Patient Safety - Frontiers in Laboratory Medicine
advertisement

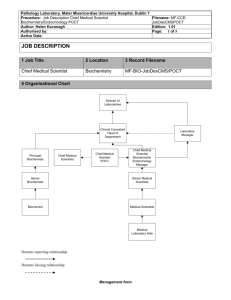
Creating value and improving patient safety – the role of the Lab Professional Dr Danielle B Freedman FiLM Feb 2011 Q1 • What do users want from a lab service – • Top10 aspects What do users really want? Role of Laboratory interface • Value of interpretative service • ‘Demand management’ inappropriate testing/non testing Patient • ‘24 hour cover’ Safety Effective use of POCT The Problems • Too many tests • Different names • Different units • Different reference intervals • Different alert limits • Inconsistent guidelines • • • • • • • What do our users want from Laboratory Medicine? Information to allow clinicians to make better decisions about patients Patient safety Clinical governance, accountability, accreditation Demand management. Investigations need to becheap, quick and correct. “New” tests Right investigation on the right patient at the right time Result needs to get to the right clinician at the right time using the right medium Right interpretation and right patient outcome What interests Practice Based Commissioners • • • • • • Care Closer to Home eg Warfarin monitoring Care pathways and pathology tests eg eGFR and Primary Care management of chronic kidney disease Collection of specimens and electronic reporting of results Need to establish clinical dialogue with laboratories Development of Point of Care Testing Patient safety J Crockett CEO, Wolverhampton City PCT 2008 • Consolidation • Diagnostics “nearer the home” • Diagnostics provided by ‘others’ ? Fragmentation of service Primary Care Clinical Advice Questionnaire S Beds 2009 Q. Did Clinical Advice on Interpretation aid in patient management? 2%2% Yes Unsure No 110 respondents 96% Comments: ‘Particularly useful in obtaining advice when testing for endocrine disorders’ ‘A1 Service’ ‘GP provider link is excellent’ ‘Knowing there is someone to ask can save inappropriate investigations & unnecessary referral’s’ ‘Dr Freedman very helpful & always return calls promptly’ Are endocrine comments useful to GPs? IM Barlow Ann Clin Biochem 2008; 45: 88–90 TFT comments affecting patient management 100 91 90 80 73 Percentage 70 60 50 40 30 20 10 0 GP Nurse Practitioner Percentage feeling comments (very) frequently helping/influencing patient management IM Barlow Ann Clin Biochem 2009; 46: 85–86 Objective evidence of the benefit of interpretative comments Provision of interpretative comments to GPs has led to: • 22% reduction in inadequate thyroxine replacement in samples from hypothyroid patients • ~500 more patients adequately treated after introducing comments Kilpatrick Ann Clin Biochem.2004:41:225-7 Getting the most from your Pathology Lab’ National Association of Primary Care Review April 2009 Housley D & Freedman DB. ‘ “Emphasis on laboratory role on interpretation … computer generated comments according to predetermined rules; comments on reports or by dialogue at bedside or by phone …” e.g. PRL Reflex testing - Macroprolactin Comment Avoids • Outpatient referral • MRI • Patient experience of an incorrect pathological diagnosis Survey of East of England GP Commissioning Groups Please score the issues below, indicating their importance to you and your practice All patient results electronically available to GPs through single access point regardless of requestor within cluster Important or Very Important (%) 100 Reduction in unit cost of tests 90 Specialist support for GPs from pathologists within cluster for pre-analytical and post-analytical phases 80 Monthly utilisation and cost data at GP level to analyse usage and inform commissioning decisions 90 Support the implementation and maintenance of POCT systems in primary care 80 Survey of East of England GP Commissioning Groups Please score the issues below, indicating their importance to you and your practice Important or Very Important (%) Accessible and convenient sampling centres which include support for extended GP working and out-of-hours 70 Guaranteed sample collection times throughout the day, maintaining ample integrity 100 Guaranteed raid and consistent turnaround times, within 2448 hours in most cases 90 Electronic ordering systems linked to sampling centres and laboratories 80 Conclusion • • • • • • • Pathology and laboratory services need to become more ‘dynamic’ and responsive to needs of patients, 1° care clinicians and commissions Community pathology services should receive higher profile in commissioning and need dialogue PBC, PCTs and pathologists Improve access to phlebotomy Test ordering – education and training and feedback or behaviour, clinical guidelines Accreditation – governance infrastructure POCT Patient Safety Q2 • What points in TTP have highest incidence of errors ? Patient Safety and Pathology Pre Analytical right test right patient right label ‘request form’ right sample Analytical EQA Accrediation (CPA) Post Analytical right lab right conditions temperature right result right patient right clinican right communication right interpretation right Mx and further investigations “patients who are acutely ill are often cared for by most junior medical staff who have least knowledge and experience” BMA News, 2 June 2007 (letter) T-bone stake “…It reminded me of the occasion when a FY2 rang while I was on call to inform me that he had seen a patient with a broken forearm – but did not know the anatomical name for the bone. At a guess it started with the letter “T”, he said. I dashed to the patient’s side to clarify that the patient had actually injured what I was envisaging and was in no danger. The FY2 had never sat a formal anatomy exam, nor had he undergone formal dissection/pro-section lessons at medical school…” “How confident are you in requesting laboratory tests?” LFT U&E Proteins Mg, PO4 Confident Usually Confident Not Confident Haematinics PTH Short Synacthen Test Urine sodium and osmolality 0% 20% 40% 60% 80% 100% “How confident are you on interpreting laboratory tests?” LFT U&E Proteins Mg, PO4 Confident Usually Confident Not Confident Haematinics PTH Short Synacthen Test Urine sodium and osmolality 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% Labs Are Vital™ Media Monitoring and Successful Results What points in the process have the highest incidence of errors? Bar coding? Specimen collection? Specimen Analysis? Results reporting? NO Laposata 2008 What points in the process have the highest incidence of errors? Test selection by clinicians? Interpretation of test results by clinicians? YES Laposata,2008 Types and relative frequency of errors in the different phases of the TTP Phase of the TTP Pre-pre-analytic Post-postanalytic Relative Frequency (%) 46 – 68.2 25 45.5 Plebani M Ann Clin Biochem 2010, 47: 101110 Post-post analytical errors: frequency of incorrect interpretation of diagnostic tests in different clinical settings Setting Primary Internal care Emergency medicine department Incorrect interpretation of diagnostic tests: estimate (%) 37 38 37 Plebani M , Ann Clin Biochem 2010 : 47 101110 Safe care measures “avoiding injuries to patients from the care that is intended to help them” AUS CAN GER NL NZ UK US Overall rank 6 5 2 1 4 2 7 Medication errors 13% 10% 7% 6% 13% 9% 14% Incorrect lab test result 7% 5% 5% 1% 3% 3% 7% Delay in notification of abnormal results 13% 12% 5% 5% 10% 8% 16% Commonwealth Fund, 2010 “No point in requesting a test if no-one looks at the results and/or acts on the result…” Kilpatrick and Holding BMJ 01 Delay ward Accident and emergency department (n=3228) Acute Medical admissions (n=1836) Within 1 hour (22)% 794 (25)% 412 1-3 hours (19)% 491 (15)% 341 Over 3 hours (30)% 500 (15)% 553 Never (29)% 1443 (45)% 529 Of 1443 A & E results – 43 (3%) could have led to an immediate change in management Audit of Emergency Department at the Luton & Dunstable Hospital: Results reported and reviewed for a 24 hour period Results not reviewed within one hour 50% [of which 89% were outside reference interval] Not within 2 hours 26% Not within 3 hours 14% Not at all 10% 17 Feb 2010 Disconnect between Lab Alerts & Follow Up Singh et al. Am J Med 2010: 123:238-244 Out Patient results May – Dec 2008 Hb Aic ≥ 15% positive hepatitis C antibody PSA ≥ 15 ng / ml TSH ≥ 15 MU / l 10.2% of alerts unacknowledged ‘Multidisciplinary interventions involving human – computer interaction and highly reliable tracking systems to monitor test result notification outcomes are needed to alleviate patient safety concerns’ Frequency of failure to inform patient of clinically significant outpatient test results Failure to inform outpatients of significant abnormal test results 1 in 14 tests e.g. Cholesterol = 8.3mmol/ L Potassium 2.6 mmol / L = Casalino et al Arch Int Med: 2009 169.11239 Critical Value Reporting ISO EN15189 :2007 … “ immediate notification of a critical value is a special requisite” CPA (UK) Ltd … “ critical value reporting is essential to ensure Quality of diagnostic laboratory services” Joint Commission NPSG 2010 ... “report critical results on a timely basis” A Way Forward: Critical Value Reporting Need for consensus critical values list Surveys for comparing and improving existing policies regarding critical values should be promoted at an INTERNATIONAL LEVEL Piva, Sciacovelli, Plebani & Laposata Clin Chem Lab Med 2010: 48:461-8 Q3 • Top 10 Quality Indicators, in general terms “What is Quality in Pathology” 12/13th Oct 2010 • www.rcpath.org/resources/pdf/rcpath_quality_meeting_draft_13.pdf • RCPath response to Ian Barnes letter “Reconfiguration of NHS Pathology Services “ July 2010 Q4 • Egs of Pre and Post analytical input has made a difference to patient outcome • ( excluding cell path/morphology/antibiotic sensitivity) Role of Laboratory Interface Clinical Vignette 48 year old male GP routine bloods Grossly lipaemic – triglyceride = 130 mmol/l (<1.9) DBF D/W GP – known alcoholic ? Risk of pancreatitis (from etoh and trigs) Commence ciprofibrate 100 mg od Cease etoh Suggest referral ASAP to hepatologist Avoidance of acute admission and potential morbidity Clinical Vignette 56 year old Chinese male (poor historian) Previous A&E attendance with 1/52 headache – given some medicine Since then generally unwell – sweating, ? Weight loss GP requested TFT – fT4 = 6 pmol/l, TSH = 1.23 mU/l TSH inappropriate for fT4 – lab add other Ix Sodium = 128 mmol/l Other U&E NAD Cortisol (08:30am) = 108 nmol/l Testosterone = 2.9 nmol/L Prolactin 167 mU/l LH = 1.9 U/l, FSH = 2.8U/l Hydrocortisone cover advised, followed by replacement of other axes – Urgent Chemical Pathology OPD arranged with GP. Infarcted pituitary adenoma confirmed. Avoidance of acute admission and potential morbidity. Clinical Vignette • • • • Patient presents to GP with bruising and nose bleeds Platelet count <20 Consultant haematologist speaks to GP to start Prednisolone immediately at 7pm on Friday - prevent inpatient admission and potential morbidity Microbiologist authorising reports 2 children with MRSA from swabs collected for ?otitis externa Both patients from same surgery seen 2 hours apart Discussion with GP revealed insufficient attention to cleaning ear pieces and issues around hand hygiene “Before ordering a test, decide what you will do if it is either positive or negative, and if both answers are the same, then don’t do the test!” Reference ranges Factors influencing the result Interpretation Further investigations ‘Delivery’ of results Clinical Vignette 28 year old male GP requests routine investigations at 6pm Friday night, processed in lab at 7pm: Sodium = 116 mmol/l (136 – 148) Potassium = 1.9 mmol/l (3.8 – 5.0) Urea <0.3 mmol/l Creatinine = 81 mol/l Only clinical details available ‘alcoholic’ ? Beer potomania Emergency admission arranged by DBF via GP 45 year old female Cholesterol 8.2mmol/L despite being on Simvastatin 40mg GP phoned Clinical Biochemistry Comment: • Exclude secondary causes of hypercholesterolaemia • Liver tests demonstrated ALP = 350 IU/L [25 – 120] • Prior to starting Statin ALP = 340 IU/L • Further investigations: Antimitochondrial antibodies , U/S Liver, Liver biopsy Diagnosis: Primary biliary cirrhosis Cost to Purchasers? Cost to patient? Value to the whole health economy? Cost to the health economy Outpatients: New : £200 F/U £100 : Admission Acute: £1150 + Market forces 16% Luton 30% + London HDU : £1000/ day + Market forces ITU £2000 / day + Market forces : Q5 • IT supporting the clinical role of the lab For use in Consultant led hepatology or gastroenterology clinics only. Requests from other sources will be reviewed and may be rejected. Multi-disciplinary investigation strategies agreed between users and diagnostic departments save clinician time and reduce variation. Ordering by clinical condition with defined options for primary care reduce inappropriate tests and reduce variation in practice. Tests linked to diagnostic algorithms at time of order promote appropriate investigations, ensure adequate investigation and improve compliance with care pathways. Electronic orders linked to patient information resources and evidenced based testing websites David I have never seen this written on a GAGS report before what is the reason they have written it here .This was an odd baby who behaved in a slightly encephalopathic way and got cooled when newborn .He has a persistently slightly abnormal ALT and is mildly anemic .Otherwise now asymptomatic when Sabine saw him yesterday Sarah Email linked to reports offers an additional way for clinicians to seek clinical advice from the laboratory. Lab advice automatically enters medical record. Clinical letters linked into lab system enable clinical scientists / pathologists to have extensive clinical / drug information available to improve reporting DOES A TICK BOX CULTURE EXIST ? TEST Gamma-GT Phos Mg 2007 3217 12857 13775 2008 3429 14745 15185 2009 4056 17463 17302 2010 4461 20199 19112 2011 2427 16907 15867 2009 2010 ICE introduced Tick boxes removed Laboratory automatically generate emails within reporting system to alert people to key results • – numerous examples, but these include: • All BNP > 200 pg/ml mailed to community heart failure nurses who then organise rapid diagnostic echo – reduces time to definitive diagnosis. • All children less than 10yrs with a TSH > 10 IU/ml alerted to paediatric endocrinologist – improves drug compliance. • All positive troponins mailed to cardiac team / rehab nurses – ensures all inpatients obtain cardiology review. System DOES NOT replace traditional alerting of critical results, but acts as a supplement to improve outcome and care. Q6 • Benefits of formal accreditation process of Pathology Views on CPA by hospital pathology users – Luton and Dunstable Hospital 2009 Improved pathology service delivery 90 80 Benefited patients 70 60 Benefited users 50 Improved the pathology services 40 reputation 30 20 Ensured that pathology 10 Results are safe and reliable 0 Improved service delivery Benefits patients Benefits users Improves lab reputation Improves DOH should safe + Regulate for reliability CPA compliance DOH should consider Regulatory requirement for Compliance with CPA standards. Effective use of Point of Care Testing (POCT) Hospital ‘Chemists’ Surgicentres Home Polyclinics ‘other’ eg internet, van GPs Paramedical vehicle World-wide PoCT Market 2001 US $2.8 billion Outside US $2.6 billion World-wide $5.4 billion 2005 $5.5 billion $10.3billion 2011 - $18.7 billion global, $7.5 billion US Applications of POCT The Evidence – Clinical and/or cost effectiveness* Some examples Infection eg CRP* Helicobacter Pylori? Chlamydia? Urine leukocyte* Chronic Disease Management DM Hyperlipidaemia Anticoagulation Hypertension CHD Acute U + E* Gases* Troponin* HbA1C* Cholesterol* INR* Albumin:cr? BNP* Cost benefits of POCT anticoagulation management in Primary Care P Johnson City + Hackney PCT (2008) Net savings as result of transferring 460 patients from 2° to enhanced service in GP practices > £150,000 pa but O’Connor, (J Clin Path Feb 2008) In Shropshire error rate for 1 practice 164 times higher than hospital [INR>8] Implementation of POCT POCT is presented as “Easy to use and capable of producing accurate results ....” but Problems (RISK MANAGEMENT) when procedures for training and quality assurance are poor • • • Incorrect results can affect the well-being of a patient Health hazards eg HIV and hepatitis viruses to both patient and operator Implementation MUST follow National Guidance Case History Miss DM, 28 year old March ‘mild glycosuria’ GP performed GTT: Time 0 mins 30 mins 60 mins 90 mins 120 mins Glucose (mmol/l) - glucometer 8.4 18.6 22.0 15.2 12.3 Rx: Glibenclamide Revisited GP - symptoms of hypoglycaemia Glibebclamide stopped September referred to Diabetic clinic GTT (laboratory) Time 0 mins 60 mins 120 mins Glucose (mmol/l) 5.3 5.3 6.1 Glucometer - faulty No QC In US • > 3200 incidents including 24 deaths and 986 injuries have been filed with FDA re blood glucose monitoring Successful POCT Joint endeavor • • • Manufacturers Many different professional groups Patients … failure of professionals to indicate to top management the clinical risk involved (Burnett Ann Clin Biochem 2000) Regulation of POCT • • • • • • • UK: no legal framework but MHRA 2010 Belgium, Finland: legal framework Netherlands: mandatory guidelines that regulate laboratory testing, including POCT Germany: legal framework for analytical quality control Italy: regional but not national guidelines France: legal regulation of public laboratories but not private labs (from report of Roundtable meeting, Abbott 2005) USA: POCT is regulated by CLIA federal law (Thanks to Dr J Pearson, Leeds) View from Mr Gordon Cropper, Chair of Lay Advisory Committee RC Pathologists (2007) “…the members of lay committee would rather have the correct/right result and wait a couple of days, than have a ? wrong result immediately…” National Guidance • ISO 15189 and ISO 22870 • National Guidance issued in 2002 • Clinical Pathology Accreditation (UK) Ltd PoCT standards in 2010 • MHRA 2010 Q8 • In 3 years time do you think the value of Lab testing will be : • • • • a) more important than today ? b) less important ? c) the same And WHY ?