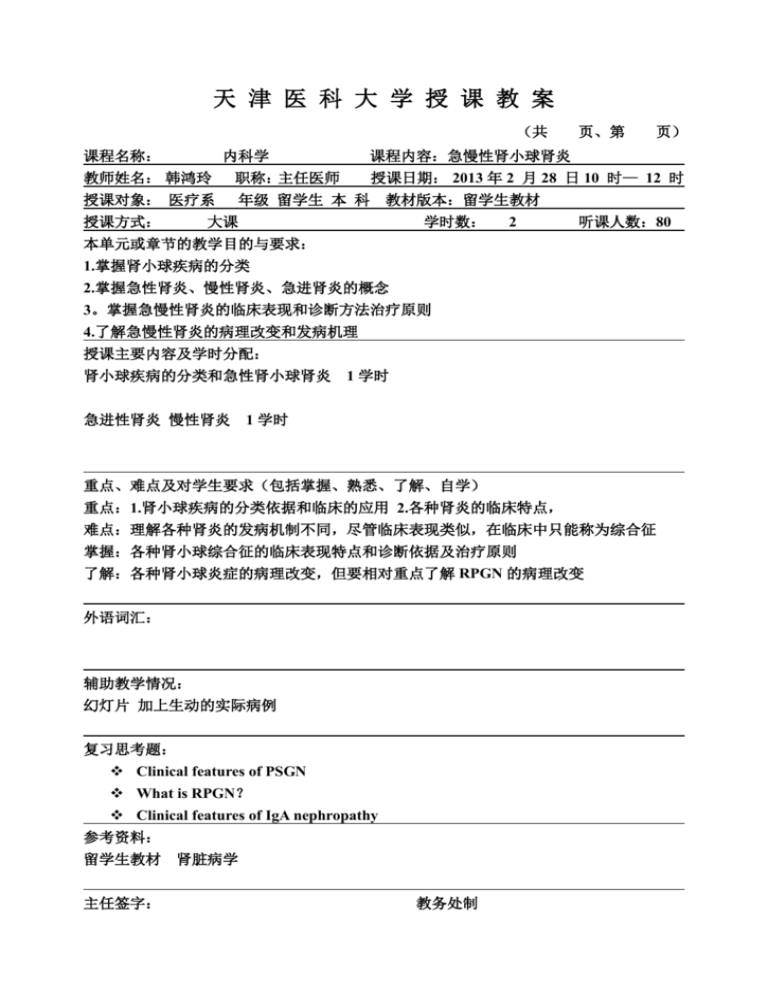
天 津 医 科 大 学 授 课 教 案 (共 课程名称: 内科学 页) 课程内容:急慢性肾小球肾炎 教师姓名: 韩鸿玲 职称:主任医师 授课对象: 医疗系 年级 留学生 本 科 授课方式: 页、第 授课日期: 2013 年 2 月 28 日 10 时— 12 时 教材版本:留学生教材 大课 学时数: 2 听课人数:80 本单元或章节的教学目的与要求: 1.掌握肾小球疾病的分类 2.掌握急性肾炎、慢性肾炎、急进肾炎的概念 3。掌握急慢性肾炎的临床表现和诊断方法治疗原则 4.了解急慢性肾炎的病理改变和发病机理 授课主要内容及学时分配: 肾小球疾病的分类和急性肾小球肾炎 1 学时 急进性肾炎 慢性肾炎 1 学时 重点、难点及对学生要求(包括掌握、熟悉、了解、自学) 重点:1.肾小球疾病的分类依据和临床的应用 2.各种肾炎的临床特点, 难点:理解各种肾炎的发病机制不同,尽管临床表现类似,在临床中只能称为综合征 掌握:各种肾小球综合征的临床表现特点和诊断依据及治疗原则 了解:各种肾小球炎症的病理改变,但要相对重点了解 RPGN 的病理改变 外语词汇: 辅助教学情况: 幻灯片 加上生动的实际病例 复习思考题: Clinical features of PSGN What is RPGN? Clinical features of IgA nephropathy 参考资料: 留学生教材 肾脏病学 主任签字: 教务处制 天 津 医 科 大 学 授 课 教 案 (共 5 页、第 1 页) AGN Gross or microscopic hematuria is most common, and is often described by the patients as smoky- coffee- or cola-colored urine. The erythrocytes in the urinary sediment are small, distored, fragmented and hypochromic which is called dysmorphic hematuria. In general, gross hematuria may last a few days to 1 or 2 weeks and then disappear. B. Proteinuria The degree of proteinuria varies according to the nature and severity of the underlying glomerular lesion. Rarely, protein excretion rates are within the normal range, but generally they are between 0.2 and 3g/d and nonselective. If proteinuria is marked and sustained, the NS may appear. C. Edema The edema appears in areas of low tissue pressure, such as periorbital areas, especially in the morning. This is called nephritic faces. Severe edema may progress to dependent portion of the body and lead to ascites and/or pleural effusions. D.Hypertension Almost 80% of cases have a mild to moderate degree of hypertension, especially in old patients. E. Oliguria Oliguria may be present when nephritis occurs. Usually less than 500ml/d, which leads to azotemia. Two weeks later the amount of urine may gradually increase. F. Renal function lesion Glomerular inflammation can lead to reduced glomerular filtration that could lead to azotemia. Usually after a diuretic, azotemia may gradually disappear, if not, acute renal failure occurs. G. Others Other symptoms of PSGN may be vomiting, nausea, sleeping, loin pain etc. Complications The complications of PSGN are heart failure, encephalopathy and uremia. Laboratory findings RBCs and RBC casts, leukocyte casts, WBCs, FDP, Cз, non-selective proteinuria (non-nephrotic range) can be detected in urine. In most children and adults, proteinuria will become negative after 4 to 6 months of onset of nephritis. Other laboratory features include positive tests for circulating immune complexes, an elevated antistreptolysis O titer, a low serum complement (usually returning to normal at 6 to 12 weeks), azotemia, elevated erythrocyte sedimentation rate (ESR) and mild anemia. Diagnosis and differential diagnosis The diagnosis of PSGN can be based on the typical renal presentation following streptococcal infection, hypocomplementemia, and serologic evidence. The differential diagnosis is that of AGN with hypocomplementemia and includes other forms of postinfectious GN, e. g. bacterial endocarditis, shunt nephritis, systemic lupus erythematosus (SLE), and membranoproliferative GN. Because the diagnosis is most often straightforward, a renal biopsy is indicated only of the disease follows an atypical course in children. Most adults with acute nephritic syndrome require a kidney biopsy to establish the diagnosis. Course and treatment Complete recovery occurs in at least 85 to 90% of all patients. However, minor urinary sediment abnormalities may continue for several years in some patients (<2%), but progression to chronic renal failure is rare, typically occurring only in older adults. Fewer than 5% of patients have oliguria for more than 7 to 9 days, and the prognosis in these patients is less favorable. There is no specific therapy for PSGN. The treatment is supportive and symptomatic until all acute signs have abated. It’s reasonable to recommended bed rest until the signs of glomerular inflammation subside. Mild protein restriction is desirable for azotemic patients. Seven to 10 days of penicillin or other suitable antimicrobials should be given with evidence of streptococcal infection. Salt restriction and, in some cases, diuretics and antihypertensive agents may be required to manage sodium retention (manifested by hypertension, edema, congestive heart failure, and other signs). Steroids and cytotoxic drugs are not of value. Rapidly progressive glomerulonephritis (RPGN) RPGN is characterized clinically by the rapid deterioration of renal function that reaches end stage within a period of days or weeks, and histologically by extensive crescents. It can be an idiopathic primary glomerular disease or can be superimposed on other glomerular diseases, either primary or secondary. Classification and pathology The classification of RPGN is based on immunofluorescence microscopic findings. The categories are as follows (shown in table -2): Table -2 Types of RPGN Types Light microscopy Immunofluorenscence Microscopy Possible Pathogenesis Association Anti-GBM antibody Crescents Necrosis Linear-IgG Fibrinogen Anti-GBM Pulmonary hemorrhage Immune-complex es Crescents Proliferation Non-immu ne-complex es Crescent s Necrosis Granular IgG complement fibrinogen Immunecomplexes Negative ANC A Bacterial infections Systemic symptom s rash,feve r ·Glom erulon ephriti s due to antibo dies directe d toward glomer ular basem ent membr ane antige ns (anti-GBM). It accounts for 20% of all cases of RPGN. ·Glomerulonephritis due to the deposition or formation of immune complexes in the glomeruli. It accounts for 40% of all cases of RPGN. ·Glomerulonephritis in which no immunoglobulins are found in the glomeruli (so-called nonimmune). It accounts for 40% of cases of RPGN. By light microscopy, extracapillary proliferation (i.e. crescents) can be detected which is a feature of RPGN. Usually more than 70% of glomeruli are involved with crescents (so called crescentic glomerulonephritis Figure-4). Endocapillary proliferation, if prominent, suggests the presence of infection. Segmental or diffuse endocapillary necrosis suggests underlying systemic necrotizing vasculitis. Nonstreptococcal acute postinfectious glomerulonephritis Nonstreptococcal acute postinfectious glomerulonephritis includes a wide variety bacterial states and various viral and parasitic diseases e.g. infective endocarditis, sepsis of other types, visceral abscess, typhoid fever, infectious mononucleosis, acute viral hepatitis B, falciparum malaria, and toxoplasmosis etc. Circulating immune complexes play an important role in the pathogenesis of AGN in these diseases. The clinical and histologic manifestation may vary somewhat, still, most have features similar to the PSGN. If the underlying infection is eradicated, the prognosis is good. Systemic lupus erythematous, Henoch-Schönlein purpura, and mixed essential cryoglobulinemia may present as an acute GN, but they are usually associated with other glomerular syndromes. Asymptomatic urinary abnormalities This group of patients has proteinuria in the nonnephrotic range and /or hematuria, unaccompanied by edema, reduced GFR, and hypertension. Abnormalities are often discovered incidentally and may be persistent or recurrent. In some, this syndrome is a phase in the natural history of other glomerulopathic syndromes, especially NS or chronic glomerulonephritis. Asymptomatic hematuria A variety of renal lesion may present as asymptomatic hematuria. IgA nephropathy IgA nephropathy or Berger’s disease is the most common cause of recurrent hematuria of glomerular origin. It accounts for 50% of cases with asymptomatic hematuria and 26 to 34% in primary glomerulopathy. Light microscopic changes are variable, but diffuse mesangial proliferative glomerulonephritis or focal and segmental proliferative glomerulonephritis is found most often. In some cases, glomerular morphology may be normal; uncommonly, crescents may be found. The diagnosis depends on the finding of prominent IgA deposits in the mesangium by immunofluorescence microscopy. The typical presentation is gross hematuria following a viral illness or vigorous exercise, with men affected two to three times more frequently than women. Most other patients present with asymptomatic hematuria discovered on an incidental examination, accompanied by mild to moderate proteinuria. Most patients are between the ages of 15 and 35. Microscopic hematuria usually remains after gross hematuria resolves. Mild proteinuria of less than 1g/d is common, but the NS develops occasionally. Serum complement is normal. Serum IgA levels are increased in about 50% of cases. At present, there is no evidence that therapy will influence the natural history, although intermittent steroid therapy may reduce the frequency of episodes of gross of hematuria. Steroids may also result in remissions of proteinuria in those patients with NS. The prognosis is variable, but the disease tends to progress slowly. Approximately 50% of patients develop end stage renal failure within 25 years of the time if diagnosis. Poor prognostic indicators include nephrotic range proteinuria, hypertension, and azotemia. IgA nephropathy recurs in the transplanted kidney in approximately 30 to 40% of cases, but with minimal long-term effects on renal function. Chronic glomerulonephritis(CGN) The syndrome of chronic glomerulonephritis is characterized by persistent urinary abnormalities (proteinuria and/or hematuria), by hypertension and the progressive loss of functioning nephrons. Except for the minimal change, all the disorders described in this chapter can lead to chronic glomerulonephritis. At the earliest time points, only mild proteinuria with a slight decrease in GFR and minimal hypertension may be seen. Inevitably, these patients generally progress to ESRD. Treatment is supportive and symptomatic. Hypertension and infections should be treated vigorously. Nephrotoxic agents should be avoided. Anticoagulants and ACEI may be beneficial. The prognosis of CGN depends upon the nature of the underlying disease and presence or absence of complications, especially hypertension. Ten, twenty, or more years may elapse from the first discovery of CGN until the development of ESRD. Renal biopsy is necessary to define the precise nature of the glomerular lesion. 教务处制