pyelonephritis - Department of Library Services
advertisement

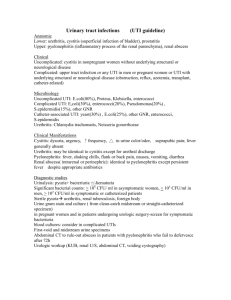
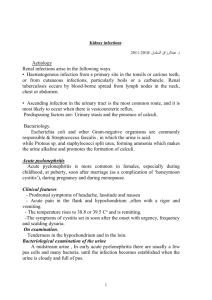
Database: Ovid MEDLINE(R) <1996 to March Week 3 2010> Search Strategy: -------------------------------------------------------------------------------1 *pyelonephritis/di (192) 2 acute disease/ (74069) 3 acute.tw. or 2 (357406) 4 1 and 3 (95) 5 limit 4 to (male and "all infant (birth to 23 months)") (21) 6 from 5 keep 1-21 (21) *************************** <1> Unique Identifier 19620428 Status MEDLINE Authors Brenner M. Bonta D. Eslamy H. Ziessman HA. Authors Full Name Brenner, Michele. Bonta, Dacian. Eslamy, Hedieh. Ziessman, Harvey A. Institution Russell H. Morgan Department of Radiology, Division of Nuclear Medicine, Johns Hopkins University and Johns Hopkins Outpatient Center, 601 N Caroline St., JHOC Rm. 3231, Baltimore, MD 21287, USA. Title Comparison of 99mTc-DMSA dual-head SPECT versus high-resolution parallel-hole planar imaging for the detection of renal cortical defects. Source AJR. American Journal of Roentgenology. 193(2):333-7, 2009 Aug. Abstract OBJECTIVE: Renal cortical scintigraphy with (99m)Tc dimer captosuccinic acid (DMSA) is the standard method to detect acute pyelonephritis and cortical scarring. Different acquisition methods have been used: planar parallel-hole or pinhole collimation and single photon emission tomography (SPECT). Publications support the superiority of each; few comparative studies have been reported, with mixed results. We have compared planar parallel-hole cortical scintigraphy and dual-head SPECT for detection of cortical defects. MATERIALS AND METHODS: Forty patients (37 children, 3 adults; 9 male, 31 female) were imaged 3 hours after injection of (99m)Tc-DMSA with dual-head SPECT and planar imaging (posterior, left, and right posterior oblique views with a parallel-hole collimator). For each patient, planar and SPECT images were evaluated at different sittings, in random order, by three independent observers. Twelve cortical segments were scored as normal or reduced uptake. The linear correlation coefficient for the number of abnormal segments detected between readers, techniques, and segments was calculated. RESUlTS: No significant difference was seen in the average number of abnormal segments detected by planar versus SPECT imaging; 2.1 for planar imaging and 2.2 for SPECT (p = 0.84, two-tailed). For all observers, the average correlation coefficient for SPECT alone, planar imaging alone, and between techniques (SPECT vs planar imaging) was high (r = 0.93-0.94). Applying nonparametric Spearman's rank analysis, the average correlation remained high (r = 0.70-0.75). Correlation between readers, techniques, and segments for methods and readers was also good (r = 0.69-0.77). CONClUSION: (99m)Tc-DMSA renal cortical imaging using dual-head SPECT offers no statistically significant diagnostic advantage over planar imaging for detection of cortical defects. Publication Type Comparative Study. Journal Article. <2> Unique Identifier 19395784 Status MEDLINE Authors Mohkam M. Asgarian F. Fahimzad A. Sharifian M. Dalirani R. Abdollah Gorgi F. Authors Full Name Mohkam, Masoumeh. Asgarian, Fahimeh. Fahimzad, Alireza. Sharifian, Mostafa. Dalirani, Reza. Abdollah Gorgi, Fatemeh. Institution Pediatric Infectious Research Center, Shahid Beheshti University (MC), Tehran, Iran. mohkamm@yahoo.com Title Diagnostic potential of urinary tumor necrosis factor-alpha in children with acute pyelonephritis. Source Iranian journal of Kidney Diseases. 3(2):89-92, 2009 Apr. Abstract INTRODUCTION. Tumor necrosis factor-alpha (TNF-alpha) is an important mediator of the inflammatory response in serious bacterial infections. The aim of this study was to evaluate the potential of urinary TNF-alpha for diagnosis of acute pyelonephritis in children. MATERIALS AND METHODS. This study was conducted from March 2006 to December 2007 on children with confirmed diagnosis of acute pyelonephritis. They all had positive renal scintigraphy scans for pyelonephritis and leukocyturia. The ratios of urinary TNF-alpha to urine creatinine level were determined and compared in patients before and after antibiotic therapy. RESULTS. Eighty-two children (13 boys and 69 girls) with acute pyelonephritis were evaluated. The mean pretreatment ratio of urinary TNF-alpha to urinary creatinine level was higher than that 3 days after starting on empirical treatment (P = .03). The sensitivity of this parameter was 91% for diagnosis of acute pyelonephritis when compared with demercaptosuccinic acid renal scintigraphy as gold standard. CONCLUSIONS. Based on our findings in children, the level of urinary TNF-alpha-creatinine ratio is acute increased in pyelonephritis and it decreases after appropriate therapy with a high sensitivity for early diagnosis of the disease. Further research is warranted for shedding light on the potential diagnostic role of urinary TNF-alpha in pyelonephritis in children. Publication Type Journal Article. Research Support, Non-U.S. Gov't. <3> Unique Identifier 19367005 Status MEDLINE Authors Mohkam M. Karimi A. Habibian S. Sharifian M. Authors Full Name Mohkam, Masoumeh. Karimi, Abdollah. Habibian, Saiid. Sharifian, Mostafa. Institution Pediatric Infectious Research Center, Shaheed Beheshti University of Medical Sciences, Tehran, Iran. mohkamm@yahoo.com Title Urinary N-acetyl-beta-D-glucosaminidase as a diagnostic marker of acute pyelonephritis in children. Source Iranian journal of Kidney Diseases. 2(1):24-8, 2008 Jan. Abstract INTRODUCTION: Prompt diagnosis and localization of pyelonephritis are of great importance in children. The urinary excretion of enzymes, and in particular N-acetyl-beta-Dglucosaminidase (NAG), is considered a simple noninvasive marker for detection of renal tubular dysfunction due to pyelonephritis. This study was performed to determine the diagnostic value of urinary NAG in acute pyelonephritis. MATERIALS AND METHODS: In a quasi-experimental study conducted on 72 children with confirmed pyelonephritis, we measured urinary NAG, creatinine, and NAG-creatinine ratio before and after the treatment. Diagnostic values of these parameters were evaluated by considering the patients before and after the treatment as disease- positive and disease-negative groups, respectively. RESULTS: The patients were 18 boys (25.0%) and 54 girls (75.0%) with a mean age of 43.0 +/- 39.0 months. The mean levels of urinary NAG were 12.20 +/- 6.14 U/L and 5.46 +/- 7.98 U/L before and after the treatment, respectively (P < .001). The sensitivity and specificity of urinary NAG-creatinine ratio for diagnosis of pyelonephritis were 73.6% and 77.3%, respectively, with a cutoff point of 10.16 U/g (area under the curve = 0.76, 95% confidence interval, 0.67 to 0.76). Significantly higher levels of urinary NAG were found in those who had a negative urine culture at diagnosis (8.8 +/- 10.4 U/L) compared to those with a positive urine culture (4.5 +/- 8.7 U/L). CONCLUSIONS: We concluded that urinary NAG is elevated in children with pyelonephritis and it can be considered as a further criterion in the diagnosis of upper urinary tract infection. Publication Type Evaluation Studies. Journal Article. Research Support, Non-U.S. Gov't. <4> Unique Identifier 18761823 Status MEDLINE Authors Roed C. Friis-Moller A. Hogh B. Authors Full Name Roed, Casper. Friis-Moller, Alice. Hogh, Birthe. Institution Hogh Hvidovre Hospital, Borneafdelingen, Hvidovre. casperroed@hotmail.com Title [A study of the validity of urinary tract infection diagnosis in children younger than two years of age at Hvidovre Hospital]. [Danish] Source Ugeskrift for Laeger. 170(33):2432-4, 2008 Aug 11. Abstract INTRODUCTION: The aim of this study is to validate the diagnosis of urinary tract infection (UTI) concerning false-positive diagnoses in children younger than two years of age at Hvidovre Hospital. MATERIALS AND METHODS: The material consists of 89 children (50 girls and 39 boys) diagnosed with acute pyelonephritis from September 2002 until October 2004. Two patients dropped out as they were diagnosed in other countries. The patient records were investigated to identify the children who fulfilled the UTI criteria used in the department: 1) Two mid-stream urine samples with bacterial growth of = 10.000 cfu (colony forming units)/cc, 2) growth of = 100 cfu/cc in urine obtained by a suprapubic puncture of the bladder or 3) a midstream urine sample with bacterial growth of = 10.000 cfu/cc and a clinical picture of UTI together with elevated inflammatory laboratory parameters. RESULTS: 70 out of 87 patients (80%, 95% confidence limits 70-88%) had a valid UTI diagnosis. CONCLUSION: We consider a diagnostic validity of 80% as satisfactory although our aim is to increase the validity to 90%. Publication Type English Abstract. Journal Article. Validation Studies. <5> Unique Identifier 18040727 Status MEDLINE Authors Rodriguez LM. Robles B. Marugan JM. Suarez A. Santos F. Authors Full Name Rodriguez, Luis Miguel. Robles, Belen. Marugan, Jose Manuel. Suarez, Angeles. Santos, Fernando. Institution Department of Paediatrics, Leon Hospital, Leon, Spain. luism@arrakis.es Title Urinary interleukin-6 is useful in distinguishing between upper and lower urinary tract infections. Source Pediatric Nephrology. 23(3):429-33, 2008 Mar. Abstract This study was designed to determine whether the measurement of interleukin (IL)-6 in urine is useful for distinguishing between acute pyelonephritis and lower urinary tract infection. This observational study was carried out at Leon Hospital (Spain) on 35 patients (ten boys) aged between 0 and 14 years with urinary tract infection. Urinary levels of IL-6 were determined with enzyme-linked immunosorbent assay (ELISA) at diagnosis and after recovery. Renal dimercaptosuccinate acid (DMSA) scan was performed on all patients to discard or confirm acute pyelonephritis. The mean urinary concentration [x +/- standard deviation (SD)] of IL-6 at diagnosis was 20.3 +/- 23.3 and 5.3 +/- 9.7 pg/ml in patients with acute pyelonephritis and lower urinary infection, respectively [95% confidence interval (CI): 2.6-27.4; p < 0.01]. Specificity for a value of IL-6 >15 pg/ml, was 94.1% (95% CI: 91.1-97.1). Positive predictive value for IL-6 >15 pg/ml was 87.5% (95% CI: 81.1-93.8). IL-6 was undetectable in the urine of both groups of patients at the time of recovery. Urinary levels of IL-6 are useful in differentiating between upper and lower urinary tract infection in children. In this clinical setting, a value >15 pg/ml is a strong indicator of acute pyelonephritis. Publication Type Journal Article. Research Support, Non-U.S. Gov't. <6> Unique Identifier 18087632 Status MEDLINE Authors Huang DT. Huang FY. Tsai TC. Tsai JD. Chiu NC. Lin CC. Authors Full Name Huang, Daniel Tsung-Ning. Huang, Fu Yuan. Tsai, Tsuen Chiuan. Tsai, Jeng Daw. Chiu, Nan Chang. Lin, Chun Chen. Institution Department of Pediatrics, Mackay Memorial Hospital, Taipei, Taiwan. Title Clinical differentiation of acute pyelonephritis from lower urinary tract infection in children. Source Journal of Microbiology, Immunology & Infection. 40(6):513-7, 2007 Dec. Abstract BACKGROUND AND PURPOSE: To evaluate clinical variables for diagnosing childhood acute pyelonephritis (APN) when technetium-99m dimercaptosuccinic acid (DMSA) scintigraphy is not available. METHODS: We retrospectively reviewed the records of 590 children with febrile UTI seen from January 1999 to February 2004. On the basis of DMSA scintigraphy performed within 7 days after admission, they were divided into APN (n = 237) or non-APN (n = 353) groups. Gender, age, clinical presentation, absolute neutrophil count, C-reactive protein (CRP), urinalysis, culture, and sonographic findings were recorded from charts. RESULTS: A CRP level of > or =66.4 mg/L, in patients with >2 days prior to admission had a sensitivity of 71.6% and a specificity of 72.5% for APN. Similarly, a CRP of >27.3 mg/L in patients with < or =2 days prior to admission and a white cell count of >14,990/mm3 had sensitivities of 68.6% and 62.0% and specificities of 66.1% and 63.0%, respectively. Combining two or more variables did not result in better discrimination. CONCLUSIONS: If a DMSA scan is not available, it is reasonable to treat a febrile UTI as APN if the CRP is >66.4 mg/L in a patient with >2 days of fever or if the CRP is >27.3 mg/L in a patient febrile for < or =2 days. Publication Type Journal Article. <7> Unique Identifier 17727746 Status MEDLINE Authors Van den Bruel A. Aertgeerts B. Bruyninckx R. Aerts M. Buntinx F. Authors Full Name Van den Bruel, Ann. Aertgeerts, Bert. Bruyninckx, Rudi. Aerts, Marc. Buntinx, Frank. Institution Department of General Practice, Katholieke Universiteit and CEBAM, Belgian Centre for Evidence Based Medicine, Leuven, Belgium. ann.vandenbruel@med.kuleuven.be Title Signs and symptoms for diagnosis of serious infections in children: a prospective study in primary care. Source British Journal of General Practice. 57(540):538-46, 2007 Jul. Other ID Source: NLM. PMC2099636 Abstract BACKGROUND: Serious infections in children (sepsis, meningitis, pneumonia, pyelonephritis, osteomyelitis, and cellulitis) are associated with considerable mortality and morbidity. In children with an acute illness, the primary care physician uses signs and symptoms to assess the probability of a serious infection and decide on further management. AIM: To analyse the diagnostic accuracy of signs and symptoms, and to create a multivariable triage instrument. DESIGN OF STUDY: A prospective diagnostic accuracy study. SETTING: Primary care in Belgium. METHOD: Children aged 0-16 years with an acute illness for a maximum of 5 days were included consecutively. Signs and symptoms were recorded and compared to the final outcome of these children (a serious infection for which hospitalisation was necessary). Accuracy was analysed bivariably. Multivariable triage instruments were constructed using classification and regression tree (CART) analysis. RESULTS: A total of 3981 children were included in the study, of which 31 were admitted to hospital with a serious infection (0.78%). Accuracy of signs and symptoms was fairly low. Classical textbook signs (meningeal irritation impaired peripheral circulation) had high specificity. The primary classification tree consisted of five knots and had sensitivity of 96.8% (95% confidence interval [CI] = 83.3 to 99.9), specificity 88.5% (95% CI = 87.5 to 89.5), positive predictive value 6.2% (95% CI = 4.2 to 8.7), and negative predictive value 100.0% (95% CI = 99.8 to 100.0), by which a serious infection can be excluded in children testing negative on the tree. The sign paramount in all trees was the physician's statement 'something is wrong'. CONCLUSION: Some individual signs have high specificity. A serious infection can be excluded based on a limited number of signs and symptoms. Publication Type Journal Article. Multicenter Study. Research Support, Non-U.S. Gov't. <8> Unique Identifier 16894326 Status MEDLINE Authors Guven AG. Kazdal HZ. Koyun M. Aydn F. Gungor F. Akman S. Baysal YE. Authors Full Name Guven, Ayfer G. Kazdal, Halis Z. Koyun, Mustafa. Aydn, Funda. Gungor, Frat. Akman, Sema. Baysal, Yunus Emre. Institution Department of Paediatrics, Akdeniz University, School of Medicine, Antalya, Turkey. Title Accurate diagnosis of acute pyelonephritis: How helpful is procalcitonin?. Source Nuclear Medicine Communications. 27(9):715-21, 2006 Sep. Abstract AIM: This prospective study aimed to investigate the diagnostic value of serum procalcitonin levels in children with acute pyelonephritis documented by Tc-dimercaptosuccinic acid (DMSA) scintigraphy. METHODS: We compared the symptoms and laboratory findings of fever, vomiting, abdominal/flank pain, leukocyte count, serum C-reactive protein and procalcitonin levels with the results of the DMSA scan obtained within the first 72 h after referral in children who were diagnosed as having acute pyelonephritis. Thirty-three children (31 female and two male) aged 1-11 years (mean 4.42 years) were enrolled in this prospective study. RESULTS: Twenty-one of 33 patients (64%) had positive DMSA scans. On the scans obtained after 6 months, five of 21 patients (23.8%) had renal scars. No correlation was found between clinical and laboratory parameters, alone or combined with each other, and positive DMSA scans. Serum procalcitonin levels were 0.767+/-0.64 and 1.23+/-1.17 ng . ml in children with normal and positive DMSA scans, respectively. The cut-off value for procalcitonin using receiver operating characteristic analysis was 0.9605 ng . ml, while sensitivity and specificity were 86.4% and 36.4%, respectively. However, if the cut-off value was chosen as 2 ng . ml, the sensitivity increased to 100% while specificity did not change markedly. CONCLUSION: The serum procalcitonin test, like other commonly used laboratory parameters, e.g. serum C-reactive protein and white blood cell count, was inadequate in distinguishing renal parenchymal involvement in acute febrile urinary tract infections. Publication Type Journal Article. Research Support, Non-U.S. Gov't. <9> Unique Identifier 16791804 Status MEDLINE Authors Chroustova D. Palyzova D. Urbanova I. Kolska M. Authors Full Name Chroustova, Daniela. Palyzova, Daniela. Urbanova, Irena. Kolska, Monika. Institution Department of Nuclear Medicine, University Hospital Kralovske Vinohrady and 3rd School of Medicine, Charles University, Prague, Czech Republic. chroust@fnkv.cz Title Results of a five-year study of 99mTc DMSA renal scintigraphy in children and adolescents following acute pyelonephritis. Source Nuclear Medicine Review. 9(1):46-50, 2006. Abstract BACKGROUND: Renal scintigraphy, generally using 99mTc-DMSA, is the accepted reference standard for detection of renal cortical changes. The timing of the test, i.e., whether an acute 99mTc-DMSA scan, a follow-up only or both scans should be performed, however, remains open to discussion. In our study, a six-month follow- up DMSA scan was performed in all the children diagnosed with a first attack of acute pyelonephritis (APN) in two large paediatric clinics of Charles University's 3rd School of Medicine in Prague during a five-year period. All diagnoses were confirmed by a paediatric nephrologist. MATERIAL AND METHODS: 382 children (267 girls, 115 boys) aged between 7 months and 19 years were included in the study. For analytical purposes, the patients were divided into 4 age groups: I--less than 1 year of age, II--1-5 years, III-5-10 years, and IV--10-19 years. In all children younger than five years, a micturition cystourethrogram (MCUG) for detection of vesicoureteric reflux (VUR) was performed between one and three months after the APN episode. Static renal scintigraphy, using an HR collimator with parallel holes was performed using a planar Gamma camera MB 9200 (Gamma Budapest) in all children six months after APN, with a complement of pinhole images, SPECT or PSPECT of the kidneys. RESULTS: 1. In group I, all four children with positive VUR on MCUG had a pathological DMSA scan, while only two of the 32 patients with negative VUR had a pathological DMSA. 2. In group II, 17 children had VUR on MCUG, six of them with a pathological and 11 with a normal DMSA scan. Most of the 221 children without VUR had a normal DMSA scintigraphy; pathological findings were present in 17 children only. 3. In group III, all children with VUR, but only 5 out of 53 without VUR, had a pathological DMSA scan. 4. Five out of 50 children in group IV had a pathological DMSA. CONCLUSIONS: APN occurred most frequently in group II (62.3%, or 238 children) and ranged between 10-15% in the remaining groups. APN was found very frequently in boys less than one year old and showed a marked decrease with increasing age. Among girls, however, APN incidence was observed to increase with age. Pathological renal changes were present in children with, as well as without, VUR. The incidence of pathological DMSA findings six months after APN was relatively low (44/382 patients, or 11.5%). Regular monitoring of these children is very important for detection of renal scarring. Publication Type Journal Article. <10> Unique Identifier 15893462 Status MEDLINE Authors Bigot S. Leblond P. Foucher C. Hue V. D'Herbomez M. Foulard M. Authors Full Name Bigot, S. Leblond, P. Foucher, C. Hue, V. D'Herbomez, M. Foulard, M. Institution Clinique de pediatrie, hopital Jeanne-de-Flandre, Lille, France. sandra_bigot@hotmail.com Title [Usefulness of procalcitonin for the diagnosis of acute pyelonephritis in children]. [French] Source Archives de Pediatrie. 12(7):1075-80, 2005 Jul. Abstract BACKGROUND: Acute pyelonephritis can induce parenchymal scarring. The aim of this study was to evaluate the usefulness of procalcitonin (PCT) to predict renal involvement in febrile children with urinary tract infection (UTI). METHODS: In a prospective study serum PCT was measured and compared with others commonly used inflammatory markers in children admitted to the emergency unit with acute pyelonephritis. Renal parenchymal involvement was assessed by a (99 m)Tc-labeled dimercaptosuccinic acid (DMSA) renal scar performed in the first 3 days after the admission. RESULTS: Among 42 enrolled patients, 19 (45%) had acute renal involvement (Group A) ; 23 (55%) (Group B) had normal DMSA scan (n = 16), or old scarring (n = 4) or various anomalies related to uropathy (n = 3). In group A, the mean PCT level was significantly higher than in the group B (5.4 ng/ml, vs 0.4 ng /ml, p < 10(-5)). In these 2 groups, mean C reactive protein (CRP) levels were 99.1 mg/l and 44.6 mg/l respectively (p < 0.001). For a level of serum PCT > or = 0.5 ng/ml, the sensitivity and specificity to predict the renal involvement were 100% and 87% respectively; for a level> or= 20 mg/l CRP had a sensitivity of 94% but a specificity of 30%. CONCLUSION: Serum PCT levels were significantly increased in febrile children with UTI when acute renal parenchymal involvement was present. PCT seems a better marker than CRP for the prediction of patients at risk of renal lesions. Publication Type English Abstract. Journal Article. <11> Unique Identifier 15286264 Status MEDLINE Authors Pecile P. Miorin E. Romanello C. Falleti E. Valent F. Giacomuzzi F. Tenore A. Authors Full Name Pecile, Paolo. Miorin, Elisabetta. Romanello, Carla. Falleti, Edmondo. Valent, Francesca. Giacomuzzi, Francesco. Tenore, Alfred. Institution Department of Pediatrics, School of Medicine, University of Udine, Piazzale S.M. della Misericovolio Udine 33100, Italy. paolo.pecile@uniud.it Title Procalcitonin: a marker of severity of acute pyelonephritis among children. Source Pediatrics. 114(2):e249-54, 2004 Aug. Abstract OBJECTIVE: Febrile urinary tract infection (UTI) is a common problem among children. The diagnosis and management of acute pyelonephritis is a challenge, particularly during infancy. The distinction between acute pyelonephritis and UTI without renal involvement is very important, because renal infection may cause parenchymal scarring and thus requires more aggressive investigation and follow-up monitoring. However, this distinction is not easy among children, because common clinical findings and laboratory parameters are nonspecific, especially among young children. In an attempt to differentiate acute pyelonephritis from febrile UTI without renal lesions in a group of 100 children, we measured serum levels of procalcitonin (PCT), a new marker of infection. The objective of the study was to determine the accuracy of PCT measurements, compared with C-reactive protein (CRP) measurements, in diagnosing acute renal involvement during febrile UTI and in predicting subsequent scars, as assessed with 99mTc-dimercaptosuccinic acid (DMSA) scintigraphy. DESIGN: Serum CRP levels, erythrocyte sedimentation rates, leukocyte counts, and PCT levels were measured for 100 children, 1 month to 13 years of age, admitted for suspected febrile UTI (first episode). Renal parenchymal involvement was evaluated with DMSA scintigraphy within 5 days after admission. The DMSA study was repeated 6 months later if the initial results were abnormal. RESULTS: The mean PCT level was significantly higher in acute pyelonephritis than in UTI without renal lesions (4.48 +/- 5.84 ng/mL vs 0.44 +/- 0.30 ng/mL). In these 2 groups, the mean CRP levels were 106 +/- 68.8 mg/L and 36.4 +/- 26 mg/L, mean erythrocyte sedimentation rates were 79.1 +/- 33 mm/hour and 58.5 +/- 33 mm/hour, and leukocyte counts were 18 492 +/- 6839 cells/mm3 and 16 741 +/- 5302 cells/mm3, respectively. For the prediction of acute pyelonephritis, the sensitivity and specificity of PCT measurements were 83.3% and 93.6%, respectively; CRP measurements had a sensitivity of 94.4% but a specificity of only 31.9%. Positive and negative predictive values for prediction of renal involvement with PCT measurements were 93.7% and 83% and those with CRP measurements were 61.4% and 83.3%, respectively. When inflammatory markers were correlated with the severity of the renal lesions, as assessed with DMSA scintigraphy, a highly significant correlation with both PCT and CRP levels was found. However, when the 2 parameters were correlated with renal scarring in follow-up scans, a significant positive association was found only for PCT levels. CONCLUSIONS: Serum PCT levels may be a sensitive and specific measure for early diagnosis of acute pyelonephritis and determination of the severity of renal parenchymal involvement. Therefore, this measurement could be useful for the treatment of children with febrile UTIs, allowing prediction of patients at risk of permanent parenchymal renal lesions. Publication Type Clinical Trial. Comparative Study. Journal Article. <12> Unique Identifier 12792386 Status MEDLINE Authors Prat C. Dominguez J. Rodrigo C. Gimenez M. Azuara M. Jimenez O. Gali N. Ausina V. Authors Full Name Prat, Cristina. Dominguez, Josep. Rodrigo, Carlos. Gimenez, Montse. Azuara, Marta. Jimenez, Orlando. Gali, Nuria. Ausina, Vicenc. Institution Serveis de Microbiologia, Hospital Universitari Germans Trias i Pujol, C/Canyet s/n, 08916 Badalona, Spain. crisprat@ns.hugtip.scs.es Title Elevated serum procalcitonin values correlate with renal scarring in children with urinary tract infection. Source Pediatric Infectious Disease Journal. 22(5):438-42, 2003 May. Abstract BACKGROUND: Urinary tract infection (UTI) in young children carries the risk of parenchymal damage and sequelae. The location of the infection within the urinary tract influences decisions regarding both therapeutics and follow-up. Because clinical features and laboratory markers of infection at an early age are not specific, it is difficult to make a distinction between lower UTI and acute pyelonephritis. Procalcitonin (PCT) has been studied as a marker of severe bacterial infection. The aim of this study was to test the usefulness of PCT concentration in serum to distinguish between uncomplicated UTI and severe acute pyelonephritis with renal scars. METHODS: PCT was measured by immunoluminometric assay in serum samples from children with microbiologically documented infection. Severe renal involvement was assessed by 99mTc-dimercaptosuccinic acid gammagraphy done 5 to 6 months after the episode to check for the presence of parenchymal scars. C-reactive protein (CRP) and leukocyte count were also measured. RESULTS: PCT at presentation showed a significant correlation (P < 0.001) with the presence of renal scars in children with UTI. Using a cutoff of 1 ng/ml for PCT and 20 mg/l for CRP, sensitivity and specificity in distinguishing between urinary tract infection with and without renal damage were 92.3 and 61.9%, respectively, for PCT and 92.3 and 34.4% for CRP. Positive and negative predictive values were 32 and 97.5%, respectively, for PCT and 23 and 95%, respectively, for CRP. CONCLUSIONS: A low PCT value at admission indicates a low risk of long term renal scarring. Increased PCT values at admission correlate with the presence of scars. PCT values have proved to be more specific than CRP and leukocyte count for identifying patients who might develop renal damage. Publication Type Comparative Study. Journal Article. <13> Unique Identifier 12775285 Status MEDLINE Authors Lai SW. Ng KC. Authors Full Name Lai, Shih-Wei. Ng, Kim-Choy. Institution Department of Community Medicine, China Medical College Hospital, Taichung City, Taiwan. Title Retrospective analysis of inflammatory parameters in acute pyelonephritis. Source Scandinavian Journal of Urology & Nephrology. 37(3):250-2, 2003. Abstract OBJECTIVE: Different parameters were compared in children with acute pyelonephritis in order to facilitate the early detection of vesicoureteral reflux (VUR) in primary healthcare settings. MATERIAL AND METHODS: This was a cross-sectional, hospital-based study. A total of 149 children with confirmed acute pyelonephritis were retrospectively analyzed between January 1999 and December 2000. The primary factors studied were body temperature, Creactive protein level, white blood cell count and neutrophil ratio. RESULTS: The study population comprised 82 males (55.0%) and 67 females (45.0%). The mean age of the patients was 2.7 +/- 3.9 years (age range 1 day to 18 years; 75% <3 years old). Of 123 patients who underwent voiding cystourethrography, 34 (27.6%) had VUR. When raised C-reactive protein, leukocytosis and raised neutrophil ratio occurred together, the specificity and positive predictive value for predicting VUR were obviously increased, but sensitivity was radically decreased. After controlling for the other covariates, multivariate logistic regression analysis showed that factors significantly related to VUR were age (odds ratio = 1.3, 95% confidence interval 1.02-1.67; p < 0.05) and raised neutrophil ratio (odds ratio = 4.2, 95% confidence interval 1.1-16.5; p < 0.05). CONCLUSIONS: Our findings emphasize that the prevalence of VUR in children with acute pyelonephritis is extremely high. If a raised neutrophil ratio is observed, the potential risk of VUR is significantly increased in patients with clinically suspected acute pyelonephritis. Hence, the neutrophil ratio is recommended as an excellent parameter for predicting VUR. Publication Type Journal Article. <14> Unique Identifier 12771787 Status MEDLINE Authors Weiser AC. Amukele SA. Leonidas JC. Palmer LS. Authors Full Name Weiser, Adam C. Amukele, Samuel A. Leonidas, John C. Palmer, Lane S. Institution Division of Pediatric Urology, Schneider Children's Hospital/Long Island Jewish Medical Center, New Hyde Park, New York, USA. Title The role of gadolinium enhanced magnetic resonance imaging for children with suspected acute pyelonephritis. Source Journal of Urology. 169(6):2308-11, 2003 Jun. Abstract PURPOSE: The diagnosis of pyelonephritis is primarily clinical. However, the history and physical findings can be confusing in children, leading to adjunctive nuclear renal cortical scintigraphic studies (99mtechnetium dimercapto-succinic acid [DMSA]) to confirm the diagnosis. Nonetheless, ambiguity occurs when differentiating between acute pyelonephritis and chronic scarring. We report our initial experience with gadolinium enhanced inversion recovery magnetic resonance imaging (MRI) to diagnose acute pyelonephritis. MATERIALS AND METHODS: Nine patients 7 months to 18 years old (mean age 81 months) underwent MRI to confirm radiographically a clinical suspicion of acute pyelonephritis. All patients had at least 1 prior episode of clinical pyelonephritis. Data were collected to determine whether acute pyelonephritic changes could be differentiated from chronic pyelonephritis on the basis of MRI characteristics. RESULTS: Of the 9 patients 4 were identified as having acute pyelonephritis on MRI (persistently high signal intensity after gadolinium), 2 demonstrated evidence of postpyelonephritic scar (parenchymal loss without change in signal intensity), 1 had evidence of acute pyelonephritis and chronic changes, and 2 had a completely normal examination (decreased signal intensity after gadolinium). At our institution the billable cost of MRI to the patient is $1,329, while the billable cost of 99mtechnetium DMSA is $1,459. All patients younger than 6 years required intravenous sedation for MRI, whereas 70% of those younger than 6 years require intravenous sedation for DMSA scanning at our institution. MRI provided greater anatomical detail regarding the renal architecture without radiation exposure, and allowed the unambiguous diagnosis of acute versus chronic pyelonephritis scar in a 1-time (versus often multipart for DMSA) imaging study. CONCLUSIONS: In cases where adjunctive imaging studies are useful to make a diagnosis gadolinium enhanced inversion recovery magnetic resonance imaging allows the detection of acute pyelonephritis rapidly, cost-effectively and safely in the pediatric population. Publication Type Journal Article. <15> Unique Identifier 12529459 Status MEDLINE Authors Hoberman A. Charron M. Hickey RW. Baskin M. Kearney DH. Wald ER. Authors Full Name Hoberman, Alejandro. Charron, Martin. Hickey, Robert W. Baskin, Marc. Kearney, Diana H. Wald, Ellen R. Institution Department of Pediatrics, University of Pittsburgh School of Medicine and Children's Hospital of Pittsburgh, Pittsburgh 15213-2583, USA. hoberman@chp.edu Title Imaging studies after a first febrile urinary tract infection in young children. Comments Comment in: N Engl J Med. 2003 May 1;348(18):1812-4; author reply 1812-4; PMID: 12724491], Comment in: N Engl J Med. 2003 Jan 16;348(3):251-2; PMID: 12529467], Comment in: N Engl J Med. 2003 May 1;348(18):1812-4; author reply 1812-4; PMID: 12728914], Comment in: N Engl J Med. 2003 May 1;348(18):1812-4; author reply 1812-4; PMID: 12728913] Source New England Journal of Medicine. 348(3):195-202, 2003 Jan 16. Abstract BACKGROUND: Guidelines from the American Academy of Pediatrics recommend obtaining a voiding cystourethrogram and a renal ultrasonogram for young children after a first urinary tract infection; renal scanning with technetium-99m-labeled dimercaptosuccinic acid has also been endorsed by other authorities. We investigated whether imaging studies altered management or improved outcomes in young children with a first febrile urinary tract infection. METHODS: In a prospective trial involving 309 children (1 to 24 months old), an ultrasonogram and an initial renal scan were obtained within 72 hours after diagnosis, contrast voiding cystourethrography was performed one month later, and renal scanning was repeated six months later. RESULTS: The ultrasonographic results were normal in 88 percent of the children (272 of 309); the identified abnormalities did not modify management. Acute pyelonephritis was diagnosed in 61 percent of the children (190 of 309). Thirty-nine percent of the children who underwent cystourethrography (117 of 302) had vesicoureteral reflux; 96 percent of these children (112 of 117) had grade I, II, or III vesicoureteral reflux. Repeated scans were obtained for 89 percent of the children (275 of 309); renal scarring was noted in 9.5 percent of these children (26 of 275). CONCLUSIONS: An ultrasonogram performed at the time of acute illness is of limited value. A voiding cystourethrogram for the identification of reflux is useful only if antimicrobial prophylaxis is effective in reducing reinfections and renal scarring. Renal scans obtained at presentation identify children with acute pyelonephritis, and scans obtained six months later identify those with renal scarring. The routine performance of urinalysis, urine culture, or both during subsequent febrile illnesses in all children with a previous febrile urinary tract infection will probably obviate the need to obtain either early or late scans. Copyright 2003 Massachusetts Medical Society Publication Type Clinical Trial. Journal Article. Multicenter Study. Randomized Controlled Trial. Research Support, Non-U.S. Gov't. <16> Unique Identifier 12107804 Status MEDLINE Authors Smolkin V. Koren A. Raz R. Colodner R. Sakran W. Halevy R. Authors Full Name Smolkin, Vladislav. Koren, Ariel. Raz, Raul. Colodner, Raul. Sakran, Waheeb. Halevy, Raphael. Institution Pediatric Nephrology Unit, B Ha'Emek Medical Center, Afula, Israel. vlsmolkin@yahoo.com Title Procalcitonin as a marker of acute pyelonephritis in infants and children. Comments Comment in: Pediatr Nephrol. 2003 Jul;18(7):726; PMID: 12721819] Source Pediatric Nephrology. 17(6):409-12, 2002 Jun. Abstract In the absence of specific symptomatology in children, the early diagnosis of acute pyelonephritis is a challenge, particularly during infancy. In an attempt to differentiate acute pyelonephritis from lower urinary tract infection (UTI), we measured serum procalcitonin (PCT) levels and compared these with other commonly used inflammatory markers. We evaluated the ability of serum PCT levels to predict renal involvement, as assessed by dimercaptosuccinic acid (DMSA) scintigraphy. Serum C-reactive protein (CRP), leukocyte counts, and PCT levels were measured in 64 children admitted for suspected UTI. Renal parenchymal involvement was assessed by (99m)Tc-DMSA scintigraphy in the first 7 days after admission. In acute pyelonephritis, the median PCT level was significantly higher than in the lower UTI group (3.41, range 0.36-12.4 microg/l vs. 0.13, range 0.02-2.15 microg/l, P<0.0001). In these two groups, respectively, median CRP levels were 120 (range 62-249 mg/l) and 74.5 (range 14.5-235 mg/l, P=0.012) and leukocyte counts were 15,910/mm(3) (range 10,200-26,900) and 14,600/mm(3) (range 8,190-26,470, P=0.34). For the prediction of acute pyelonephritis, the sensitivity and specificity of PCT were 94.1% and 89.7%, respectively; CRP had a sensitivity of 100%, but a specificity of 18.5%. We conclude that serum PCT may be an accurate marker for early diagnosis of acute pyelonephritis. Publication Type Journal Article. <17> Unique Identifier 12089883 Status MEDLINE Authors Pacanowska B. Jarmolinski T. Zimon T. Dudarenko G. Authors Full Name Pacanowska, Beata. Jarmolinski, Tomasz. Zimon, Tomasz. Dudarenko, Grazyna. Institution Oddzial Nefrologii ze Stacja Dializ, Specjalistycznego Samodzielnego Publicznego Zakladu Opieki Zdrowotnej nad Dzieckiem i Mlodzieza w Szczecinie. Title [Acute pyelonephritis--clinical picture and the main diagnostic and therapeutic problems in children]. [Polish] Source Polski Merkuriusz Lekarski. 12(70):261-4, 2002 Apr. Abstract The aim of the study was to determine the main clinical and organising difficulties affecting quality and efficacy of medical care in children with acute pyelonephritis (AP). 41 children aged 3 wk--17 yr 4 mo hospitalized for AP at the Department of Nephrology, District Children's Hospital, Szczecin, Poland in 2000 were investigated. Epidemiologic and demographic data, history, clinical presentation, auxiliary investigations, treatment and ambulatory follow-up were analysed. Instead of typical clinical picture neither diagnostic management nor the therapy fulfilled accepted standards. The main problems found were: delay of referral to hospital by primary care doctor, misdiagnosis or inaccurate primary diagnosis followed by insufficient treatment, difficulties with performing simple ambulatory tests (urinalysis, urine culture, ultrasonography) before hospitalisation and lack of co-operation between parents and nephrological outpatient clinic after discharge. For reflux and obstructive nephropathy, often presenting as urinary tract infection, are still the main cause of chronic renal failure in children in Poland the special attention was paid to necessity of thorough education of family doctors in the subject of management of such cases as well as improvement of accessibility to specialistic care. Publication Type English Abstract. Journal Article. <18> Unique Identifier 11793131 Status MEDLINE Authors Ilyas M. Mastin ST. Richard GA. Authors Full Name Ilyas, Mohammad. Mastin, Suzanne T. Richard, George A. Institution Division of Nephrology, Department of Pediatrics, College of Medicine, University of Florida, Gainesville, FL 32610-0296, USA. Title Age-related radiological imaging in children with acute pyelonephritis. Source Pediatric Nephrology. 17(1):30-4, 2002 Jan. Abstract Accurate diagnosis of acute pyelonephritis (APN) using clinical and laboratory parameters is often difficult in children. The aims of this retrospective study were twofold. Firstly, to correlate the clinical and laboratory manifestations of APN with the results of the dimercaptosuccinic acid (DMSA) renal scan in different age groups. Secondly, to compare the DMSA renal scan, renal ultrasonography (RUS), and voiding cystourethrography (VCUG) in patients with clinical APN. The DMSA renal scan was utilized as the gold standard for renal involvement. We determined the sensitivity of these tests in febrile urinary tract infections (UTI) in three age groups: group I less than 2 years; group II 2-8 years; group III older than 8 years. During the period January 1992 through December 1998, 222 children presented with a febrile UTI. All patients had a DMSA renal scan, 208 had contrast VCUG, and 163 had RUS. The clinical and laboratory manifestation of pyelonephritis correlated better with a positive DMSA renal scan in the older children than in the younger children; 85% of the DMSA renal scans were positive in group III; 69% in group II; 48% in group I (P<0.001). Vesicoureteral reflux detected by contrast VCUG was more prevalent in the younger age groups. Although high grades of reflux (grade IV-V) correlated better with a positive DMSA renal scan, it did not reach a level of statistical significance (P>0.05). RUS did not correlate with a positive DMSA renal scan in any age group. Publication Type Journal Article. <19> Unique Identifier 10654988 Status MEDLINE Authors Fretzayas A. Moustaki M. Gourgiotis D. Bossios A. Koukoutsakis P. Stavrinadis C. Authors Full Name Fretzayas, A. Moustaki, M. Gourgiotis, D. Bossios, A. Koukoutsakis, P. Stavrinadis, C. Institution P&A Kyriakou Children's Hospital, Second Department of Pediatrics, University of Athens, Thibon and Levadias St,Goudi, Athens 115-27, Greece. march193@hol.gr Title Polymorphonuclear elastase as a diagnostic marker of acute pyelonephritis in children. Source Pediatrics. 105(2):E28, 2000 Feb. Abstract OBJECTIVE: Experimental evidence suggests that neutrophils and their metabolites play an important role in the pathogenesis of pyelonephritis. The aim of this study was to investigate the diagnostic value of polymorphonuclear elastase-a(1)-antitrypsin complex (E-a(1)-Pi) for the detection of acute pyelonephritis in children. METHODS: Eighty-three patients, 29 boys and 54 girls, 25 days to 14 years of age, with first-time symptomatic urinary tract infection were prospectively studied. Fifty-seven healthy children served as controls. Dimercaptosuccinic acid (DMSA) scan and voiding cystourethrography were performed in all patients. Plasma and urinary E-a(1)-Pi, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), neutrophil count, urinary N-acetyl-beta-glucosaminidase (NAG), N-acetyl-beta-glucosaminidase b (NAG b), and creatinine levels were measured in all patients on admission and 3 days after the introduction of antibiotics. The same markers were also measured in the control subjects. RESULTS: Planar DMSA scintigraphy demonstrated changes of acute pyelonephritis in 30 of 83 children (group A). It was normal in the remaining 53 children (group B). The sex and age distributions were not significantly different between the 2 groups, as well as between the patients and the control subjects (group C). Nineteen of the 53 children with a normal DMSA had body temperature >/=38 degrees C, whereas all but 4 children with abnormal DMSA had temperature >/=38 degrees C. Therefore, the temperature was significantly different between these 2 groups. The sensitivity and specificity of fever (>/=38 degrees C) as an indicator of renal involvement based on isotopic findings were 86% and 64%, respectively. Given the significant number of the febrile children with normal DMSA scintiscans, group B was subdivided into B(1) with 19 febrile children (14 boys and 5 girls) and B(2) with 34 children whose body temperature was below 38 degrees C (8 boys and 26 girls). The sex and age distribution was significantly different between groups B(1) and B(2). The mean age of group B(1) was.78 years (range: 28 days to 9 years; median:.25 years; standard deviation: 2.1). All but 1 child in this group were younger than 1 year of age. In contrast, in group B(2), there were only 4 infants, the remaining 30 children were older than 2.5 years (mean age: 6 years; median: 7 years; standard deviation: 3.5; range: 34 days to 12 years). The mean duration of fever before hospital admission was 2.8 days for group A and 1.8 days for group B(1). This difference was not statistically significant. Similarly, body temperature was not significantly different between these 2 groups. The distribution of plasma E-a(1)-Pi values was normal in the control subjects. The sensitivity and specificity of plasma E-a(1)-Pi, as an indicator of renal involvement, were 96% and 50%, respectively, taking the 95th percentile of the reference range as a cutoff value. However, considering as a cutoff value the level of 72 microg/dL (95th percentile of group B(2)), its sensitivity and specificity were 74% and 86%, respectively. Plasma E-a(1)-Pi levels were significantly elevated in group A compared with group B and in both groups, the plasma E-a(1)Pi values were significantly higher than in the control subjects. A significant difference also was noticed between group A and each of the subgroups B(1) and B(2) and also between the subgroups themselves. Plasma E-a(1)-Pi concentrations correlated significantly with neutrophil count in groups A (r =.3), B (r =.4), and B(2) (r =.46), but the correlation was not significant in group B(1.) ESR levels showed, among the different groups, similar differences with those of Ea(1)-Pi values. Unlike E-a(1)-Pi, CRP levels were comparable between groups A and B(1), which both consisted of febrile children. Neutrophil count was not significantly different between subgroups B(1) and B(2). (ABSTRACT TRUNCATED) Publication Type Journal Article. <20> Unique Identifier 9832579 Status MEDLINE Authors Benador N. Siegrist CA. Gendrel D. Greder C. Benador D. Assicot M. Bohuon C. Girardin E. Authors Full Name Benador, N. Siegrist, C A. Gendrel, D. Greder, C. Benador, D. Assicot, M. Bohuon, C. Girardin, E. Institution Department of Pediatrics, Children's Hospital, Geneva, Switzerland. Title Procalcitonin is a marker of severity of renal lesions in pyelonephritis. Source Pediatrics. 102(6):1422-5, 1998 Dec. Abstract OBJECTIVE: In an attempt to differentiate acute pyelonephritis from lower urinary tract infection (UTI), we measured serum procalcitonin levels, a recently described marker of infection. We compared it with other commonly used inflammatory markers and evaluated its ability to predict renal involvement as assessed by dimercaptosuccinic acid (DMSA) scintigraphy. METHODS: Serum C-reactive protein, leukocyte counts, and procalcitonin levels were measured in 80 children, 1 month to 16 years of age, admitted for suspected pyelonephritis. Renal involvement was assessed by 99mTe-DMSA scintigraphy in the first 5 days after admission. The examination was repeated at least 3 months later if the first result was abnormal. RESULTS: In lower UTI, the mean procalcitonin (PCT) was 0.38 micrograms/L +/- 0.19 compared with 5.37 micrograms/L +/- 1.9 in pyelonephritis. In these two groups, respectively, leukocyte counts were 10939/mm3 +/- 834 and 17429/mm3 +/- 994, and C-reactive protein (CRP) levels were 30.3 mg/L +/- 7.6 and 120.8 mg/L +/- 8.9. When inflammatory markers were correlated to the severity of the renal lesion as ranked by DMSA scintigraphy, we found a highly significant correlation with plasma levels of PCT, but borderline significance with CRP and none with leukocyte counts. Patients without vesicoureteral reflux had a mean PCT of 5.16 micrograms/L +/- 2.33, which was not significantly different from that in patients with reflux who had a mean PCT of 5.76 micrograms/L +/- 3.49. For the prediction of renal lesions at admission, CRP had a sensitivity of 100% and a specificity of 26.1%. The sensitivity and specificity of PCT were 70.3% and 82.6%, respectively. CONCLUSION: We conclude that serum PCT levels were increased significantly in children with febrile UTI when renal parenchymal involvement (assessed by DMSA scintigraphy) was present and allowed for prediction of patients at risk of severe renal lesions. Publication Type Journal Article. Research Support, Non-U.S. Gov't. <21> Unique Identifier 9028852 Status MEDLINE Authors Lavocat MP. Granjon D. Allard D. Gay C. Freycon MT. Dubois F. Authors Full Name Lavocat, M P. Granjon, D. Allard, D. Gay, C. Freycon, M T. Dubois, F. Institution Department of Pediatrics, CHU de Saint Etienne, Hopital Nord, F-42055 Saint Etienne Cedex, France. Title Imaging of pyelonephritis. Source Pediatric Radiology. 27(2):159-65, 1997 Feb. Abstract OBJECTIVE: Accurate diagnosis of pyelonephritis using clinical and laboratory parameters is often difficult, especially in children. The main aims of this prospective study were to compare the value of different imaging techniques [renal sonography, cortical scintigraphy with technetium-99m dimercaptosuccinic acid (99mTc DMSA) and computed tomography (CT)] in detecting renal involvement in acute urinary tract infections and to determine the sensitivity of DMSA scans for permanent renal scars 6 months later. MATERIALS AND METHODS: Between February 1992 and January 1993, 55 children admitted to our pediatric unit with febrile symptomatic urinary tract infections were eligible for analysis. Ultrasonography (US), DMSA scanning and micturating cystourethrography were performed in every case. Only 18 children underwent CT. A second DMSA scan was performed in 48 children a mean of 7.5 months after the first. RESULTS: US abnormalities were found in 25 children (45 %). The first DMSA scan showed a parenchymal aspect suggestive of pyelonephritis in 51 patients (93 %). Among the 18 patients studied by CT, 14 had abnormalities. Normal US findings did not rule out renal parenchymal involvement. Scintigraphy appeared to be more sensitive than CT for renal involvement. The frequency and degree of initial renal parenchymal damage seemed to correlate with vesicoureteral reflux, but the most severe initial parenchymal defects were not associated with marked clinical or laboratory manifestations. Repeat DMSA scans, performed on 45 kidneys with abnormalities at the first examination, showed resolution in 19, improvement in 16, persistence in 8 and deterioration in 2. The prevalence of vesicoureteral reflux was not higher in patients with renal scarring on the second DMSA scan than in patients whose scans showed an improvement. CONCLUSION: DMSA scans should be considered as a reference in the detection and follow-up of renal scarring associated with acute urinary tract infection as this technique is more sensitive than US and CT, the latter being unsuitable because it entails radiation exposure and sedation of patients. Publication Type Comparative Study. Journal Article.