ActionAgenda0803 - Institute For Safe Medication Practices
advertisement

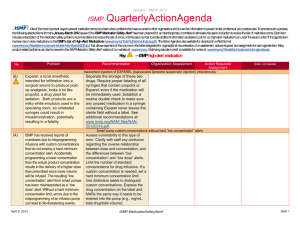
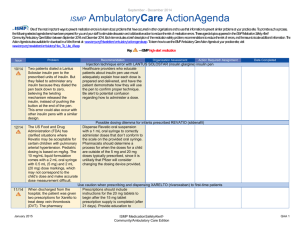
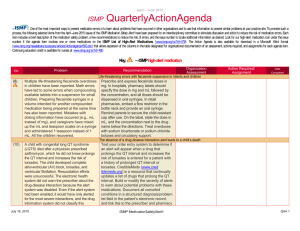
April - June 2008 ISMP QuarterlyActionAgenda One of the most important ways to prevent medication errors is to learn about problems that have occurred in other organizations and use that information to prevent similar problems at your practice site. To promote such a process, the following selected agenda items have been prepared for your senior leaders and an interdisciplinary committee to stimulate discussion and action to reduce the risk of medication errors. These agenda items appeared in the ISMP Medication Safety Alert! between April and June 2008. Each item includes a brief description of the medication safety problem, recommendations to reduce the risk of errors, and the issue number in parentheses to locate additional information as desired. Look for our highalert medication icon under the issue number if the agenda item involves one or more medications on the ISMP List of High-Alert Medications. Many product-related problems can be viewed in the ISMP Medication Safety Alert! section of our website. The Action Agenda is also available for download in a Word format (www.ismp.org/Newsletters/acutecare/articles/ActionAgenda0803.doc) that allows expansion of the columns in the table designated for organizational documentation of an assessment, actions required, and assignments for each agenda item. Continuing education credit is available for nurses at: www.ismp.org/Newsletters/acutecare/actionagendas.asp. Key: Problem No. (7) In 1999, label changes were made to highlight the total amount of drug available in Cerebyx vials after fatalities resulted from confusing the per mL concentration as the total dose in the vial. Despite label changes, FDA has identified seven more fatalities of children who received 10-fold overdoses of Cerebyx. In four cases, the drug was obtained from an automated dispensing cabinet (ADC). In two cases, the per mL concentration (50 mg July 17, 2008 — ISMP high-alert medication Recommendation Organization Action Required/ Assessment Assignment Medication errors associated with CEREBYX (fosphenytoin) Date Completed ADC screens, shelf labels, and printed requisitions should display the total drug content per container instead of the concentration per mL. Ensure all written information is consistent with the manufacturer’s label (100 mg PE/ 2 mL, or 500 mg PE/10 mL). Pediatric facilities should consider stocking only 100 mg PE/2 mL vials of Cerebyx in the emergency department. The need to retrieve many vials in order to prepare a single dose (i.e., ten 2 mL vials would be needed to prepare a 1,000 mg PE dose versus just two 10 mL vials) may serve ISMP MedicationSafetyAlert! QAA 1 April – June 2008 ISMP Problem No. PE/mL) was listed on the ADC screen, not the total drug in the vial (500 mg PE/10 mL). (10 ) (10 ) (12 ) The current situation with heparin products and back-orders means that hospitals may be receiving heparin in quantities, strengths, and packaging that are unfamiliar to staff. The possibility of significant dosing errors increases when unfamiliar products are stocked. A fatal error occurred when a pregnant woman was given a prescription for propylthiouracil, abbreviated as “PTU,” early in her pregnancy but received Purinethol when the prescription was filled. A second patient experienced liver toxicity when a prescription for propylthiouracil, also written as “PTU,” was dispensed as Purinethol. QuarterlyActionAgenda Recommendation Organization Assessment Action Required/ Assignment Date Completed to alert practitioners to a possible dosing error. Recall of heparin leads to use of unfamiliar concentrations Barcode scanning is the best defense against mix-ups arising from unfamiliar products. Use auxiliary labels to call attention to unusual strengths—even circling the concentration on vial labels with a pen. Vials of heparin flush solutions should be separated from vials containing therapeutic concentrations. Mix-ups with propylthiouracil and PURINETHOL (mercaptopurine) The dangerous abbreviation “PTU” should not be used. Physicians should be encouraged to list brand and generic names on orders for Purinethol, and to include the purpose when prescribing either drug. Computer order entry system warnings should be installed for both drugs. Do not store Purinethol and propylthiouracil near each other. Consider placing warning labels on product containers. Caution regarding color-coded eye meds (8) The American Academy of Ophthalmology has long endorsed a voluntary color-code scheme for ophthalmic products based on therapeutic July 17, 2008 Color-coding ophthalmic products according to therapeutic class does not decrease medication mix-ups in hospitals, as it might in a patient’s home. To prevent ISMP MedicationSafetyAlert! QAA 2 April – June 2008 QuarterlyActionAgenda Problem No. class. But the color schemes are too similar to differentiate between classes of eye medications, and numerous product mixups, both between and within each class, have been reported. ISMP Recommendation Organization Assessment Action Required/ Assignment Date Completed look-alike problems, pharmacy purchasers should avoid awarding contracts to one vendor for an entire product line and should consider purchasing drugs within a class from different manufacturers. Strength misread as total dose on mannitol IV bags (B. Braun) (8) The labeling on 250 mL bags of IV mannitol 20% states, “Each 100 mL contains: Mannitol USP 20 g in Water for Injection USP.” A physician prescribed three bags for a patient, believing each one delivered just 20 g. Each 250 mL bag actually contains 50 g. Consider affixing alert stickers to mannitol to inform staff about the total amount of drug in each bag. Review other medication labels for potential errors, and affix warning stickers or other visual cues to communicate the total content of medication in each container. Safety issues with insulin pens used in hospitals (9) Errors arising from the adoption of insulin pen devices in healthcare organizations are emerging: needlestick injuries to healthcare workers; sharing pens among different patients; withdrawing medication from pens, which results in air pockets that can interfere with dosing accuracy; inadvertent product mix-ups; and erroneous dosing due to July 17, 2008 Although insulin pens offer many advantages over insulin vials, safe use requires anticipating and reducing potential risks before implementation and close monitoring during the first few months of implementation when unanticipated failures and workarounds are most likely to occur. Conducting a failure mode and effects analysis before use, limiting the variety of pens in use, educating staff before use, and establishing ISMP MedicationSafetyAlert! QAA 3 April – June 2008 ISMP Problem No. improper drug administration techniques. QuarterlyActionAgenda Recommendation Organization Assessment Action Required/ Assignment Date Completed written guidelines for reference are important risk reduction strategies. Avoid confusion with TORISEL (temsirolimus) dose preparation (9) Torisel injection is distributed in a kit that contains a vial of active drug along with a vial of diluent. Following dilution, the pre-printed strength on the vial is no longer accurate. A 20% overfill (that is not explicitly stated on the label) adds complexity and increases the potential for dosing errors. (9) Inadvertently storing one insulin product inside of the external carton of another type of insulin can lead to serious wrong-drug errors. (9) Sumatriptan 25 mg tablets were placed into a matrix drawer intended for sitagliptin 25 mg tablets in an automated dispensing cabinet (ADC). Both medications are manufactured in 25, 50, and 100 mg tablets, and the generic names are similar when read July 17, 2008 Pharmacists should keep the package insert, with full instructions for dilution, with both the active drug and diluent vials. Use pharmacy computer alerts during order entry and/or warning stickers on packaging to notify staff about the change in concentration when preparing the final dilution. For more information, visit: www.ismp.org/sc?k=pbm. Remove insulin vials from cartons External cartons for insulin products should be discarded prior to dispensing the vials or at the time of receipt on the nursing unit. Sumatriptan (IMITREX) confused with sitagliptin (JANUVIA) Be alert for potential mixups with this look-alike, sound-alike pair. Use of a bar-coding system when replenishing ADC stock diminishes the risk of inadvertent drug mix-ups. Add a redundancy to manual checking processes by having stocking personnel match both the generic and brand ISMP MedicationSafetyAlert! QAA 4 April – June 2008 QuarterlyActionAgenda Problem No. and pronounced. (10 ) Hospitals may not manage the process by which pharmaceutical products, devices, and related education are brought into their organizations to maximize safety. Unexpected pharmaceutical products (including samples) and changes in drug storage have given rise to serious, preventable errors. ISMP Recommendation Organization Assessment Action Required/ Assignment Date Completed names (if available) when refilling matrix drawers. Managing visits from pharmaceutical sales representatives If you allow onsite visits by pharmaceutical representatives, require them to schedule visits with the pharmacy, wear an identification badge, sign an agreement to abide by hospital rules—including no sample distribution, and be escorted to their destination. For details, visit: www.ismp.org/Newsletters/acu tecare/articles/20080522.asp . Red rules in healthcare (10 ) (12 ) In highly reliable industries, “red rules” are limited to just a few rules that must always be followed to prevent serious harm to employees, customers, or the product line. In healthcare, red rules should not be confused with policies or standard operating procedures—even crucial ones like handwashing that call for strict adherence. While compliance with policies and procedures is always expected, there will July 17, 2008 Red rules should be limited to a few, well understood and memorable rules that are possible and desirable for everyone to follow under all circumstances. Anyone who notices that a red rule has been breached should have the authority to stop the process. Examples of red rules in healthcare might include a time out before an invasive procedure and reconciliation of a sponge count before closing a surgical incision. Following the “5 rights” of medication use and full compliance with barcode scanning technology ISMP MedicationSafetyAlert! QAA 5 April – June 2008 QuarterlyActionAgenda Problem No. (11 ) (11 ) ISMP Recommendation Organization Assessment Action Required/ Assignment Date Completed inevitably be are not appropriate red circumstances when rules in healthcare, as both practitioners cannot rules are often broken for abide by the rules, or reasons rooted in inadequate circumstances where system support for following violating a rule may be the rule. the best course of action. Restricted character space and truncated drug listings are a set-up for medication errors Truncated information Review how drug information appeared on a medication appears on MARs and pharmacy administration record labels. If problems are (MAR) as “NOVOLOG found, work with the FLEXPEN 70” rather than pharmacy computer system “NOVOLOG FLEXPEN 70/30.” vendor to prevent truncated This led a nurse to data from appearing on MARs administer 70 units of and labels. Including “Mix” NOVOLOG (insulin aspart) with NOVO-LOG MIX 70/30 instead of NOVOLOG 70/30 (which is the actual brand (insulin aspart name) can help differentiate protamine, insulin the drug from NovoLog. aspart). Identify home medications A patient filled The original medication prescriptions for error was a causative factor ISENTRESS (raltegravir) in the need for inpatient 400 mg, one tablet BID, care, and his condition and PREZISTA (darunavir) continued to worsen until 300 mg, two tablets the error was discovered and twice daily. The labels rectified. Pharmacists must on the prescription identify—very early on—any bottles were reversed, medication brought from home so he took incorrect by patients, especially if doses for a month. He it’s necessary to use the was admitted to the patient’s home medication hospital where the error supply until the hospital persisted because his pharmacy can obtain the home medications were drug(s). administered according to the misplaced labels. July 17, 2008 ISMP MedicationSafetyAlert! QAA 6 April – June 2008 ISMP Problem No. (12 ) (12 ) QuarterlyActionAgenda Recommendation Organization Assessment Action Required/ Assignment Date Completed Prevent dangerous drug-device interaction causing falsely elevated glucose levels When patients receive Hospitals should consider EXTRANEAL (icodextrin) using only POC blood glucose peritoneal dialysis meters that rely on glucose solution, blood glucose oxidase, glucose hexokinase, values obtained using glucose dehydrogenase some point-of-care (POC) nicotinamide adenine glucose meters may be dinucleotide (GDH-NAD), or falsely elevated. Deaths flavin adenine dinucleotide have been reported due glucose dehydrogenase (FADto severe hypoglycemia GDH), which are accurate after prescribing even in the presence of insulin based on the interfering products falsely elevated glucose including maltose. If other levels. MaltosePOC meters are used, screen containing IV patients for interfering immunoglobulin (IVIG) products and, if they are products may cause prescribed, obtain glucose similar falsely elevated levels using hospital glucose values with laboratory methods only. glucose meters. Look-alike glass bottles of sodium chloride and nitroglycerin Sodium chloride 0.9% Evaluate and correct storage injection was practices that can lead to administered instead of errors. Determine if at-risk IV nitroglycerin when behaviors (such as “grab and similarly appearing go” when selecting products) glass bottles were are occurring on busy units. stored beside one Practice habits—such as another in a busy ED. meticulous reading of labels and consistent use of barcode technology—should be operational norms that are periodically monitored. July 17, 2008 ISMP MedicationSafetyAlert! QAA 7