Final_Policy_Paper
advertisement

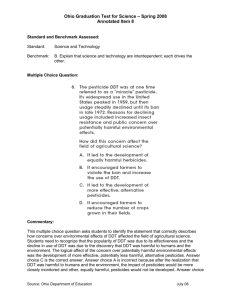
An Argument for the Birds: Banning DDT Sarah Anderson, Dylon Baker, Bethany Benike, Dane Christensen, Katrina Flaig, Tara Greiman, Adrienne Keep, Antonia Murray, Monica Sweeney, Julie Sweep Introduction Dichlorodiphenyltrichloroethane (DDT) was found to be a useful pesticide when it was discovered in Switzerland by Dr. Paul Mueller in the year 1939 (Turusov 2002). The production of DDT quickly spread throughout the United States and internationally; this mass production and use continued up until 1959 when negative impacts such as resistance to DDT, pesticide alternatives, and public awareness began to take effect (Turusov 2002 and EPA 1975). DDT was first used in World War II by the Allies to control insect vector diseases: Typhus in Europe and Malaria in the South Pacific (Dunlap 1981). Because of its efficient elimination of these two diseases, DDT became known as a “miracle cure.” Widespread controversy over DDT began with Rachel Carson’s Silent Spring, published in 1962, which condemned the use of DDT and made known the negative effects that DDT has contributed to the environment (Greenberg 1963). Silent Spring made the public aware of the negative effects of DDT and in the 1970s many of the environmental groups began campaigning against the use of DDT (Tren 2004). In 1957, the United States Department of Agriculture Forest Service banned the spraying of DDT in protective buffer zones around protected aquatic resources. In 1958 DDT was no longer used for spraying against the gypsy moth and the spruce budworm. By 1972 the Environmental Protection Agency (EPA) banned the remaining agricultural registrations for DDT(EPA 1975); this however did not ban public health and quarantine uses. In 1970, Sweden became the first country to fully ban the use of DDT. The USSR in 1981 banned its use for agricultural purposes, and later the Stockholm Convention (brought into force in 2004) completely banned the production and use of DDT (Turusov 2002; Tren 2004). Twenty-nine countries have granted exemption from using DDT and only China, India, and Russia have requested to continue to use and produce the insecticide for public health purposes (Jensen 2003). DDT is still used for disease vector control using Indoor Residual Spraying (IRS) even though the U.S. Center for Disease Control classifies DDT as a level 2B carcinogen (Roberts 1997; CDC 2002). DDT raises controversial issues because its use is seen as a quick and easy fix to some of today’s disease and agricultural issues, but it also holds implications of long-term risks associated with the environment and public health concerns. For these reasons, DDT should be banned from use: Because not only can public health be equally well protected through alternative measures, but society should also avoid the risks associated with the use of DDT. DDT Properties Toxic Composition DDT is produced by adding two chlorobenzene molecules for every one chloral hydrate molecule in a concentrated sulfuric acid solution (U.S. Department of Health and Human Services 2002, p. 221). In terms of elements that are arranged within DDT, for every one molecule there are fourteen carbon atoms, nine hydrogen atoms, and five chlorine atoms. This particular composition makes DDT a halogen organochlorine, meaning that it is extremely reactive within the environment. To clarify, chlorobenzene has been linked to several other chemical pesticides, as well as to several types of degreasers (ASTDR 1999). In addition, chloral hydrate is well known for its sedative and hypnotic drug properties, as well as its effectiveness as an adhesive and spot remover (ASTDR 2003). What makes DDT so dangerous is its insolubility in water. This property allows for bioaccumulation within the environment since water cannot wash away the substance. It can only make the substance seep further into the soil; this has environmental consequences which will be discussed later. Cheaper Than Competitors? Part of the reason DDT originally gained such popularity was its effectiveness as a contact-killer. Indeed, DDT is one of the only tested pesticides that repels, irritates, and is toxic to mosquitoes (Grieco et al. 2007). DDT also remains effective within the environment for longer periods of time relative to many other insecticides, requiring only two sprays for year round protection (Walker 347). However, findings from the same study reveal that “As a killing agent, DDT is inferior to modern insecticides which kill mosquitoes more quickly and at much lower concentrations” (Soderlund 2008, p. 612). The use of DDT is also apt to build vector resistance, making the chemical less effective. This ineffectiveness can then be true of other chemicals, as DDT-resistant mosquitoes are often resistant to pyrethroids, another common group of insecticides. As previously mentioned, DDT was hailed as a miracle drug for its ability to effectively control disease-carrying pests at a low cost. DDT is created by condensing chloral hydrate with chlorobenzene in concentrated sulfuric acid (U.S. Department of Health and Human Services 2002). All of these substances are relatively easy to obtain, making the production process costefficient. In fact, production of the chemical is so easy that some chemists were able to make the product (illegally) in their own homes (Time Magazine 1945). In 1990, DDT was considered to be 2 to 23 times cheaper than other leading pesticides on the market. However, by 1998, these numbers decreased to somewhere between 1.4 and 18.7 times cheaper (Walker 2000). Therefore, DDT’s cost advantage has been shrinking over the past decade. While current price comparisons are unavailable, DDT could very well be comparable to other pesticides in cost by 2010. A Cost-Effective Alternative However, insecticides are not the only answer to controlling malaria; there is another competitor quickly gaining favor around the world. Insecticides treated bed-nets (ITNs) have been shown to efficiently protect human lives, and can have comparable costs of use depending on the area (Walker 2000). ITN use is a more discriminating means of pesticide control because it protects individuals directly, without needing to spray the inside of every built surface as must be done with DDT (Yukich 2007). While ITNs have a comparable cost to DDT based on whole population protection, the cost of averting death and/or disability adjusted life years (DALYs) with ITNs is considerably less than with indoor residual spraying, also known as IRS (i.e., DDT use). Using the highest cost estimate of ITN use and the lowest cost estimate of IRS for death and DALY aversion, ITNs still cost 25% less to use annually (Yukich 2007). With this information, it is clear that efficient, cost-effective alternatives to DDT are available. Environmental Impacts of DDT Effects on Soil and Water DDT infiltrates the soil and water by vertical distribution in which rainfall washes DDT from the surface layer of the soil to lower soil horizons and groundwater stores (Mohapatra et al. 1995). This effect is exacerbated by plowing which mixes contaminated topsoil with lower layers (Perfect, 1980). DDT is insoluble in water enabling it to travel through water, rivers and lakes spreading contamination; after water evaporates, DDT is left on the soil where it percolates into groundwater supplies. By entering the water cycle, DDT molecules can also travel through rainfall, runoff and spray drifts (Mohapatra et al. 1995). Due to its effects on soil and water, as well as its effects on wildlife (discussed later), DDT is hazardous to surrounding natural and man-made environments. This chemical has been found to reduce decomposition rates of materials in soil, and impact the amount of surface earthworm activity, which gravely affect soil fertility (Perfect 1980). Plants which are exposed to DDT or grown in DDT exposed soils can absorb the toxin and transfer it to the stem and leaves (Perfect 1980). Together, the lower fertility of soils and the absorption of DDT by plants can lead to a decrease in plant biomass in natural areas and a lower crop yield in agricultural fields (Perfect 1980). Aside from the economic consequences of these effects, reduced biomass can have a large impact on habitat composition by disrupting natural systems and cycles (Moore 1967). Effects on Wildlife The effects of DDT on wildlife are wide-spread and well documented. Due to its long persistence bioaccumulation of DDT is common compared to many other pesticides (Williams 1970). Bioaccumulation, or food web accumulation, causes the concentration of a chemical to increase with each level of the food chain it travels through. Therefore, high order carnivores feel the effects of DDT most strongly (Williams 1970; Sherburne & Dimond 1969). DDT can affect all sorts of wildlife, from minnows to moose, in many of the same ways. For smaller organisms, even those not targeted for eradication or control, DDT can be lethal on contact (Surber 1946). DDT exposure can lead to health problems, reproductive issues, and higher susceptibility to disease. For example, there has been evidence of DDT causing cancer and cysts, primarily in mammals (Heinrichs et al. 1971). It also effects hormone production, which can lead to various health concerns, including decreased reproductive productivity, decreased metabolism, and immunosuppression (Williams 1970; Heinrichs et al. 1971; Storelli et al. 2009). Immunosuppression and the reaction of DDT with other chemicals can also make organisms more susceptible to infection, disease, and chemical poisoning (Tiedeken & Ramsdell 2009). DDT also affects the nervous systems, which can cause hyperirritability, muscular tremors, twitches, and spasms, incoordination, and even paralysis (Surber 1946; Michigan DNR 2002). All of these effects make DDT a very strong selective pressure on species (Moore 1967). Aquatic food chains are very long and complex, meaning bioaccumulation of DDT happens very quickly and at very high levels, especially in aquatic carnivores and animals which eat fish, including humans (Williams 1970; Moats and Moats 1970). This means fish, aquatic mammals, crustaceans, other aquatic organisms, and their predators are among the most heavily affected by pesticides such as DDT. The most obvious consequence of DDT on aquatic ecosystems is the poisoning of fish, which causes neurological damage starting with hyperirritability, muscular incoordination, spasms, and eventual prostration and death (Surber 1946). The presence of DDT in the water can also bring about the death of newly hatched fry (Moats & Moats 1970). Probably the most well known effect of DDT is bird egg shell thinning. This causes the eggs to crack when their parents sit on them and makes eggs more prone to cracking (Williams 1970; Grier 1982; Fry & Toone 1981; Ratcliffe 1970; Moats & Moats 1970). DDT effects the production of progesterone, which stimulates calcium transfer to the reproductive organs for egg shell production (Williams 1970). There is a chance that eggs which are not broken will become addled and fail to hatch, and those chicks that do hatch have a higher mortality rate (Moats & Moats 1970; Niering 1968). Birds can also experience feminization, in which males develop female characteristics, ultimately making them unable to breed and creating an imbalanced sex ratio (Fry & Toone 1981). Effects on Humans DDT has been found to cause adverse health effects on humans as well. There are three ways that a person can be exposed: inhalation, oral, and dermal. The inhalation of DDT is associated with lung cancer. A study was conducted on workers in five pesticide manufacturing plants. There was a significant excess of deaths from stroke, in the plant where primary exposure was DDT (ATSDR 1). Oral exposure to DDT can also alter normal hepatic metabolic enzyme activity. Neurological tests assessing cognitive, motor, and sensory functions found the dermally exposed group had overall poorer performance than the control group (ATSDR 2). Further studies have found that in utero exposure to DDT may be associated negatively with neurodevelopment of young children (Eskenazi et al. 2006). DDT may also be carcinogenic to humans (Eskenazi et al. 2009). The reproductive health of humans is also negatively effected by DDT. De Jager et al. (2006) found evidence that male reproductive health and fertility potential is influenced by nonoccupational, subchronic DDT exposure. There is also evidence of incomplete DNA condensation, indications of increased stillbirths, neonatal deaths, congenital defects in children, post-generational impacts on females, and an increase in incidence of pre-term birth and underweight babies. There is also evidence for high prevalence of urogenital birth defects due to DDT exposure. Finally, the breast milk in lactating mothers may be contaminated by DDT exposure which means that breastfed babies may exceed allowable daily intake levels (IPEN). Field workers are especially prone to these effects due to their heightened exposure to pesticides on crops. Alternatives Some possible alternatives to DDT for pest control include less hazardous pesticides which target specific species, as opposed to DDT which is a nonspecific insecticide. One example of alternatives would be Methoxychlor, which is used to control Dutch Elm disease and is much less hazardous to wildlife (Niering 1968; Moats & Moats 1970). Pesticides such as Dieldrin, Endrin, Aldrin, and Lindane were found to be much less persistent than DDT, though many of them have some of the same detrimental effects and Dieldrin and Endrin are more toxic (Beyer & Gish 1980; Fleming et al. 1982; ATSDR). Along with those listed, there are many other available pesticides which all have their positive and negative attributes. Another option would be the use of natural pest control such as organic pesticides, natural predators, and ITNs. Because these viable alternatives exist, there is no reason to continue to endanger wildlife and humans with the long-lasting toxic effects of DDT. Public Health Typhus The main cause of typhus was largely unknown until recent medical advances, and thus, little was known about preventing or curing the disease. Lice are the main transmission vector by which humans are infected with typhus, and when an infected louse bites a person, typhus is transmitted to the host through bacteria in the saliva. After contracting the disease, the human host will experience a long-term fever, and without proper medical intervention, death. Since lice prefer hosts with body temperature at or near 98.6 degrees Fahrenheit, an infected louse quickly moves to a new host after their old one has experienced extreme changes in body temperature associated with typhus infection (Medline 2009). Consequently, the spread of typhus is directly linked to dense populations and the ease of the louse finding a new target. Ever since humans have lived in dense urban environments, typhus has been a public health concern. Some scholars claim the first major outbreak of typhus can be attributed to the Athenian Plague of 430 B.C. (Conlon). And since the Dark Ages, every century has experienced a large typhus outbreak in cities across the world. As Joseph Conlon stated, “in crowded tenements, prisons, refugee camps, or under conditions or times of war or disaster, when prisoners, refugees, or troops are unable to change clothes or bath regularly, lice may spread rapidly through the entire population. This is particularly true during the winter, when bathing is made more difficult by the cold weather” (Conlon). In most of these situations, people did not understand what caused typhus and how it was transmitted to other humans. As a result, typhus is linked to areas with dense urban environments, poor sanitation levels, and little knowledge about how diseases are transmitted. The transmission of typhus is now fully understood and can be prevented by washing or boiling clothes, living in clean and sanitary conditions, having good personal hygiene, and in some cases, the use of pesticides like DDT (Medline 2009). Since lice serve as the transmission vector for typhus into human populations, eradication of the louse is the best method to prevent typhus outbreaks. Poor sanitation on both an individual and societal level helps lice species grow to large numbers and encourage their spread into human populations. Proper personal hygiene by bathing regularly and washing or boiling clothes is the best method to remove lice and prevent their arrival on human bodies. On a societal level, proper removal of waste and adequate sanitation limits the population of rodent species that may carry infected lice. This is particularly true for dense urban environments that produce a lot of human waste and garbage. In 2009, Tajikstan, Central Asia’s poorest country, experienced a typhus outbreak that numbered over 100 cases. Areas of the world that are experiencing dramatic growth without adequate city planning are particularly vulnerable to outbreaks of deadly diseases like typhus. In countries with economies similar to Tajikstan, governments may not be able to afford large-scale water treatment plants and sewage systems. In these societies, public education initiatives may prove to be a cheaper alternative in preventing typhus outbreaks than redesigning entire city sewage systems. In some civilizations, the access to resources may not be available to discourage the spread of typhus. Societies with limited or partial access to water sources may not be able to bathe as often as privileged societies. As Conlon mentioned earlier, some societies may not be able to bathe as frequently during the winter months because of the cold. However, proper personal hygiene in the summer months would keep the lice of the body until winter arrived. As long as humans were not living in crowded tenements with rodents, the typhus-carrying lice would die off during these winter months. Educating people about cleanliness and the animals that carry typhus would greatly reduce the number of world-wide outbreaks. Ultimately, public education about the vectors that transmit typhus may be the best and least costly preventative measures against a deadly outbreak. Malaria As Malaria becomes an increasingly global issue, the scientific and political community have come together to further develop existing standards for prevention and the successful diagnosis of this disease. From previous research, we know that Malaria is mainly transmitted from person to person through the bite of the female Anopheles mosquito; An. culicifacies, An. funestus, and An. gambiae. Successful malarial prevention has to then incorporate a multilayered system which includes proper education on both the individual and community responsibilities for rural, semi-rural, and urban environments. Parallel to prevention is the clinical diagnosis for malarial infections. In areas where malaria either is, or has been endemic, the problems for public health workers include the classification of disease severity and ultimately the correct diagnosis and treatment to patients. Procedural guidelines have been made into official policy by the National Malarial Control Programme (NMCP), the World Health Organization (WHO) and individual national health regulations in response to reported confusion between clinics and laboratories on irregularities between patient analyses. For the purpose of this paper, I will be focusing the discussion on the past and present forms of public health and the resulting economics of the situation mainly in India and Sub-Saharan Africa. The NMCP has created four procedures which are done before an outbreak: (1) indoor residual spraying with DDT and other insecticides (IRS), (2) insecticide-treated nets (ITN), (3) larval control and (4) case detection and effective treatmenti. Malaria frequency is mainly influenced by the practices of both the individual and the community in terms of personal protection. In richer communities, the majority of which are found in urban environments, the household would follow the first preventative measure, as listed by NMCP; indoor residual spraying on their walls and furniture with DDT as the most common insecticide. For many people in high risk malarial zones, this first procedure would be too expensive. Taking economics into consideration, state governments and charities have given the poorest communities free prevention materials; the most common of which would be insecticide-treated bed netting. The use of nets while sleeping has become increasingly common, due mainly to its obvious help in deterring mosquito blood meals. The application of DDT to the nets is not a universal procedure, though it is listed as one by NMCP and, historically, the use of this insecticide has been the best method for malarial defense. Multiple scientific surveys (Baume 2009; Gu 2009; Rowe 2009; Satoguina 2009) have compared the competence of insecticide and non-insecticide infused nets in keeping the inhabitants safe. What their research has concluded is that whether the net is treated is not as important as how the net was being usedii. In most cases, the use of insecticide did not exhibit an overtly increased ability to hinder malarial infection. (Sataguina 2009). However, government programs continue to promote the usage of the more expensive insecticide treated nets. “The proportion of cases and controls using bed nets did not exceed 25%, in the absence of systematic activities of distribution before the [malarial] outbreak. The health authorities of Naxalbari [Angola] distributed 5,000 insecticide-treated bed nets among the affected population in October 2005.” (Rowe 2009; 21) In reaction to the overuse of insecticides for malarial control in endemic areas, there have been reports of a possible resistance to DDT by An. culicifacies (Sharma 2005). In the near future, as more research develops on this possibility, the use of insecticide treated nets becomes inconsequential. Instead, an increased effort of instruction for the population on malarial prevention needs to be enacted; both the lay person and to those in the medical field. For rural and semi-rural communities, the education has focused on controlling their environment so as to better prevent malaria. As many of these communities are below the poverty line, the best way for them to protect their household is to trim all vegetation around the house, decrease their proximity to mosquito habitats and wearing protective clothing (Carme 2009). These simple steps, if completed properly, would help communities to combat against the disease which is a major variable of inducing their poverty. As preventative measures are continuously being debated and enacted on the global and local levels, the massive case loads for public health officials, clinics, and laboratories continue to be a major problem for successful diagnosis and treatment of malaria. Rowe et al, (2009), classifies the disease into two categories. In order to identifying which class the patient belongs, the doctor must look for signs of fever and/or headaches, joint pain, chills, sweating, anemia, cough (occurs only in children), anorexia, fatigue, vomiting, or diarrhea. Once the initial diagnosis has been completed, they can move the patient into one of the two diagnosis categories: 1) Uncomplicated malaria, which is present without signs of severe illness, and 2) Complicated malaria, where the patient exhibits at least one sign of severe illness. Since 2000, due to the increasing resistance to chloroquine and other regularly used antimalarial medication, 45 African countries have made Artemisinin-Based Combination Therapy (ACT) into public health policy, announcing that this is the first course of action when battling uncomplicated malaria. (Rowe et al. 2009) However, after its execution, there have been weaknesses in the policy which make it nearly un-usable. Mainly that the public health sector is lacking both the funds and credible manpower to maintain the policy as it was written. Rowe et al (2009) defined the standard for assessing the quality of malaria testing, diagnosis, and treatment as a challenge because: 1) policy and training materials sometimes lacked precision; 2) the survey protocol did not include testing for all patients who should have been tested; and 3) the NMCP (National Malarial Control Programme) policy had recently underwent a revision. The ACT policy included government sponsored training for all public health workers, however there continues to be confusion based on the specific criterion for correctly diagnosing malaria. In 2000, when the policy was first initiated, clinics would look to both the policy and the official documents published from the World Health Organization (WHO) in order to fill in the gaps left out of ACT. Confusion arouse specifically when a child (5>) or a pregnant woman, was brought to the clinic presenting mild to severe fever. Since neither were mentioned or given correct procedural guidelines on how to treat, along with the encouragement of healthcare workers to reduce patient discomfort, many took this to mean that any cases which fall to either patient precondition was to be treated with an anti-malarial. As of 2007, health policy underwent another rewrite in order to better encompass a universal plan of action when health care workers were faced with children (5>) and pregnant women. They employed an “analysis algorithm” which was to help workers create a “gold standard” in determining what the diagnosis and treatment for the various stages (mild or severe) of malaria. The new standard used the test results of a microscopy and of Rapid Diagnostic Tests (RDTs) ordered by the clinic (Rowe 2009). What it does not use are laboratory results. By approaching each case in this new “golden standard” format, it allows for the best adherence to official guidelines, since it prevents the condemnation of public health workers if the clinical results do not match laboratory results. As scientific research continues to combat malaria, the multi-layered system of prevention and diagnosis is helping the at-large population to be better prepared for possible endemics. The use of DDT is no longer seen as the only possible gauge for prevention of the disease. Because of this, communities are looking towards alternatives to harmful insecticides’. With an increase of malaria education programs in poorer regions, each household has the responsibility to apply the new lessons in reducing possible mosquito habitats and personal protection. Though malaria continues to be a modern plague in tropical zones, the combined efforts made by the scientific and governmental communities have made great leaps in combating this disease. DDT Use and Other Approaches Typhus DDT has commonly been used in contemporary societies as a pesticide to kill lice and other insects that transmit diseases. While DDT is a cheap and easily manufactured pesticide that may be a great deterrent for typhus and malaria outbreaks, there are also some physiological and environmental side-effects associated with its use. Studies have shown that there is a correlation between DDT use and asthma among human populations. Additionally, DDT does not easily dissipate from the soil because of its chemical structure, posing long-term risks to the environment. Although DDT has been an effective method to eradicate animals that may be carrying diseases, there are other ways of preventing these diseases that makes the use of DDT unnecessary and inherently more risky. Under adequate medical facilities, typhus can be treated and cured with proper medications. “Today, with good supportive care and early judicious use of antibiotics such as the tetracyclines, quinilones, chloramphenicol, and paraaminobenzoicacid, the risk of a fatal issue is greatly reduced” (Conlon). While typhus can be easily treated if recognized early, the long term effects of DDT exposure are more difficult to diagnose and treat medically. Given that the use of DDT can possibly cause more problems than it prevents, and the long-term risks it poses to human populations and the environment at large, it may be more ethical and beneficial for humanity by treating outbreaks of typhus with antibiotics instead of using harmful pesticides as a preventative measure. Malaria Countries worldwide have implemented various techniques in preventing the outbreaks of deadly diseases such as malaria. Each strategy must take into account how the virus is transferred. When the malaria parasite Plasmodium resides within their host, the Anopheles mosquito, the transmission vector enters human populations by the host’s blood meal. In effect, a reduction or elimination of mosquito populations would be the best preventative measure against malarial endemics. Traditionally, DDT and the use of other insecticides have been common practice for reducing the number of Anopheles mosquitoes. However, due to the toxic classification of insecticides, safer alternatives could be used to either complement or replace the overall use of DDT. As malaria endemics have been given worldwide attention during the past decade, the United Nations Environmental Programme (UNEP) has been at the forefront of negotiations for the discontinuation of DDT and called for nations throughout the high-risk zones to ban its use altogether. Universal education by health authorities to all levels of the society is the safest and most productive alternative to DDT use. While it is likely that the majority of persons living in and around malaria zones understand that the disease is transmitted via mosquitoes, they may not understand how to reduce their chances of getting bit. One of the most important concepts a community should consider is the mosquito’s habitat and its preference to breed in standing water (i.e. forgotten well, livestock water basins). By reducing the insect’s habitat, they would also be reducing their risk of a possible endemic. As DDT and other Persistent Organic Pollutants have proven to be detrimental to the surrounding environment, UNEP has created the Integrated Vector Management (IVM) program. IVM supports the systematic approach to malarial control in high-risk regions whereupon community participation is a key contributor alongside safe prevention materials. The program continues to promote the use of bed nets, screens over windows and doors, roof boards (in regions where that is necessary), and the burning of mosquito coils. Per design specifications, UNEP has made this program cost-effective. Meaning that even in the poorest areas afflicted with malaria, there is always the option to undertake IVM, without having to use DDT and other Persistent Organic Pollutants. Conclusion Admittedly, DDT is cheap and efficient for controlling insect vectors and pests. However, the costs of DDT are so great and the risks so many, that it is impossible to justify the use of this dangerous chemical when viable alternatives exist. The long persistence and likelihood of bioaccumulation in animal tissues and the environment make DDT a hazard to species across the globe from tiny fish fry to the great eagle, and even human beings. Entire webs of life can be altered by the effects of DDT in water and terrestrial environments. Malaria and typhus are horrible diseases with widespread effects across the globe. However, DDT is not the only solution to controlling their spread. Education, screens or ITNs, and alternative insecticides are all farsighted and effective measures to protecting human health against disease transmission. From these points, it is apparent that DDT use is an outdated and dangerous habit that the planet must kick. All of these factors prove that DDT use is most costly and the environment than alternative measures. Works Cited "Ddt Contamination in South Africa." International POP's Elimination Network (IPEN), http://www.ipen.org/ipepweb1/library/ipep_pdf_reports/5saf%20ddt%20contamination% 20in%20south%20africa.pdf. “Ddt and Other Chlorinated Hydrocarbon Pesticides." In Michigan Wildlife Disease Manual: Michigan Department of Natural Resources, 2002. Agency for Toxic Substance and Disease. (ATSDR). July 2003. 09 December 2009 <http://www.atsdr.cdc.gov/tfacts19.pdf> Agency for Toxic Substances and Disease Registry (ATSDR). 1. "Public Health Statement for Aldrin/Dieldrin." http://www.atsdr.cdc.gov/toxprofiles/phs1.html#bookmark03. Agency for Toxic Substances and Disease Registry (ATSDR). 2. "Toxicological Profile for Ddt, Dde, and Ddd." http://www.atsdr.cdc.gov/toxprofiles/tp35.html. Agency for Toxic Substances and Disease. (ATSDR). July 1999. 05 December 2009 <http://www.atsdr.cdc.gov/tfacts131.pdf> Baume, Carol, Richard Reithinger and Sara Woldehanna. 2009. Factors Associated with the Use and Non-Use of Mosquito Nets Owned in Oromia and Amahara Regional States, Ethiopia. Malaria Journal 8:264-280. Beyer, W. Nelson, and Charles D. Gish. "Persistence in Earthworms and Potential Hazards to Birds of Soil Applied Ddt, Dieldrin and Heptachlor." Journal of Applied Ecology 17, no. 2 (1980): 295-307. Carme, Bernard. 2009. Malaria or Kalimbe: How to Choose?. Malaria Journal 7:280-289. CDC. 2002. Toxicology Profile for DDT, DDE and DDD. In Toxicology Profiles: Centers for Disease Control. http://www.atsdr.cdc.gov/toxprofiles/tp35.pdf. Accessed Nov 2009 De Jager, Christiaan, Paulina Farias, Albino Barraza-Villarreal, Mauricio Hernandez Avila, Pierre Ayotte, Eric Dewailly, Christian Dombrowski, Franc Ois Rousseau, Vicente Diaz Sanchez, and Janice L. Bailey. "Reduced Seminal Parameters Associated with Environmental Ddt Exposure and P,P'-Dde Concentrations in Men in Chiapas, Mexico: A Cross-Sectional Study." Journal of Andrology 27 (2006): 16-27. Dunlap, Thomas R. 1981. DDT : Scientists, citizens, and public policy. Princeton, N.J.: Princeton University Press. EPA. 1975. DDT : a review of scientific and economic aspects of the decision to ban its use as a pesticide : prepared for Committee on Appropriations, U.S. House of Representatives. Washington : U.S. Environmental Protection Agency. Eskenazi, Brenda, Amy R. Marks, Asa Bradman, Laura Fenster, Caroline Johnson, Dana B. Barr, and Nicholas P. Jewell. "In Utero Exposure to Dichlorodiphenyltrichloroethane (Ddt) and Dichlorodiphenyldichloroethylene (Dde) and Neurodevelopment among Young Mexican American Children." Pediatrics 118, no. 1 (2006): 233-41. Eskenazi, Brenda, Jonathan Chevrier, Lisa Goldman Rosas, Henry A. Anderson, Maria S. Bornman, Henk Bouwman, Aimin Chen, Barbara A. Cohn, Christiaan de Jager, Diane S. Henshel, Felicia Leipzig, John S. Leipzig, Edward C. Lorenz, Suzanne M. Snedeker, and Darwin Stapleton. "The Pine River Statement: Human Health Consequences of Ddt Use." Environmental Health Perspectives 117 (2009): 1359-67. Fleming, W. James, M. Anne Ross McLane, and Eugene Cromartie. "Endrin Decreases Screech Owl Productivity." The Journal of Wildlife Management 46, no. 2 (1982): 462-68. Fry, D. Michael, and C. Kuehler Toone. "Ddt-Induced Feminization of Gull Embryos." Science 213, no. 4510 (1981): 922-24. Grieco, J.P., Achee, N.L., Chareonviriyaphap, T., Suwonkerd, W., Chauhan, K., et al. (2007) A New Classification System for the Actions of IRS Chemicals Traditionally Used For Malaria Control. PLoS ONE 2(8): e716. doi:10.1371/journal.pone.0000716 Grier, James W. "Ban of Ddt and Subsequent Recovery of Reproduction in Bald Eagles." Science 218, no. 4578 (1982): 1232-35. Gu, Weidong. 2009. Predicting the Impact of Insecticide-Treated Bed Nets on Malaria Transmission: The Devil is in the Detail. Malaria Journal 8:256-266. Heinrichs, W. L., R. J. Gellert, J. L. Bakke, and N. L. Lawrence. "Ddt Administered to Neonatal Rats Induces Persistent Estrus Syndrome." Science 173, no. 3997 (1971): 642-43. Jensen, J. K. 2003. DDT. United States Environmental Protection Agency, Office of Pesticide Programs, Washington DC, USA. Moats, Sheila A., and William A. Moats. “Towards Safer Use of Pesticides.” BioScience 20, no. 8 (1970): 459-464. Mohapatra, Satya P., Mukesh Kumar, Vijay T. Gajbhiye, and Narendra P. Agnihotri. "Ground Water Contamination by Organochlorine Insecticide Residues in a Rural Area in the Indo-Gangetic Plain." Environmental Monitoring and Assessment 35, no. 2 (1995): 15564. Moore, N. W. "Effects of Pesticides on Wildlife." Proceedings of the Royal Society of London. Series B, Biological Sciences 167, no. 1007 (1967): 128-33. Niering, William A. "The Effects of Pesticides." BioScience 18, no. 9 (1968): 869-75. Perfect, John. "The Environmental Impact of Ddt in a Tropical Agro-Ecosystem." Ambio 9, no. 1 (1980): 16-21. Ratcliffe, D. A. "Changes Attributable to Pesticides in Egg Breakage Frequency and Eggshell Thickness in Some British Birds." Journal of Applied Ecology 7, no. 1 (1970): 67-115. Roberts, D. R., L. L. Laughlin, P. Hsheih, and L. J. Legters. 1997. DDT, global strategies, and a malaria control crisis in South America. Emerging Infectious Diseases 3:295-302. Rowe, Alexander, et al. 2009. Quality of Malaria Case Management at Outpatient Health Facilities in Angola. Malaria Journal 7:200-241. Satoguina, Judith, et al. 2009. Comparison of Surveillance Methods Applied to a Situation of Low Malaria Prevalence at Rural Sites in The Gambia and Guinea Bissau. Malaria Journal 9: 274-286. Science: Homemade DDT. Time Magazine. August 6, 1945. Accessed: November 14, 2009 <http://www.time.com/time/magazine/article/0,9171,803716,00.html> Sherburne, J. A., and J. B. Dimond. "Ddt Persistence in Wild Hares and Mink." The Journal of Wildlife Management 33, no. 4 (1969): 944-48. Soderlund, D.M. "Pyrethroids, knockdown resistance and sodium channels." Pest Management Science 64 (2008): 610-16. Print. Storelli, Maria Maddalena, Arianna Storelli, Grazia Barone, and Delia Franchini. "Accumulation of Polychlorinated Biphenyls and Organochlorine Pesticide in Pet Cats and Dogs: Assessment of Toxicological Status." Science of the Total Environment 408, no. 1 (2009): 64-68. Surber, Eugene W. "Effects of Ddt on Fish." The Journal of Wildlife Management 10, no. 3 (1946): 183-91. Tren, Richard, and Roger Bate. 2004. South Africa's War Against Malaria: Lessons for the Developing World. In Policy Analysis: Cato Institute. http://www.degroenerekenkamer.nl/grkfiles/pa513.pdf. Accessed Nov 2009 Turusov, Vladimir, Valery Rakitsky, and Lorenzo Tomatis. 2002. Dichlorodiphenyltrichloroethane (DDT): Ubiquity, Persistence, and Risks. Environmental Health Perspectives 110 (2):125-128. U.S. Department of Health and Human Services. (2002). Toxicological Profile for DDT, DDE, and DDD. Federal Register. United Nations Environmental Programme. 2009. Towards DDT-Free Malaria Control Leaflet. http://www.unep.org/PDF/UNEP_GEFMalariaLeaflet.pdf, accessed December 10, 2009. Walker, K. August 18, 2000. Cost-comparison of DDT and alternative insecticides for malaria control. Medical and Veterinary Entomology, 14. 345-354. Williams, Ray E. “DDT: Hero or Villain?” The American Biology Teacher 32, no. 1 (1970): 1113. Yamamoto, Shelby S., et al. 2009. The Effects of Zooprophylaxis and Other Mosquito Control Measures Against Malaria in Nouna, Burkina Faso. Malaria Journal 8:283-300. Yukich, J., Tediosi, F., Lengeler, C. Operations, costs and cost-effectiveness of five insecticidetreated net programs (Eritrea, Malawi, Tanzania, Togo, Senegal) and two indoor residual spraying programs (Kwa-Zulu-Natal, Mozambique). USAID. July 12, 2007. i When there is an endemic, the contaminated areas are visited by public health workers bi-weekly, whereupon they collect the blood samples of each person in the home. As per government procedure, public health workers also take blood smears if a person only has a fever. (Sharma 2005) ii In each survey, scientists talked with multiple households within their perspective community and found that many were using the nets incorrectly. Either the nets were not installed correctly or the family had been saving the nets for special situations (i.e. visitors). (Gu 2009; Rowe 2009)