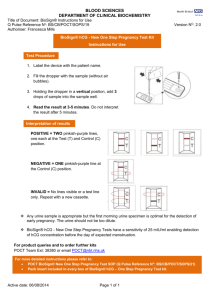
point of care testing (poct) procedure
advertisement

POINT OF CARE TESTING (POCT) GUIDELINES These Guidelines underpin section 3.14: POCT in the Medical Devices Policy 533576959 Created on 30/06/2008 15:39:00 Page 1 of 19 Review: 26/03/2010 1. INTRODUCTION/PURPOSE OF THE GUIDELINES 1.1 Definition of Point of Care testing 1.1.1 Point of care Testing (POCT) is defined as any analytical test performed for a patient by a healthcare professional outside the conventional Pathology laboratory setting and is a valuable procedure used in patient care. Examples of POCT include: o Blood glucose monitoring o Blood gas/ co-oximetry analysis o Electrolyte analysis o Blood coagulation measurement o Blood HbA1c analysis o Urine analysis o Rapid tests for infectious disease markers o Pregnancy testing 1.1.2 POCT is now an established part of clinical practice. However it is important that it is viewed as part of an integrated activity in which the objective is caring for the patient in the best clinical and most cost-effective way. The main strengths and weaknesses of POCT are summarised as follows: Strengths Improved turnaround time allowing Weaknesses Duplication of testing and equipment rapid therapeutic intervention Cost-per-test invariably greater than equivalent informed counselling for therapeutic laboratory tests management Incompatibility with laboratory results leading to Smaller sample volumes reducing iatrogenic clinical confusion blood loss Tests performed by staff with a non-analytical Economic benefits associated with reduced background – leads to increased risk of length of stay in hospital adverse incidents Possibility for reduced sample transport costs. May encourage inappropriate testing These strengths and weaknesses must be carefully considered when addressing whether POCT should be implemented and in reviewing situations in which POCT has grown in an unregulated and uncontrolled manner. 533576959 Created on 30/06/2008 15:39:00 Page 2 of 19 Review: 26/03/2010 1.2 GUIDELINES FOR POCT 1.2.1 In 1999, the Joint Working Group on Quality Assurance (JWG) published guidelines highlighting that POCT is a Clinical Governance issue and emphasising the central role that Pathology must have in the implementation and management of POCT. 1.2.2 The MDA Device Bulletin (2002), Management and Use of IVD Point of Care Test Devices are consistent with and based on the JWG Guidelines. It provides definitive guidance on all issues relevant to implementation and management of POCT. 1.2.3 These above guidelines are used as standards for POCT by Clinical Pathology Accreditation UK Ltd that is an independent body that assesses the standard of Pathology services, including POCT. 1.2.4 The European In Vitro Diagnostic Medical Devices Directive 18 regulates most of the equipment used for POCT. The Directive, which came fully into force on 7th December 2003, aims to ensure that; devices will not compromise the health and safety of patients and users; devices are designed and manufactured to achieve the performance specified by the manufacturer for the stated medical purpose. Devices that meet the relevant essential requirements of the Directive will carry a CE mark to denote compliance. 1.3 Aim of the Guidelines 1.3.1There is a requirement to ensure that all POCT equipment used within the Trust: o Is suitable for its intended purpose o Meets safety and quality assurance standards o Can be supported adequately o Is operated only by appropriately trained staff 1.3.2 This requirement can only be met by Trust-wide Guidelines on POCT based on the JWG and MDA guidelines which will ensure consistent procedures are in place throughout the Trust. These Guidelines will facilitate adherence to the principles of Clinical Governance by defining responsibility and procedures for: o Training, certification and proficiency testing of POCT operators o Standardisation of equipment where practical thereby facilitating use, training and maintenance o Effective risk management o Compliance with Health and Safety legislation and infection control measures 533576959 Created on 30/06/2008 15:39:00 Page 3 of 19 Review: 26/03/2010 1.3.3 If not used appropriately there is a risk that patients may be put at risk from inappropriate testing or wrong results. Therefore for the successful use of POCT devices it is essential that the purchase, implementation and quality assurance assessment be carried out appropriately. 1.3.4 The appropriate use of these tests should be considered as a Clinical Governance issue and subject to examination of clinical effectiveness. 1.3.5 To achieve the best possible results from POCT devices it is essential that there is the closest possible liaison with the Pathology services relating to all aspects of such tests. To ensure reliable performance and manage the risks associated with point of care testing, the Pathology laboratory must have a central role in management of these devices. o On-going quality control, quality assurance and auditing of POCT o Negotiation of cost effective bulk discounts with suppliers of equipment and consumables o Networked IT support to facilitate audit trails and faster troubleshooting. 2. APPLICATION: TO WHOM THESE GUIDELINES APPLY These guidelines apply to all those working in the Trust, in whatever capacity. A failure to follow the requirements of this procedure may result in investigation and management action being as considered appropriate. This may include formal action in line with the Trust’s disciplinary or capability procedures for Trust employees; and other action in relation to other workers, which may result in the termination of an assignment, placement, secondment or honorary agreement. 3. SUMMARY OF THE GUIDELINES These guidelines are set out to ensure complete quality assurance with regards to all issues surrounding Point of Care Testing. Roles and responsibilities are set out and lines of accountability are clearly defined. 4. THE GUIDELINES 4.1 Trust POCT Committee 4.1.1 The Trust POCT Committee is a sub committee of the Medical Devices Committee and will oversee POCT across the Trust to ensure that POCT is appropriate and accreditable. It is chaired by the Consultant Chemical Pathologist with responsibility for POCT and has a wide membership to ensure all relevant expertise is incorporated, as follows: o Trust POCT Co-ordinators 533576959 Created on 30/06/2008 15:39:00 Page 4 of 19 Review: 26/03/2010 o Trust Risk Management o Pathology Laboratory Management o Diabetes Nurse Specialists o Medical Representatives (Consultant Physician) Nursing Representatives (Medicine and Critical Care) o Pharmacy/Supplies Representative o Medical Engineering and Maintenance 4.1.2 The Committee will co-opt additional members where appropriate as the practice of POCT expands e.g. Primary Care Representative 4.1.3 The Committee will co-opt representatives from additional fields on a temporary basis to ensure that there can be an informed discussion on agenda items. This will particularly apply to Infection Control and Medical Audit representatives. 4.1.4 The Committee shall ensure that POCT Devices are implemented and used appropriately. The POCT committee will report to the Medical Devices Group, which itself reports to the Clinical Governance committee. These report to the Trust Board. 4.1.5 The MDA Notices and the Joint Working Group on Quality Assurance emphasise the central role that Pathology has in ensuring that POCT Devices are used appropriately. This subcommittee reflects that recommendation. 4.1.6 No POCT Devices should be used within the Trust unless approval has been obtained from the POCT Committee. 4.1.6 The POCT committee will have responsibility for: o considering the case for introduction of POCT in a particular location prior to procurement. o determining budgetary responsibility for individual POCT services. o ensuring compatibility between instrumentation (POCT and laboratory) in use Trust-wide. o establishing the presence of a link nurse at ward level. o ratifying Standard Operating Procedures (SOPs), Service Level Agreements (SLAs), Risk Assessments and COSHH assessments. o ascertaining the complexity of a device and therefore grades of staff that would be authorised to use that device following training. o internal quality control material and participation in external quality assessment scheme 533576959 Created on 30/06/2008 15:39:00 Page 5 of 19 Review: 26/03/2010 o accreditation scheme compliance e.g. CPA (UK) Ltd o consumables o record keeping e.g. data handling system o cleaning and waste disposal 4.2 Cost Benefit Analysis and Procurement. 4.2.1 All POCT devices are subject to the criteria described in this document irrespective of whether the equipment has been purchased (including from endowment funds), hired, loaned or received as a donation 4.2.2 Proposals to introduce POCT must be supported by a Cost Benefit Analysis, which includes a clear definition of the problem that a POCT device would solve so that a full examination of all possible solutions can be made. 4.2.3 The Pathology Department will, in conjunction with the requesting clinical department, be responsible for the production of the Cost Benefit Analysis, which will be presented to the POCT committee for evaluation and approval before submission to the Trust for financial support. 4.2.4The Cost Benefit Analysis must detail all the financial consequences to Pathology and the proposed POCT site. These will include capital and revenue costs associated with the equipment itself and all staffing resources required by both the laboratory and the clinical area to provide the service. These costs can be further broken down as follows: o initial purchase of equipment and accessories. o provision of a safe environment e.g. health and safety improvements o site alterations to accommodate POCT o interfacing with information management systems o staff time (clinical and laboratory) required for patient analysis, support, training, quality assurance and audit. o routine and preventative maintenance e.g. external service contracts with manufacturers o internal quality control material and participation in external quality assessment scheme o accreditation scheme compliance e.g. CPA (UK) Ltd o consumables o record keeping e.g. data handling system o cleaning and waste disposal 4.2.5 The Cost Benefit Analysis must recognise the need for any device to be compatible with existing equipment, both in the laboratory and in other areas of the hospital. The Pathology Department will address issues of compatibility and be responsible for producing a shortlist of potential suppliers. 533576959 Created on 30/06/2008 15:39:00 Page 6 of 19 Review: 26/03/2010 4.2.6 The Pathology laboratory will evaluate the technical quality of the equipment and any interfacing requirements. Short-listed suppliers will be invited to submit their equipment for demonstration and/or trial. 4.2.7 When funding has been identified, an operational specification will be drawn up jointly by Pathology and the clinical users and companies will be invited to tender. The final selection will be made by a panel composed of representatives from Pathology and the clinical unit and will be ratified by the POCT committee. o ensuring that all users are trained and certified in the use of POCT devices. o ensuring that internal quality control (IQC) and external quality assessment (EQA) schemes are employed effectively. o ensuring that all POCT services within the Trust are assessed for CPA Accreditation in conjunction with the relevant Pathology Department, o monitoring and recording all adverse incidents involving POCT devices. 4.3 Risk management 4.3.1 It is essential that training and support from the Pathology departments and the POCT Committee properly manage the risks associated with the use and interpretation of results obtained. No POCT devices are totally fail-safe. 4.3.2 In accordance with current guidelines, POCT devices with network connectivity are the preferred option. Instruments that can be connected directly to the Point of Care Connectivity system allow transfer of data directly to the laboratory computer, ensuring accountability and a complete audit trail. It is for this reason if a connectivity version is available this is what must be purchased. 4.3.3 The Cost Benefit Analysis must recognise the need for any device to be compatible with existing equipment, both in the laboratory and in other areas of the hospital. The Pathology Department will address issues of compatibility and be responsible for producing a shortlist of potential suppliers. The Pathology laboratory will evaluate the technical quality of the equipment and any interfacing requirements. Short-listed suppliers will be invited to submit their equipment for demonstration and/or trial. 4.3.4 When funding has been identified, an operational specification will be drawn up jointly by Pathology and the clinical users and companies will be invited to tender. The final selection will be made by a panel composed of representatives from Pathology and the clinical unit and will be ratified by the POCT committee. 4.3.5 Lines of accountability should be clearly written into local policies and procedures. (see appendix A) 4.4 Health & Safety 4.4.1 Managers of the Clinical service involved together with the Pathology service must jointly develop and enforce policies consistent with current legislation and Guidance. For example: the Health & Safety at Work 533576959 Created on 30/06/2008 15:39:00 Page 7 of 19 Review: 26/03/2010 Act 1974, Consumer Protection Act 1987, the Control of Substances Hazardous to Health (COSHH) Regulations 1988, Safe Working and the Prevention of Infection in Clinical Laboratories – Model Role for Staff and Visitors, HSC 1981, Protection against Blood-born infections in the workplace: HIV and hepatitis (ACDP) 1995. 4.4.2 There should be close liaison between the Safety Officers responsible for the testing site and Pathology. 4.4.3 A Decontamination certificate (see Trust Policy), providing evidence of appropriate decontamination, must be issued before servicing or repair of equipment. 4.4.4 The Infection Control Physician/Medical Microbiologist must be involved in decisions on placement and maintenance of equipment. 4.4.5 The manufacturer prior to installation must provide a Master Indemnity Agreement. 4.5 Budgetary Management and Stock Control 4.5.1 The designated budget holder for each particular POCT service will be ultimately responsible for managing the budget. 4.5.2 The clinical department will, jointly with Pathology, agree necessary measures to resolve budgetary problems. 4.5.3 The clinical department will ensure that there is a rotation system in operation and that all reagents are within their shelf life. 4.6 Maintenance 4.6.1 It is mandatory that all POCT devices must be regularly maintained. The POCT Co-ordinator will be responsible for overseeing the maintenance of all such devices and the POCT Co-ordinator will be responsible for training designated operators as necessary. Responsibility of the ward and the laboratory for carrying out maintenance procedures will be outlined in the SOP for each device. 4.6.2 The manufacturers’ engineers according to the company service schedule will perform Service visits. The POCT Co-ordinator will determine responsibility and procedures for liasing with the manufacturer regarding all equipment problems and failures. 4.6.3 Each device must have a “Device Record Book” or logbook in paper or electronic form in which maintenance records, faults, corrective actions and repairs by named individuals are documented. These records are the management responsibility of the Pathology laboratory and must be accessible for inspection at all times. 533576959 Created on 30/06/2008 15:39:00 Page 8 of 19 Review: 26/03/2010 4.7 POCT Operators and Training 4.7.1 Only staff whose training and competence has been established and documented will be authorised to use any POCT device. 4.7.2 The training course must be specified and supervised by the relevant Pathology department and provided by the manufacturer or local staff trained to the satisfaction of the relevant Pathology department. 4.7.3 The training course must include:o patient preparation o sample collection o sample suitability and stability o sample analysis o quality assurance procedures o interpretation of results o recording results o limitations and contraindications o health and safety issues and liability issues. 4.7.4 Once competence has been achieved and documented, the user can be added to the "Named Operator List" and a password to gain access to the device issued if appropriate. 4.7.5 POCT Operator ID barcodes and passwords must NEVER be shared or given out to any other member of staff. POCT Operators must only use their own POCT barcode and password. 4.7.6 Additional training, as specified and supervised by the relevant Pathology department, will be provided for designated staff responsible for maintenance. 4.7.7 All trained staff must undergo proficiency assessments and refresher/update training as specified in the SOP in order to retain their operator status. 4.7.8 The Pathology department will provide input into the development and delivery of appropriate Continuing Professional Development (CPD) programmes. 533576959 Created on 30/06/2008 15:39:00 Page 9 of 19 Review: 26/03/2010 4.7.9 Responsibilities of POCT operators and those of the POCT Co-ordinator are listed in Appendix C. 4.8 Standard Operating Procedures (SOPs). 4.8.1 All POCT devices must have SOPs that are available to and followed by all operators of the device with no deviations. 4.8.2 All devices must have an SOP which includes information on:o sample suitability and stability o quality assurance procedures o performing the analyses o method of recording results o interpretation of results o reference ranges o limitations and contraindications o health and safety issues. o action required in case of suspected device failure or an unexpected result. 4.8.3 All SOPs must be written to the standard required by Clinical Pathology Accreditation. A master copy of the SOP must be held by Pathology and be available to Assessors from Clinical Pathology Accreditation, or equivalent accreditation agencies. 4.8.4 Additional supporting documents must be stored with the SOP including COSHH and Risk Assessments, Manufacturers Operator Manuals, relevant MDA notices, Named Operator Lists. Duplicate copies of these documents will be stored in Pathology. 4.9 Quality Assurance and Audit 4.9.1 Quality assurance is a mandatory component of POCT and includes all the measures taken to ensure that investigations are reliable – test selection, obtaining a satisfactory specimen, analysing it and recording the results promptly, interpreting the result accurately, taking appropriate action, and documenting all procedures for reference. 533576959 Created on 30/06/2008 15:39:00 Page 10 of 19 Review: 26/03/2010 4.9.2 There are two components to quality assurance: internal quality control (IQC) and external quality assessment (EQA). The Pathology laboratory is responsible for ensuring that they are applied to the same rigorous standard as in the laboratory setting, such as would satisfy CPA inspection criteria. 4.9.3 Internal Quality Control is a means of checking that results are reliable before they are issued. Results obtained must be recorded appropriately (electronically or on paper), compared with acceptance limits and the appropriate action taken as defined in the SOP. 4.9.4 EQA involves the analysis of samples with unknown value from an external source. These samples will be issued and administered by the Pathology laboratory. EQA samples must be analysed by a user of the instrument as if they were normal patient samples. It is the responsibility of the ward manager to allow time for users to perform EQA analysis. Results should be recorded and returned to the laboratory. 4.9.5 The Pathology department is responsible for evaluation of QC and QA data, liasing with clinical users regarding performance and determining appropriate action in the event of unsatisfactory performance. 4.9.6 The Pathology department must carry out regular audits of the reliability and effectiveness of the tests being carried out. 4.10 Recording of Results 4.10.1 All patient and Quality Control/Quality Assessment (QC/QA) results must be recorded. This record must include unequivocal patient identity, time of test, the result, relevant QC results and the identity of the user. 4.10.2 Management of these records is the responsibility of the POCT Co-ordinator who must have free access to all data. 4.10.3 A more permanent record of documentation in the patient’s notes must replace temporary reports issued by POCT devices. This should take the form of a laboratory report (paper or electronic) in the case of devices with connectivity. 4.10.4 All patients’ results must be treated as confidential and kept in a secure place. If patient results are stored in a computer system, local rules on access to the system, whether stand-alone or networked, should be maintained. 4.11 Support 4.11.1 There must be a Service Level Agreement defining the level of support for the device with respect to stock control, maintenance, troubleshooting, repairs, continuing training and QA monitoring. 533576959 Created on 30/06/2008 15:39:00 Page 11 of 19 Review: 26/03/2010 4.11.2 A device that fails or is suspected of failing to perform to specification must be withdrawn immediately from service and Pathology informed. If devices are not used or cared for appropriately the Pathology department will have the authority to remove the device from service. If multiple use of an individual’s password is suspected that password will be withdrawn from use and the individual’s supervisor informed. 4.12 POCT Analysers Specific POCT analysers and their respective procedures (SOP’s, Training, QC procedures) are listed on the Point of Care Testing Microsite on the Trust’s Intranet. A summary of these specific procedures are listed in Appendix B. 533576959 Created on 30/06/2008 15:39:00 Page 12 of 19 Review: 26/03/2010 Flow chart for the Implementation of New and Replacement Point of Care Testing Devices Idea to Stage 1: Ask the POCT Co-ordinator for advice introduce a new POCT service or replace a POCT device Preliminary discussions with POCT Co-ordinator, Pathology Dept and Clinical Lead Produce Proposal document POCT Chair may act to initiate urgent approval Stage 2: Submit Proposal Document to POCT Committee Recommendation to obtain further supporting information or agreement not to proceed Recommendation to proceed Involvement of supplies for procurement of suitable POCT analyser Laboratory evaluations Operator evaluations Advice from IT, Infection Control, Risk Management POCT Co-ordinator organises collection of information on devices Secure capital and consumable costs for project Clinical Area and Laboratory work together to prepare Cost Benefit Analysis & Business Plan for preferred option(s) Identify POCT Link Nurse and staffing implications for Clinical Area and Laboratory support. Review relevant literature Stage 3: POCT Committee considers procurement of named device Rejected or deferred A letter outlining the reasons will be issued Approved Clinical Area make changes to ward fabric e.g. IT links, reagent storage POCT Co-ordinator arranges Training protocols, SOPS, COSHH, SLA, EQA and IQC, record keeping, maintenance logs etc Stage 4: Approval Process POCT Committee approves SOPs, SLAs, training & EQA Referred for amendments A letter detailing the specific reasons will be issued Approved POCT service goes live On-going audit of POCT impact on patient care On-going audit of quality of testing Stage 5: POCT Committee Review Process 533576959 Created on 30/06/2008 15:39:00 Page 13 of 19 Review: 26/03/2010 The diagram illustrates all the possible stages involved in the POCT implementation and audit process. In practice some of the implementation stages will merge although which stages will depend on the POCT device and service. 533576959 Created on 30/06/2008 15:39:00 Page 14 of 19 Review: 26/03/2010 Appendix A 1. Issue 2. Process Co-ordination 3. Action by 4. Responsible for action 5. Evaluated by Cost benefit analysis (business case) POCT Committee Trust Management Trust Management Risk Management POCT Committee Trust Management Trust Management Health & Safety POCT Committee Trust Management Trust Management Budgetary arrangements POCT Committee Purchasing Advisory Group and POCT committee Trust Risk Management Group Trust Risk Management Group Pharmacy Trust Management POCT committee Maintenance POCT Committee Trust Management Training (including record of trained staff) POCT Committee Trust Management POCT Committee Pathology Trust Management Standard Operating Procedures POCT Committee Trust Management CPA (UK) Ltd. Routine Operation POCT Committee POCT Coordinator POCT coordinator Training Dept. Key Trainers Pathology and POCT Committee Users POCT committee/audit Recording Results POCT Committee Users Line Manager (e.g. Ward Sister through Link Nurse) Line Manager Support POCT Committee POCT coordinator Trust Management Trust Management Quality Control & EQA- internal - external POCT Committee Users POCT coordinator Trust Management POCT committee Pathology 533576959 Created on 30/06/2008 15:39:00 Page 15 of 19 Review: 26/03/2010 POCT committee/audit Appendix B Blood Glucose Meters Roche Advantage III glucose meter. 1. Standard Operating Procedure 2. Training Competency Form 3. Procedure for External and Internal Quality Control Testing Blood Gas Analysers Roche Cobas b221 blood gas analyser 1. Standard Operating Procedures. 2. Training Competency Forms 3. Procedure for External and Internal Quality Control Testing. Hemocue Hb Analyser 1. Standard Operating Procedure 2. Training Competency Form 3. Procedure for External and Internal Quality Control Testing. Oximcom 3000 Oxygen Saturation Analyser 1. Standard Operating Procedure 2. Training Competency Form 3. Procedure for External and Internal Quality Control Testing. ACT Plus Analyser 1. Standard Operating Procedure 2. Training Competency Form 3. Procedure for External and Internal Quality Control Testing. Urine Pregnancy Testing Emergency Department 1. Standard Operating Procedure 2. Procedure for External Quality Control testing 533576959 Created on 30/06/2008 15:39:00 Page 17 of 19 Review: 26/03/2010 Appendix C Responsibilities of Users of POCT devices No staff member must use any POCT equipment unless they are certified to do so. No staff member may train another in the use of POCT equipment unless they are authorised to do so. All staff members must use the equipment in a safe and responsible manner. All staff members must have a unique identifier (password) where applicable. No password must be shared with another staff member. An accurate and up to date maintenance log must be maintained, signed and dated each day. All staff members must satisfy the quality control (QC) requirements pertaining to the specific instrument. All patient and QC results must be documented. Included with the results should be the operator's initials and the date and time of the test. All staff members operating POCT equipment will have up to date competency records. In the event of an instrument failure, staff members will immediately notify the POCT Coordinator or if out of hours, the laboratory (extension 4048). Responsibilities of Point of Care Co-ordinator Works within the constraints of the Pathology laboratory service. Is responsible for ensuring that all POCT is performed to the same standard as would be expected from regular laboratory testing. Identifies the types and locations of all POCT equipment within SHH. An electronic record of all equipment is maintained. Is responsible for ensuring that all of the SHH staff performing POCT, has current competency training and documentation. Included is an awareness of health and safety issues pertaining to samples and equipment. Is responsible for ensuring regular Quality Assurance (QA) is maintained and Quality Control (QC) samples are analysed on POCT devices, with up-to-date documentation and history. Is responsible for ensuring that adequate supplies of consumables and QC materials are maintained, to ensure continuity of service. Is responsible for troubleshooting of all POCT devices, with up-to-date documentation and history. Discussion All SHH staff members who perform a Point of Care Test must assume responsibility for the result(s) they generate. In effect, for the duration of the test, they become a surrogate laboratory scientist, governed by the same rules and strictures as laboratory workers. The SHH POCT Guidelines must be complied with. Noncompliance may result in a disciplinary hearing. Therefore it is in both the hospital's and the laboratory's interests to promote awareness of POCT: quality assurance and quality control, analyser maintenance, ongoing training and competency testing are all matters pertaining to POCT, which by definition involves both hospital and laboratory Quality Implementation (QI) practices. The SHH POCT Guidelines are available as a reference for QI. POCT issues such as competency documents, audit trails, quality assurance and maintenance records may be investigated by accreditation authorities during forthcoming certification process. Erroneous results If a patient was adversely affected by an incorrect POCT result, an investigation into the circumstances surrounding the incident would occur. Procedures already well established within SHH would be used. POCT is no different in this respect to any other enquiry that would be undertaken in similar circumstances. Remember: Never share your ID or password with other staff members. Always sign and date any printouts or transcription of results 533576959 Created on 30/06/2008 15:39:00 Page 18 of 19 Review: 26/03/2010 If a new staff member commences work, ensure they have the necessary POCT training from the POCT Coordinator or a credited staff member. Don't train new staff members yourself. Make sure your competencies are up to date. References Medical Devices Agency Device Bulletin: Management and Use of IVD Point of Care Test Devices; MDA DB2002(03); March 2002. Joint Working Group on Quality Assurance Point of Care Testing Guidelines: ACB News: May 1999; 433; 1623 Point of Care Testing: Ed Christopher Price and Jocelyn Hicks, Pub AACC Press, 1999. Clinical Governance: Implications for point of care testing: D B Freedman, Ann Clin Biochem, Vol 139, No5, Sept 2002, 421-423 Guidelines for implementation of point of care testing: International Federation of Clinical Chemistry (IFCC) 1999 (on line) CPA New Standards: Clinical Pathology Accreditation (UK) Ltd. Can be downloaded from the CPA website www.cpa-uk.co.uk NCCLS Communications Standards: Connectivity Industry Consortium (CIC). Can be downloaded from the CIC website www.poccic.org 533576959 Created on 30/06/2008 15:39:00 Page 19 of 19 Review: 26/03/2010