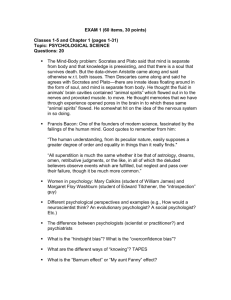
normal CNS
advertisement

Nervous system – Normal Coronal section – opening slide Gray matter runs along edge (cortex), most of the rest is white matter Gray matter: at the very edge is where we actually do our thinking, neuronal cell bodies Wires: white matter, myelinated axons carrying information Computational devices: gray matter Connection: white matter Convolutions Maximize amount of area we have: have lots of convolutions to allow for more gray matter Things that stick out: gyri (gyrus, singular) Ditches between them: sulci (sulcus, singular) General anatomy Longitudinal fissure: splits brain into right/left Cingulate gyrus: prominent anatomical landmark Corpus callosum: allows R and L sides to communicate Septum: “wall” between left & right lateral ventricles Caudate nucleus (along with globus pallidus & putamen): form the “striatum” [Latin: stripe] caudate & globus pallidus are part of basal ganglia globus pallidus & putamen form the lenticular nucleus Insula: big convolution that allows us to have even more surface area Sylvian fissure forms the insula [Latin: island] Anterior commissure: another means to communicate L to R Amygdaloidal nucleus: almond shaped nucleus, fear center (if absent, person loses inhibition) – usually just called “amygdala” Hippocampus: (next to amygdala – not shown in diagram) memory center (important that fear and memory centers are very close together in order to stay alive – we really remember danger so that we can avoid dangerous situations) Internal capsule: all information coming from cortex to body or vice versa goes through here any damage to internal capsule will have tremendous adverse effects Corona radiata: sun’s rays; fibers span out in all directions from there Neurons Only place we find pseudounipolar cells is in sensory nerves Cell body and long dendrite and axon nerve in fingertip, dendrite all way up to dorsal root ganglia (DRG) axon from DRG to spinal cord and synapse immediately or travel to brain Multipolar cells make up 99.99% of neurons; lots of dendrites As things synapse, action potential at end causes depolarization & action potential At axon terminus, calcium comes in, releases neurotransmitter, binds on postsynaptic cleft, something happens (either hyperpolarization: down or depolarization: up) Bipolar neurons are found in the eyes and ears. Axons can be myelinated (signal travels faster) or non-myelinated if supposed to be myelinated but loses it (it can no longer function; signal will travel much slower or NOT at all) Schwann cell in peripheral nervous system Oligodendrocyte: Central Nervous system 4 types of Glial cells: glue that holds brain together Astrocyte: wraps around capillary, the capillaries are completely covered by them, nothing gets out of capillary without going through astrocyte, will then contact a neuron (form blood brain barrier (BBB)) protect neurons from any potential harm that could reach neuron from blood there are a lot of drugs that don’t work in brain because can’t cross the BBB Oligodendrocytes: myelate axons in the CNS Microglial cell: macrophage, samples the environment until it finds something wrong, then becomes activated, causing an inflammatory response (activated by injury in brain; e.g. after stroke or traumatic brain injury) Ependyma cells: line ventricles and ducts that CSF flows through have cilia in them that move CSF throughout in choroid plexus, ependyma cells create CSF Don’t worry about tanycytes (nobody else does) 3 parts of brain: Cerebrum: 4 lobes of the cerebrum (named for their respective bones) Frontal Temporal Parietal Occipital Central sulcus: in front of it we have precentral gyrus, behind it the postcentral gyrus Lateral (or Sylvian) fissure separates frontal and temporal lobes Cerebellum Brainstem Midbrain Pons medulla oblongata Brodmann’s area Gray matter of cerebral cortex has 6 layers of cell types (e.g. input/output layers, processing layers, communication layers, etc) Some parts of brain looked very different from others (structure determines function) Korbinian Brodmann Systematically mapped brain (published in 1909) Assumption: neighboring slices where brain had same structure would have same function while neighboring areas that look different will have different function Don’t need to know Brodmann numbers but do need to know the names of areas on slide Some important parts of your brain Front of the brain: in front of central sulcus what you do to the world Back of the brain: what the world does to you Front of the brain Precentral gyrus: neurons of upper motor neuron (neuron that causes a muscle fiber to contract) primary somatic motor areas Premotor cortex: where we coordinate muscles in order to move smoothly, getting the sequence just right Frontal eye field: moving eyes, getting them to converge and focus, keeps movement of eyes so in sync that we do not see double even when eyes are moving quickly Broca’s area: coordinating muscles of speech, very carefully time contraction and relaxation of muscles – speech is extremely complicated muscle movements Prefrontal area: what makes you, you (least important part of your CNS; if you lost it you would be boring and not do well on tests – but you could survive) Where we make plans, store declarative memories, etc. Personality & memories of your life, etc. Back of brain is sensory Postcentral gyrus: sensory equivalent of primary somatic motor, sensing an individual sensory nerve ending primary somatic sensory cortex Visual cortex: approximately each pixel (rod or cone) has a neuron Auditory cortex: where we decode sounds – frequency decomposition of sound Association areas: putting things together Putting touch sensations together to feel things – somatic sensory association area Putting the pixels together to make pictures – visual association areas Putting sound components together to identify sounds – auditory association areas Angular gyrus: where we store information about things (what cat looks like, sounds like, feels like) Angular gyrus is very close to the key language center (Wernicke’s area) Language probably started with just nouns (names of things) Homunculus: Describing motor and sensory cortex in visual way We don’t have equitable distribution of motor or sensory neurons across the body We want to distribute neurons to where we need more precision (toes v. fingers) would rather have motor neurons controlling fingers rather than toes or back likewise need more sensory neurons for hands, mouth/face, etc. than back Corticospinal tract = most important motor tract Starts in cortex, goes to spine corticospinal Upper motor neuron: starts in motor cortex. Example, thumb control axon runs down and decussates in medulla, continues down spine and synapses in spine (cervical enlargement) lower motor neuron: starts in spinal cord. Example, thumb control runs from cervical enlargement and down to innervate muscle (e.g. abductor pollicis brevis) (80-90%) cross over in medulla, rest decussate in anterior white commissure of spinal cord, near the cell body of the lower motor neuron Both synapse in spine with the lower motor neuron runs Will not control head, face, larynx and pharynx (NOT controlled by spinal nerves, they are controlled by cranial nerves) Corticobulbar tract (Bulb: think pons (bulb out of brainstem)) Innervate the cranial nerves; upper motor neurons of lower motor neurons of cranial nerves that control skeletal muscles 1, 2, and 8 are the only cranial nerves that do NOT have motor components 3, 4, 6 – ocular muscles 5: Trigeminal: facial senses and mastication muscles 7: Facial: facial expressions (muscle component) 9: Glossopharyngeal: swallowing 10: vagus: very many functions, skeletal muscles of pharynx & palate 11: Accessory: sternocleidomastoid & trapezius 12: Hypoglossal: tongue muscles Know all the functions of the cranial nerves on slide Rubrospinal & reticulospinal tracts Modulates the action of muscles (e.g. starting/stopping action) Parkinson’s: damage to substantia nigra normal strength but trouble initiating the action resting tremors DCML (Dorsal Column Medial Lemniscus): travel up dorsal columns of spinal cord (i.e. fasciculus gracilis [legs] & fasciculus cuneatus [arms], cross at medulla, to medial lemniscus continue up lemniscus thalamus primary sensory nucleus fine touch and kinesthesis stays on same side until it reaches the medulla oblongata Spinothalamic: spinal cord to thalamus pain and temperature immediately cross over in spinal cord, up to thalamus and then up to primary sensory cortex both pathways have cell bodies in dorsal root ganglia Pain synapses and crosses immediately at spinal cord (Spinothalamic) Large fiber impulses block pain and small fiber impulses increase pain by rubbing something when it hurts you activate large fiber impulses and it blocks the pain Brain can modulate sensitivity of our sensory pathways Spend a lot of time turning off sensory processes that are not important (sitting) Descending pathways from brain control sensitivity Narcotic drugs can also block pain channels Referred pain Pain in right side and right shoulder when you run Pain in side when running is always on right side Pain in shoulder when run always right shoulder the liver is complaining (liver refers pain to right side, and right shoulder) liver is moved up and down with diaphragm Heart: radiating down left arm, possibly up to neck Kidney pain: back and flanks Spinal cord 7 cervical vertebrae but 8 cervical nerves 12 thoracic 5 lumbar 5 sacral Spinal cord running through vertebral foramen Spinal cord part of CNS dura mater, arachnoid and pia mater neurons are myelinated by oligodendrocytes 3 types of neurons enter/leave the spinal cord Somatic motor neurons Upper motor neuron synapses with lower motor neuron, lower motor neuron runs to neuromuscular junction to innervate muscle Sensory neurons nerve ending, long dendrite, cell body and dorsal root ganglion, axon enter spinal cord via dorsal horn Autonomic motor neurons axon that comes out of spinal cord, 1 synapse, postsynaptic neuron innervates end organ Dorsal (posterior): sensory Ventral (anterior): motor including motor autonomic (controls visceral functions) All nerves will contain both motor and sensory components reflex arc Hit patellar tendon: it gets dented in, lengthens muscle, signal goes back to interneuron to say muscle lengthened, interneuron says generate more force to stop muscle from lengthening When walking, at foot fall, knee is slightly bent Need to generate exact amount of force when walking, too little fall, too much hop Reflex arc allows us to generate exact amount of force to push against – without the “brain” in the loop, this is much faster and off-loads processing from the brain Somatic v. autonomic motor neurons Somatic: spinal cord has lower motor neuron that runs to skeletal muscle, nothing between except axon Autonomic: one synapse between spinal cord and end organ vagus innervating heart: neuron out of cardiorespiratory center, second neuron (post synaptic neuron controls) slows heart down or decreases contractility One synapse between CNS and organ Exception: adrenal medulla (entire body is medulla’s post synaptic neuron) whole body responds Acetylcholine: for all of the first axons, the neurotransmitter is acetylcholine For sympathetics the Second neuron transmitter is usually norepinephrine exception: sympathetic control of sweat glands uses acetylcholine at 2nd neuron For parasympathetics the second neuron transmitter is acetylcholine Autonomic nervous system Sympathetics Emerge from T1 - L2/3 No sympathetics on cranial nerves parasympathetics on cranial nerves (3, 7, 9, 10) No additional parasympathetics until we get down to sacral (usually S2 – S4) the vagus (10) controls everything below head and above descending colon sacral parasympathetics control distal colon, bladder and genitals Blood supply to brain & head Brachiocephalic (only on right side) R common carotid R subclavian L common carotid & L subclavian come directly off aorta Common carotid: split to internal and external carotid Vertebral arteries come off L & R subclavians Combine to form Basilar artery Enters skull through foramen magnum (big hole) Circle of Willis: Anterior, middle and posterior cerebral arteries Anterior and posterior communicating arteries left and right internal carotid Internal carotids give rise to L & R middle cerebral arteries Also gives rise to L & R anterior cerebral arteries basilar artery (two vertebrals came together) gives rise to L & R posterior cerebral arteries Have three ways to get blood to brain: if any one becomes blocked you still survive and have proper functioning Anterior communicating artery connects L & R anterior cerebral arteries L & R posterior communication arteries connect posterior & middle cerebral arteries Often quite a bit of variation in distribution of blood flow Distribution of blood to the brain Anterior cerebral: coming off front of circle of Willis feeds medial frontal and medial parietal lobes Middle cerebral: comes out Sylvian fissure feeds lateral sections of brain (frontal, parietal, and temporal lobes) Posterior cerebral: Feeds occipital and lower temporal lobes Ventricles & CSF Lateral, 3rd and 4th ventricles We make cerebral spinal fluid in all but mostly in lateral ventricles Choroid plexus CSF flow Lateral ventricles 3rd ventricle Cerebral aqueduct 4th ventricle From 4th ventricle: Two lateral foramina (Lushka), one medial foramen (Magendie) Circulates through brain in arachnoid region Numerous cisterns (large pools of CSF) reabsorbed by arachnoid granulation and dumped into superior sagittal sinus sinus is similar to vein, but made out of dura mater Central canal in spinal cord: usually obstructed (obstruction of no significance) CSF flow through arachnoid region CSF cushions the brain ~150 ml volume We make ~500 ml of CSF per day So we replace our CSF ~3 times per day Meninges Dura mater: tough leathery coating, adherent to skull Arachnoid mater: thin layer spider web like, CSF circulates through here Pia mater: layer closest to brain – adheres to brain