Glomerulonephritis_2007_revised
advertisement

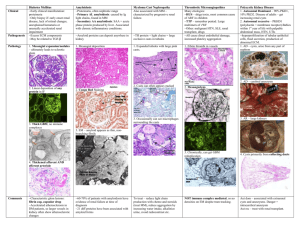
Glomerular Disease Farid M. Nakhoul M.D. Department Of Nephrology Rambam-Health Care Campus Email: f_nakhoul@rambam.health.gov.il Classification Based on Clinical Presentation – History – Physical Exam (Edema? Hypertension?) – Urinalysis (Nephritic? Nephrotic?) – Presence of Renal Failure – Time Course Presentation varies from patient to patient, e.g., IgA Nephropathy Clinical Features of Glomerular Diseases Proteinuria Hematuria Edema Hypertension Renal Dysfunction Glomerulonephritis Kidney diseases that primarily affect the glomerulus. Leading Cause of End Stage Renal Disease worldwide Third leading cause of End Stage Renal Disease in the United States Introduction-I • Glomerular disease has clinical presentations that vary from the asymptomatic individual who is found to have hematuria, proteinuria, to a patient with a fulminant illness with acute renal failure possibly associated with life-threatening extrarenal disease. Introduction -II • Numerous Inflammatory and Noninflammatory diseases affect the glomerulus and lead to alterations in glomerular permeability, structure, and function. • GN may be primary , restricted in clinical manifestations to the kidney, or it may be part of multisystem Dis. , most frequently SLE or vasculitis. Introduction-III • The presence of some form glomerular disease is usually suspected from the history and from one or more of the following urinary findings: hematuria particulary dismorphic red blood cells, red cell casts, proteinuria, associated with renal insufficiency (Pcr is high), oliguria and arterial hypertension>>>> (Nephritic Syndrome). GN-Clinical Evaluation • History>>Family, Hearing loss • Physical Examination>> Edema, Purpura • Laboratory studies>> Urine sediment • Imaging/US>>To ensure the presence of two kidneys, to rule out obstruction. • Renal Biopsy>> require to establish the type of glomerular disease and to guide treatment decision. Nephritic Syndrome • • • • • Decreased urinary output Dark or smoky urine (hematuria) Volume-dependent HTN Edema,CHF, seizures Urinalysis: dysmorphic RBCs, RBC, WBC, proteinuria (non-nephrotic) • C3,C4 are low. • KNB • ARF requiring dialysis Laboratory 1. 2. 3. 4. 5. 6. 7. Urine Sediment/volume C3, C4 Anti-DNA/ ANA CBC/ Kidney Function Tests ANCA (P,C), Cryoglobulins, Anti-GBM. HbsAg, Anti-HCV abs, Liver Function Tests Classificatio of urinary Casts • Hyaline: non indicative of renal disease • Red cell cast: GN, Vasculitis • • • • Granular: degenerating cellular cast Waxy: Advanced Renal Failure Fatty: Nephrotic syndrome Epithelial Cell: ATN RBC Cast Imaging • Kidney Ultrasound • Kidney Biopsy: Closed/ Laparoscopic Pathogenesis 1.In-situ Immune reaction: - Anti-GBM nephritis 2. Circulating Immune-Complexes - Endogenous (DNA) or - Exogenous(Streptococci, Hepatitis B, C). Classification • GN is classified by the different patterns of histologic injury seen on a renal biopsy examined by light microscopy, immunofluorescence, and electron microscopy. • It is more helpful to regard the renal biopsy appearance as a ‘Pattern’ rather than a disease. Acute Glomerulonephritis (KNB) • Focal Glomerulonephritis • Diffuse Glomerulonephritis Focal Glomerulonephritis • Focal glomerulonephritis is associated with inflammatory lesions in less than one-half glomeruli on light microscopy • The urinalysis reveals red cells ( dysmorphic) occasionally red cell casts and mild proteinuria(<1.5gr). • Renal insufficiency and hypertension are usually absent. • These patients often present with asymptomatic hematuria and proteinuria. 1. Focal Glomerulonephritis • Mild post-infectious GN • IgA Nephropathy • Henoch-Schonlein purpura IgA Nephropathy and HSP • IgA nephropathy is a mesangial proliferative glomerulonephritis, characterized by diffuse deposition of IgA . • Clinical presentation is visible Hematuria provoked by mucosal infection. • Henoch-Schonlein purpura is a small –vessels vasculitis affecting the the kidney, skin and gut. Is characterized by mesangial IgA deposition. IgA Nephropathy • In 50% of cases the clinical presentation is episodic macroscopic hematuria, most frequently in the second and third decades of life. • Hematuria usually follows intercurrent mucosal infection, usually upper respiratory tract infection. • Usually is visible within 24 hours of the onset of the symptoms of infection. IgA Nephropathy Clinical manifestation • • • • Macroscopic hematuria Asymptomatic hematuria and proteinuria Proteinuria and nephrotic syndrome Acute renal failure: Crescentic IgA glomerulonephritis>> STEROIDS!!! • Chronic renal failure • The Most Common Cause of GN in the world. Diffuse Glomerulonephritis • Affects most or all of the glomeruli • Heavy proteinuria, red cell casts, edema, hypertension, and Renal Insufficiency. • Aggressive treatment Diffuse GN • Less than 15 yrs: postinfectious GN, MPGN • 15-40 yrs: Postinfectious, Lupus Nephritis • Greater than 40 yrs: Vasculitis( including cryoglobulinemia), Postinfectious GN. Diffuse GN associated with Hypocomplementemia • • • • Postinfectious GN Lupus-nephritis Membranoproliferative GN( MPGN) Mixed cryoglobulinemia • Hypocomplementemia in GN is most often due to complement activation by immune-deposits. Postinfectious GN • Post-streptococcal pharyngitis • Endocarditis • Infected Ventricular shunt • Pyoderma Postinfectious GN(PSGN) • Ac. GN can develop 2-3 weeks after pharyngitis or skin infection with certain group A, B-hemolytic Streptococci. • Immune complex deposition of streptococcal antigens as well as auto-immune reactivity. • Diffuse proliferative and exudative nephritis containing many neutrophils and monocytes • Deposition of C3, IgG, IgM (Subepithelial) • Rapidly progressive renal failure with cellular crescents. Poststreptococcal Glomerulonephritis Poststreptococcal GN (Introduction) Usually occurs 10 days after pharyngitis and 14 days after skin infection (not synpharyngitic) Fallen incidence in US, but common in some rural areas, poor hygiene places, and tropical countries Occurs more often in males and children Poststreptoccal GN (nephritic strains) Known nephritic strains include M types 1, 2, 4, 12, 18, 25, 49, 55, 57, 60 Many proposed mechanisms: Molecular mimickry vs. autoimmune vs. polyclonal activation of B lymphocytes Repeat infections are not common as immunity is type specific and not usually transient Clinical Presentation Most patients have milder disease Classically, presents with overt nephritic syndrome and oliguric ARF Symptoms can include gross hematuria (100% microscopic), HA, htn (60-80%), hypervolemia, and edema (80-90%) Clinical Presentation Nephritic urinary sediment – dysmorphic RBCs, red cell casts, leukocytes, subnephrotic proteinuria Nephrotic-range proteinuria not common Post-streptococcal GN • Sometimes esp. in adults, patients may develop HTN, proteinuria and renal insufficiency>>> ESRD>>>Dialysis. Labs Serum Cr can be commonly elevated at presentation, though mild C3 and CH50 decreased w/in 2 weeks C4 usually normal (complement level usually normal within 68 weeks) Most patients have directed Ab, such as ASO, anti-DNAse B, etc Serum IgG and IgM increased in 80% and returns to normal in 1-2 months Polyclonal cryoglobulinemia in 75% Light Microscopy On light microscopy, usually see diffuse proliferative GN Immunofluorescence Microscopy Deposition of IgG and C3 3 patterns mesangial Starry sky (mesangial and capillary wall) Garland (capillary loops) Electron Microscopy large electron – dense immune deposits in subendothelial, subepithelial, and mesangial areas Course Irreversible Renal Failure rare – less than 1 % in children, slightly higher in adults Resolution usually quick, plasma Cr usually returns to previous levels by 3-4 weeks Hematuria resolves usually within 3-6 months, proteinuria falls at a slower rate Some patients experience htn, recurrent proteinuria, and renal insufficiency 10-40 yrs after > 20% of adults may have some degree of persistent proteinuria and or compromise of GFR 1 year out Treatment Eliminate strep infxn with abx Supportive therapy Diuretics and antihypertensives to control bp and extracellular fluid volume Rapidly Progressive GN (Crescentic) • RPGN describes the clinical situation in which glomerular injury is so acute and severe that renal function deteriorates over days or weeks. The patient may present as a uremic emergency, with nephritic syndrome that is not self-limiting but moves on rapidly to renal failure. • The histologic counterpart of RPGN is crescentic GN. Crescentic GN • Crescents are inflammatory collections of cells in Bowman’s space. They appear when severe glomerular injury results in local rupture of the capillary wall allowing plasma proteins and inflammatory material to escape from the capillary into Bowman’s space. Crescents consist of both proliferating parietal cells and invading inflammatory cells, both lymphocytes and monocytes/macrophages. • They are destructive, rapidly increasing in size and squeezing the glomeruli tuft until it is occluded. Rapidly progressive (Crescentic) Glomerulonephritis(RPGN) • Anti-glomerular basement membrane antibody disease( with pulmonary disease, Goodpasteure’s Syndrome). • Immune Complex-mediated GN. • Pauci-immune GN, usually ANCApositive. Therapy A. -Pulse Therapy: IV Methylprednisolone followed by PO Prednisone 1mg/Kg. -IV Cyclophosphamide or Cell-Cept Or Imuran. B. Plasmapheresis C. Hemodialysis( Hyperkalemia, Hypervolemia). Acute GN and Pulmonary Hemorrhage ANCA associated systemic vasculitis and antiGBM - common causes Also reported to occur in SLE, HSP, mixed Cryoglobulinemia Study of 88 patients with Pulmonary Hemorrhage and Nephritis: 48 ANCA, 6 Anti GBM, 7 both, 27 neither ANCA nor anti-GBM (latter group – not many causes could explain both findings) Anti-glomerular basement membrane disease and Goodpasture’s Syndrome • Anti-GBM anti-body disease is a rare autoimmune disorder associated with antibodies specific for any components of the GBM. • Characterized by rapidly progressive GN with crescentic changes that affect most glomeruli on renal biopsy. • When pulmonary hemorrhage present>>>>> Goodpsteur Syndrome !!!! Anti-GBM Disease • • • • • • • Breathlessness and cough>> Hemoptysis X-Ray >>Alveolar shadowing Carbon-Monoxide transfer factor(KCO) Low incidence 1/1000,000 20% of all RPGN Spring , early summer ANCA-Systemic vasculitis (30%) Anti-GBM Disease • Bimodal age distribution with peak incidence in the third and sixth decades. • Males>females • Influenza Vaccination: Viral Infection ?? • Most patients present with the combination of RPGN and lung hemorrhage, although 30-40% present with isolated renal involvement. • Acute nephritis • Arterial hypertension is late feature. Goodpasteur’s Disease • Disease associated with autoantibodies specific for Noncollagenous domain (NC1) of the alpha-3 chain of type (IV) collagene>>>ELISA highly sensitive and specific. • May include RPGN , lung hemorrhage, or both. Type IV collagen exists as a complex supramolecular network. Three individual 3(IV) chains are interwoven to form a triple helix, known as the protomer. The NC1 domains are arranged in a head-to-head fashion to form hexamers, and binding through the 7S domains completes the network structure. Hexamers can be dissociated to form dimers and monomers of NC1 domains, allowing identification of 3(IV)NC1 as the autoantigen (redrawn with permission from [72]). Membranoproliferative GN • Primary ( Idiopathic) • Secondary) Cryoglobulinemia) MPGN • MPGN also called mesangiocapillary glomerulonephritis. • MPGN is a renal disease characterized by diffuse mesangial proliferation and thickening of the capillary wall. MPGN • MPGN type I: Subendothelial /Mesangial Deposits ( HCV: 70-90%). • MPGN type II: Mesangial ( Dense deposit disease). • MPGN type III: Subendothelial, GBM, Subepithelial Deposits. MPGN/Etiology • • • • • • Cryoglobulinemia (type-I) Infections Complement Abnormalities or deficiencies Malignancies Chronic liver disease Collagen vascular disease MPGN /Clinically • MPGN is one of the major causes of nephrotic syndrome which include MCD, FSGS, MGN • 5-20% of all primary glomerulonephritis • May present as microscopic hematuria, nonnephrotic proteinuria (35%), nephrotic syndrome with renal insufficiency, chronically progressive glomerulonephritis (20%), or as rapidly progressive renal failure. • Systemic hypertension 50-80% • Can present with systemic cryoglobulinemia (HCV+): purpura, weakness, arthralgia. MPGN • • • • • C3 and C4 are low (type1 with cryo +) Circulating immune-complexes RF+ HCV-RNA + (PCR) KNB !! MPGN recurs in renal transplant recipients with a frequency of 20-30% in type-I, 80-90% in type-II.