Report - Institute of Medical Ethics
advertisement
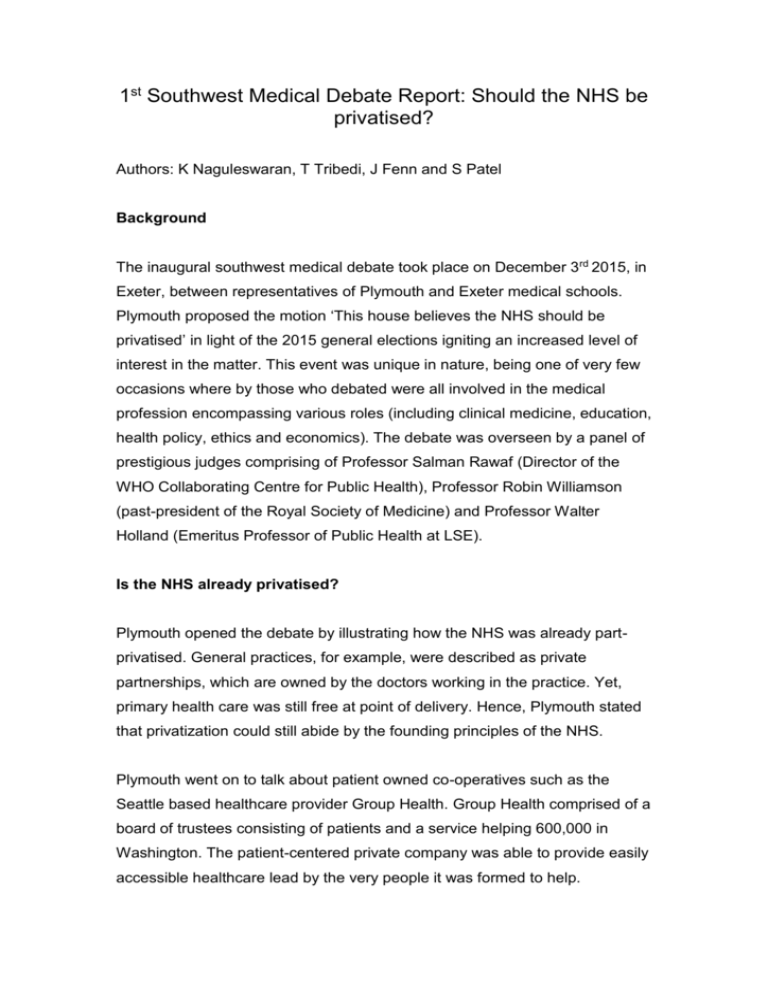
1st Southwest Medical Debate Report: Should the NHS be privatised? Authors: K Naguleswaran, T Tribedi, J Fenn and S Patel Background The inaugural southwest medical debate took place on December 3rd 2015, in Exeter, between representatives of Plymouth and Exeter medical schools. Plymouth proposed the motion ‘This house believes the NHS should be privatised’ in light of the 2015 general elections igniting an increased level of interest in the matter. This event was unique in nature, being one of very few occasions where by those who debated were all involved in the medical profession encompassing various roles (including clinical medicine, education, health policy, ethics and economics). The debate was overseen by a panel of prestigious judges comprising of Professor Salman Rawaf (Director of the WHO Collaborating Centre for Public Health), Professor Robin Williamson (past-president of the Royal Society of Medicine) and Professor Walter Holland (Emeritus Professor of Public Health at LSE). Is the NHS already privatised? Plymouth opened the debate by illustrating how the NHS was already partprivatised. General practices, for example, were described as private partnerships, which are owned by the doctors working in the practice. Yet, primary health care was still free at point of delivery. Hence, Plymouth stated that privatization could still abide by the founding principles of the NHS. Plymouth went on to talk about patient owned co-operatives such as the Seattle based healthcare provider Group Health. Group Health comprised of a board of trustees consisting of patients and a service helping 600,000 in Washington. The patient-centered private company was able to provide easily accessible healthcare lead by the very people it was formed to help. Can healthcare be ethical if financially incentivized? Exeter started by opposing the motion on ethical grounds, codes of conduct, efficiency and accessibility. Privatization would, by its very nature, be financially motivated. How could we base our healthcare system on economically status as opposed to medical need? In addition, Exeter outlined the evidence in a variety of studies showing that making patients pay for healthcare deters the most socio-economically deprived from accessing said care. Hence, by privatizing the NHS, we would betray our evidence-based medical system and ignore evidence in favor of financial incentives. Exeter went on to describe how privatization would result in medical professionals capitalizing on patient’s ill health and suffering. The ethical ramifications of this notion are huge. Could an individual be trusted to perform solely in the patient’s best interest if their pay was dependent on other factors? Evidence in healthcare systems abroad unanimously say no. Does privatatisation make sense economically? Plymouth applied to the economically minded by stating that competition in any market increases the quality of service. They highlighted the effectiveness of such competition using the evolution of the smartphone. Couldn’t such a revolution occur if healthcare was opened up to private providers? They would undercut each other’s prices and the public would stand to benefit. Exeter rebutted this point by clarifying that healthcare and smartphones are incomparable. The variety of smartphones makes for a more successful market. A variety of healthcare providers, Exeter argued, would merely complicate the matter for the patient, making it difficult to make an informed decision. Therefore, this multitude of providers could detrimentally affect healthcare delivery to those in most need. Closing Remarks Plymouth concluded by highlighting, to the medical professional and students in attendance, that the current health service would increasingly lack in resources. In addition, professionals will have less autonomy over their dayto-day practice due to bureaucratic inference and be paid less than European counterparts. Exeter concluded the event by adamantly defending the foundations principles of Aneurin Bevan. They cited partial privatization as the cause of the NHS woes brought up by Plymouth. Therefore, complete privatization would only make the situation worse. Conclusion The judges (a 2-to-1 split decision) and audience swing vote decided that Exeter had made the most convincing arguments. The NHS founding principles along with new evidence from the Commonwealth report (rating the NHS 1st in various aspects of healthcare) was effectively used by Exeter. The audience was not convinced by Plymouth’s argument that privatization could increase the quality of healthcare while remaining easily accessible by all. However, Plymouth was praised for considering aspects of foreign health systems, which worked well and highlighting how the NHS could be improved in various areas such as waiting times. Both teams appealed to ethical considerations. However, Exeter excelled by highlighting the lack of healthcare available (unethically) to millions in the US where a private healthcare system is utilised. ACKNOWLEDGEMENTS Chair: Professor Robert Sneyd (Dean and Professor of Anaesthesia at PUPSMD) Judges: Professor Salman Rawaf (Director of the WHO Collaborating Centre for Public Health) Professor Robin Williamson (past-president of the Royal Society of Medicine) Professor Walter Holland (Emeritus Professor of Public Health at LSE) Debaters: Sir Denis Pereira Gray (Exeter) Professor Brian Kirby (Exeter) Professor Stuart Logan (Exeter) Professor Rod Sheaff (Plymouth) Professor Sheena Asthana (Plymouth) Professor Poorna Gunasekera (Plymouth) (NB: sides were randomly allocated to be for or against the motion) Any finally we would like to thank the Institute of Medical Ethics for sponsoring the event. We subsequently were able to not charge for attendance.