ISMP Medication Safety Alert - Institute For Safe Medication Practices
advertisement

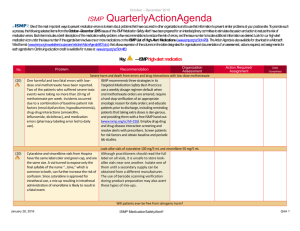
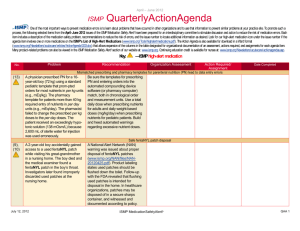
January – March 2012 ISMP QuarterlyActionAgenda Oneof the most important ways toprevent medication errors is to learn about problems that have occurred in other organizations and to use that information toprevent similar problems at your practice site. Topromote such aprocess, thefollowing selected items fromtheJanuary-March 2012 issues of theISMP Medication Safety Alert! have been prepared for an interdisciplinary committee tostimulate discussion and action to reducethe risk of medication errors. Each item includes a description of themedication safety problem, recommendations toreducethe risk of errors, and theissue number to locate additional information as desired. Look for our high-alert medication icon under the issuenumber if theagendaitem involves oneor more medications on theISMP’s List of High-Alert Medications (www.ismp.org/Tools/highalertmedications.pdf). TheAction Agenda is alsoavailablefor download in a Word format (www.ismp.org/Newsletters/acutecare/articles/ActionAgenda1202.doc) that allows expansion of the columns in thetable designated for organizational documentation of an assessment, actions required, and assignments for each agenda item. Many product-related problems can also beviewed in the ISMPMedication Safety Alert! section of our websiteat: www.ismp.org. Continuing education credit is available for nurses at: www.ismp.org/Newsletters/acutecare/actionagendas.asp. Key: Problem No. (6) Exparel, a local anesthetic intended for infiltration into a surgical wound to produce postop analgesia, looks a lot like propofol, a drug used for sedation. Both products are a milky white emulsion used in the operating room, so unlabeled syringes could result in misadministration, potentially resulting in a fatality. (4) ISMP has received reports of overdoses due to misprogramming infusions with custom concentrations that do not employ a hard minimum concentration alert. Accidentally programming a lower concentration than the actual product concentration results in the delivery of a higher dose than prescribed since more volume will be infused. The resulting “low concentration” alert from smart pumps has been misinterpreted as a “low dose” alert. Without a hard minimum concentration limit, errors due to the misprogramming of an infusion pump can lead to life-threatening events. April 5, 2012 Recommendation —ISMP high-alert medication Organization Assessment Action Required/ Assignment Inadvertent injection of EXPAREL (bupivacaine liposome suspension injection) intravenously Date Completed Separate the storage of these two drugs. Require proper labeling of all syringes that contain propofol or Exparel, even if the medication will be immediately used. Establish a routine double check to make sure any unused medication in a syringe containing Exparel never leaves the sterile field without a label. See additional recommendations at: www.ismp.org/NAN/ files/NAN20120318.pdf. Smart pump custom concentrations without hard “low concentration” alerts Assess vulnerability to this type of error. Clarify with staff any confusion regarding the inverse relationship between dose and concentration, and the differences between “low concentration” and “low dose” alerts. Limit the number of standard concentrations for drug infusions. If a custom concentration is needed, set a hard minimum concentration limit. Use distinctive labels to distinguish custom concentrations. Express the drug concentration on the label and MARs the same way it needs to be entered into the pump (e.g., mg/mL, total drug/total volume). ISMP MedicationSafetyAlert! QAA 1 January – March 2012 ISMP Problem No. (1) An order for “eribulin” (eribulin mesylate, HALAVEN) was misinterpreted by a pharmacist and entered into the computer as epirubicin. Both drugs are associated with breast cancer treatment, but typical dosing is very different and should have prompted a call to the prescriber for verification. (1) QuarterWatch™ analysis of adverse events reported to FDA showed a large number (505) of hemorrhagic events with dabigatran, more than any other drug including warfarin (176). Events involved mostly elderly patients. Patients with mild renal failure had dabigatran blood levels 50% higher than patients with normal renal function, although prescribing information suggests dosage adjustment only for severe renal impairment. (1) According to a recent study (www.nejm.org/doi/ full/10.1056/NEJMsa1103053?qu ery=featured_home), warfarin, insulin, oral antiplatelet agents, and oral hypoglycemics accounted for more than twothirds of the drugs tied to hospitalization for adverse drug events in older adults. Most events were associated with unintentional overdoses. April 5, 2012 QuarterlyActionAgenda Recommendation Organization Assessment Action Required/ Assignment Date Completed Chemotherapy mix-up between eribulin mesylate and epirubicin Add the salt “mesylate” to the eribulin listing in computer systems, and apply tall man lettering (eriBULin mesylate, EPIrubicin) to prevent name mix-ups. A pharmacist should verify and independently recalculate the dose of any antineoplastic agent before dispensing it. Any questions should result in a direct query to the prescriber. Adverse events with dabigatran during quarter 1 of 2011 Alert prescribers to reports of hemorrhagic events and dosing issues associated with elderly patients with renal impairment. The drug’s manufacturer reported it is working with FDA to provide better guidance to physicians on treating elderly patients, especially those with transient (e.g., contrast media use) or chronic impaired renal function. Medications associated with adverse events that led to hospitalization Provide specific medication errorprevention education to hospitalized patients who are discharged on warfarin, insulin, oral antiplatelet agents, and oral hypoglycemic agents. Pay particular attention to the prevention of dosing errors. ISMP MedicationSafetyAlert! QAA 2 January – March 2012 ISMP Problem No. (4) At least three fatalities have been reported in Europe due to inadvertent administration of IV bortezomib into the intrathecal space. These events involved intrathecal chemotherapy scheduled on the same day/time as the IV bortezomib. Intrathecal chemotherapy and IV bortezomib are both administered in small volumes via syringes, increasing the likelihood of a mix-up. (1) Repeated events suggest widespread misunderstanding that sterility can be maintained between patients by affixing a fresh needle on a pen device. Studies have shown that biological contamination occurs in up to half of all reused insulin pens. This concern led the CDC to issue a clinical reminder (www.cdc.gov/injectionsafety/ clinical-reminders/insulinpens.html) regarding increasing reports of improper use of insulin pens. (5) Inadvertent tubing misconnections are frequent and preventable errors that pose a significant risk to patient safety and can result in devastating outcomes. Because of human factors, the clinical environment, and the interconnectivity of Luer connectors, healthcare April 5, 2012 QuarterlyActionAgenda Recommendation Organization Assessment Action Required/ Assignment Date Completed Bortezomib deaths due to intrathecal misadministration Administer intrathecal chemotherapy at a different time than IV chemotherapy. Verify that intrathecal medication has been administered before dispensing IV bortezomib (or vice versa) for patients receiving medications via both routes. Label bortezomib syringes with warnings about IV use only. Require a time-out procedure and an independent check before administering intrathecal medication or chemotherapy. Do not use an insulin pen for multiple patients To reduce the risk of cross contamination, insulin pens should be assigned to individual patients and labeled using a “flag” attached to the body of the pen without covering the drug name. If ongoing education and monitoring of proper use of pen devices cannot be accomplished, hazardous conditions may persist, and hospitals may need to consider whether patients would be safer by dispensing vials or prefilled syringes of insulin. Tubing Misconnections Self Assessment for Healthcare Facilities Hospitals are encouraged to complete a new self assessment tool (www.baxter.com/healthcare_ professionals/clinical_center_of_exc ellence/connections_portfolio/progr ams/tubing_misconnection_index.ht ml) that guides users to evaluate current delivery systems and mating devices. By completing the ISMP MedicationSafetyAlert! QAA 3 January – March 2012 ISMP Problem No. professionals have mistakenly connected the wrong devices and delivered substances via the wrong route. (2) The use of multidose vials in the operating room (OR) has resulted in infection outbreaks and errors. Cross contamination is always a possibility when using multidose vials. Also, when medications are supplied in quantities that exceed the amount typically given, practitioners may misinterpret the amount in the vial as a single dose, leading to overdoses. (3) ISMP continues to identify instances in hospitals where resuscitation carts have outdated versions of the Broselow tape, which is used to identify doses of medications for children based on body length. (4) Studies show that Cosmegen diluted at concentrations of 10 mcg/mL or higher in sterile water, normal saline, and 5% dextrose are stable for 10 hours (room temperature). But dilution with April 5, 2012 QuarterlyActionAgenda Recommendation Organization Assessment Action Required/ Assignment Date Completed assessment, hospitals will identify potential tubing misconnection risks and develop an action plan to mitigate risks through processes, device selection, and education. Avoid multidose vials in the operating room The Association of periOperative Registered Nurses (AORN) recently released a set of recommended practices (http://alturl.com/xapaa) that include a recommendation to collaborate with pharmacists to procure and store only single-dose vials in the OR and post-anesthesia unit. Multi-dose vials should be avoided. The document outlines other best practices in the OR when procuring, prescribing, dispensing, administering, and monitoring the effects of medications. New Broselow tape available Ensure that the newly available, most up-to-date Broselow tape (dated 2011 Edition A) is available on resuscitation carts as appropriate (www.arm strongmedical.com/index.cfm/go/pr oduct.detail/sec/3/ssec/14/fam/2371 ). The tape has revised zones based on new national data on length-weight relationships in children, making these tapes more accurate. Do not infuse COSMEGEN (DACTINomycin) in sterile water Dilute Cosmegen only in 5% dextrose or normal saline during preparation for IV administration. ISMP MedicationSafetyAlert! QAA 4 January – March 2012 ISMP Problem No. QuarterlyActionAgenda Recommendation Organization Assessment Action Required/ Assignment Date Completed sterile water could result in a hypotonic solution that would cause hemolysis if administered IV. (3) An order for Rapaflo 8 mg daily was transcribed incorrectly as Rapamune. Due to a bug in a software upgrade (since corrected), some of the medications in the database would not appear on the screen if the full drug name was entered. This reinforced an at-risk behavior of only typing in the first few characters of a drug name, which in this case (R-A-P) called up the wrong drug. (5) FDA discovered an unlicensed supplier selling fake bevacizumab injectables (under the brand name AVASTIN) to oncology practices. The fake product contained no active ingredient. (6) Vials of calcium gluconate and cupric sulfate were mixed up when preparing infusions. Both vials are similar in size and have a similar pink color on the label, although one is from American Regent (cupric sulfate) and the April 5, 2012 Mix-ups between RAPAFLO (silodosin) and RAPAMUNE (sirolimus) Hospitals should add this drug name pair to their list of look-alike drug names. Prescribers can help prevent mix-ups by including the drug’s purpose when ordering medications and regularly reviewing the patient’s medication list. The full drug name should be used whenever feasible instead of the first few characters when entering orders into the pharmacy computer. Prevent counterfeit drugs from reaching patients All healthcare professionals, not just pharmacists, need to be aware of proper procedures for safely procuring medications for patients. The Partnership for Safe Medicines provides resources for pharmacists, nurses, and physicians to help prevent counterfeit medicines from reaching patients (http://safedr.ug/ for_pharmacists, http://safedr.ug/for_nurses, http://safedr.ug/for_physicians). Look-alike vials of calcium gluconate (100 mg/mL) and cupric sulfate (4 mg/10 mL) Separate storage of these products in the pharmacy. If possible, purchase one of the products from a different manufacturer. ISMP MedicationSafetyAlert! QAA 5 January – March 2012 ISMP Problem No. QuarterlyActionAgenda Recommendation Organization Assessment Action Required/ Assignment Date Completed other from APP (calcium gluconate). (6) Sharing eye drop containers between patients and between both eyes of one patient has led to serious eye infections due to cross contamination. While most products include preservatives to prevent growth of bacteria and fungi, organisms can still thrive on the tip of the bottle. Rates of contamination as high as 35% have been noted in some studies; although infections are rare, they can happen and even cause blindness in some cases. April 5, 2012 Eye drop-related infections To reduce costs, ophthalmicspecialty hospitals often have mandatory training, competency, and monitoring programs to teach and validate safe eye drop administration. Hospitals without this level of training and monitoring should dispense separate containers of eye drops for each patient and each eye. Once discharged, patients can use a device (e.g., Owen Mumford) that does not allow the bottle to touch the eye when squeezing out the drops. ISMP MedicationSafetyAlert! QAA 6