Tuturial_Acute Glomerulonephritis_May 26
advertisement

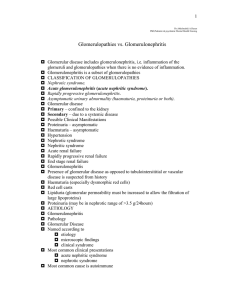
Tutorial Case Nephrology Division King Khalid University tutorial to course441 14 year old Saudi young female student C/0 fever- Headache for 10 days General malaise Dark urine x 3 days HPI Fever intermittent Muscular joint pain no skin rash urine character edema PH & Med antibiotic & NSAID Social Hx S. review FH Examination Bp : 160/90 &Pulse 120/MIN Temp 39 C Resp 25/MIN .pale Look Sick Puffiness in face Head& neck JVP high Chest: Bronchial breathing decrease Breath Rt side Increase TVF Increase Dull percussion S1 increase S2 N S3 Positive pan systolic murmur radiation to axilla grade 3 Abd tend epigastic tend lions BS + ve CNS Drawsy M.S tender joint &muscle Initial Diagnosis Fever? Infection RT lung consolidation MR HEAMATURIA: Renal stone (ARF –AKI- ATN) Acute glomerulonephritis (post infection) GN RPGN IgA Hemolytic anemia hemolytic uremic syndrome NSAID papillary necrosis Investigation WBC 15000 cells per microliter Hb 100 g/L Plat 150 g/L PT normal PPT normal Bl film Sec Sec U&E Scr 210 μmml urea 20 mmol/L K6 mmol/L Na 125 mmol/L Ca 1.9 mmol/L album 28 g/L Urine Analysis few RBC No cast Protein 1.2g/24h U/S : kid size ENLARGE 12.2CM Treatment Patient receive ceftrixone IV and IV fluid TREAT HYPERKALEMIA Follow up: S cr 300 μmml/L JVP Oliguria Edema Management: IV lasix Repeat urine analysis RBC CAST ANCA(P) positive Kidney Biopsy RPGN Final diagnosis microscopic polyangitis Glomerular Disease – Acute Glomerulonephritis Post infectious glomerulonephritis Group A Strep Infection Infective endcarditis Membranoproliferative glomerulonephritis: Systemic lupus erythematosus Hepatitis C virus Rapidly progressive glomerulonephritis Vasculitis (cryoglobulinemia Type I RPGN (direct antibody) Good Posture syndrome Type II RPGN (immune complex) Post infectious Systematic lupus erythematosus Henoch – Schonlein pupura (IgA) Others Type III RPGN (pauci-immune) o o Wegener granulomatosis Microscopic polyarteritis Investigations for Glomerulonephritis Regular Follow-up and U&E Antistreptolysin O (ASO) ANA, Anti DNA C3-C4 ANCA (p, c) HCV Antibody HBsAg HIV RF Cryoglobulin Anti-basement Membrane Antibody (With lung hemorrhage) Acute postinfection Glomerulonephritis Often associated with group A B-hemolytic streptococcal type 12 infection Abrupt onset 10-12 days after strept throat or 14-21 skin infection (impetigo) Also staphylococcus or viruses Acute Glomerulonephritis Symptoms occur 10-21 days after infection Hematuria Proteinuria Decreased GFR, oliguria Hypertension Edema around eyes, feet and ankles Ascites or pleural effusion Low C3, normal C4, Antistreptolysin O (ASO) – Kidney biopsy immune complexes and proliferation, Proliferative GN- poststretococcal This glomerulus is hypercellular and capillary loops are poorly defined. This is a type of proliferative glomerulonephritis known as poststreptococcal glomerulonephritis. Poststreptococcal GN Post-streptococcal glomerulonephritis is immunologically mediated, and the immune deposits are distributed in the capillary loops in a granular, bumpy pattern because of the focal nature of the deposition process. Post-Streptococcal Glomerulonephritis CONSERATIVE TREATMENT (acute kidney injury) Improves 1-4 weeks, C3 normalizes in 1-3 months, hypertension improves 1-3 months, intermittent hematuria x 3 years 99% complete recovery in children and 85% in adult IgA Nephropathy (Berger's Disease) Most common acute glomerulonephritis in US ;South East Asia Associated with H.S. Purpura Upper respiratory(50%) IN 1—2 Day(Synpharyngitic hematuria) Primary versus secondary (IBD, Liver Disease, SLE, vasculitis) 50% risk of CRF Proteinuria, hypertension, renal insufficiency predict worse prognosis 50% increased IgA, normal compliments TREATEMENT COSERVATIVE; ACEI HIGH RISK: patient prednisone & alkylating agent (cyclophosphamide-azothroprim) &ASA&ACEI&tosilectomy Rapidly Progressive GN Develops over a period of days or weeks Primarily adults in 50’s and 60’s Progresses to renal failure in a few weeks or months Hematuria is common, may see proteinuria, edema or hypertension Rapidly Progressive (Crescentic) Glomerulonephritis Morphology crescent formation crescents are formed by proliferation of parietal cells infiltrates of WBC’s & fibrin deposition in Bowman’s space EM reveals focal ruptures in the GBM MICROSCOPIC POLYANGITIS Necrotizing vasculitis of small- and medium- sized vessels in both the arterial and venous circulations Frequently involves the lung and the kidneys with typical complications of hemorrhage and glomerulonephritis Associated with ANCA in three-fourths of all cases, usually anti-myeloperoxidase antibodies (MPO-ANCA) that cause a P-ANCA pattern on immuno-flourescence testing. ANCA directedf againsts proteinae-3 (PR3ANCA) can also be observed in microscopic polyangiitis Treatment Initial Therapy Combination cyclophosphamide-corticosteroid therapy A slow steroid taper, with the goal of reaching 20 mg of prednisone per day by the end of two months and an overall glucocorticoid course of between 6 and 9 months. Either daily oral or monthly intravenous cyclophosphamide. Treatment Plasmapheresis Severe manifestations of pulmonary hemorrhage on presentation. Dialysis-dependent renal failure upon presentation. Concurrent anti-GBM antibodies. Goodpasture Syndrome Antibody formation against pulmonary and glomerular capillary basement membranes Damage glomerular basement membrane Men 20 - 30 years of age Pulmonary hemorrhage and renal failure TREATMENT: Early treatment is essential Pulse Steroid (10 mg/ kg/day for 3-5 days) Cyclophosphamide Plasmaphorisis Goodpasture’s syndrome This immunofluorescence micrograph shows positivity with antibody to IgG has a smooth, diffuse, linear pattern that is characteristic for glomerular basement membrane antibody with Goodpasture's syndrome.