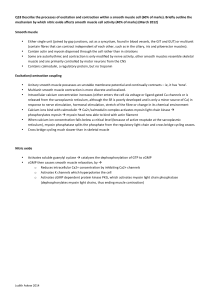
VIII. Cardiac muscle
advertisement

Title: Muscles Teacher: Magdalena Gibas MD PhD Coll. Anatomicum, 6 Święcicki Street, Dept. of Physiology Muscles I. The structural and functional organization of muscles A. Functions of muscles include: movement, stability, communication (facilitate speech, writing), control of body openings and passages, and heat production. B. Skeletal muscle Skeletal muscle is voluntary striated muscle usually attached to bone. It exhibits striations, reflecting the overlapping nature of the internal contractile proteins. I band consists of thin filaments only, A band contains thick and thin filaments, M line is composed of myosin tails (thick filaments), Sarcomere, which is a functional unit, is located between two Z lines (Z line – site of fixation of thin filaments). Cyclic “rowing” of thick filaments over thin shortens Iband, H zone, but A band is constant. The series-elastic components of muscular tissue include the stretched endomysium, perimysium, epimysium, fascia, and tendon, all of which are not excitable but do stretch and recoil. II. Functional structure of skeletal muscle cell A. The muscle fiber (muscle cell) 1. Myofilaments Myofilaments are central to muscle contraction. Three kinds exist: thick filaments, thin filaments, and elastic filaments. 2. Sarcomere Sarcomere is the unit of contraction of a muscle fiber. 3.Sarcoplasmic reticulum (SR) Sarcoplasmic reticulum is a reservoir for calcium ions, it joins with T tubules to form terminal cisternae III. The nerve-muscle relationship A. Motor neurons 1. Skeletal muscle is innervated by somatic motor neurons whose cell bodies are in the brainstem and spinal cord. The axons of motor neurons are called somatic motor fibers. Each muscle fiber (of skeletal muscle) is supplied by only one motor neuron. B. The motor unit A motor unit consists of one nerve fiber and all the muscle fibers it innervates. It behaves as a single functional unit and contracts as one. Multiple motor units within a muscle are able to "work in shifts." C. The neuromuscular junction 1. A nervous impulse traveling down the neuron triggers the release of neurotransmitter (acetylcholine - ACh) from synaptic vesicles into synaptic cleft. ACh binds to receptors, which are present in the motor end plate (part of sarcolemma = membrane of muscle fiber). This is the signal for depolarization of motor end plate. An enzyme called Acetylcholinesterase breaks down Ach after its diffusion from Ach receptor. IV. Behavior of skeletal muscle fibers A. Resting potential of cell membrane (sarcolemma) is negative, about - 80 to - 90mV. B. Excitation-contraction coupling During excitation-contraction coupling, action potentials in the muscle fiber lead to activation of the myofilaments. The wave of action potential (AP) reaches the T tubules and continues into terminal cisternae of SR. AP affect dihydropyridine receptors (DHPR) in the T tubules. It activates ryanodine receptors on SR and opens calcium channels of SR (ryanodine receptors work as a calcium channels). Calcium ions are released then into the cytosol. Calcium ions bind to the troponin of the thin myofilaments, causing the troponintropomyosin complex to shift aside, exposing the active sites on the actin filament. The heads of the myosin filaments (called crossbridges) can now bind to these active sites and initiate contraction. B. Contraction During the contraction phase, sliding of the thin myofilaments across the thick ones causes the muscle fiber to shorten. The sliding filament theory of Hanson and Huxley suggests that thin filaments slide over thick ones, causing sarcomeres to shorten. The head of each myosin molecule contains myosin ATPase that releases energy from ATP. In preparation for action, the myosin binds and hydrolyzes an ATP molecule, and is now in the "cocked" position. When the active sites on the actin filament are exposed, the myosin head contacts the active site, releases energy, and performs a power stroke (movement). At the end of a power stroke, myosin binds to a new ATP, releases the actin, and returns to its original position in a recovery state. The cycle of power stroke and recovery is repeated many times during muscle contraction. C. Relaxation When nervous stimulation ceases, the muscle relaxes. Acetylcholinesterase breaks down ACh so the muscle stops generating its action potentials. Calcium is carried back to the sarcoplasmic reticulum by active transport (it requires ATP break down). D. The length -tension relationship and tonus 1. The degree of actin and myosin overlap determines tension development by contracting muscle. If the muscle is already contracted, stimulation will cause a weak contraction. Conversely, if the muscle is overstretched, little overlap exists between actin and myosin filaments, and contraction can damage the muscle. V. Behavior of whole skeletal muscles A. Threshold, latent period, twitch 1. Muscle have a threshold or minimal voltage, necessary to produce a muscle contraction. 2. If a muscle is given a single, brief stimulation, it will show a quick cycle of contraction and relaxation called a twitch. 3. A very brief latent period exists between two successive twitches in which the muscle cannot contract. B. Contraction strength of twitches 1. The strength of contraction of a whole muscle is increased as more motor units are activated. 2. Another way to produce a stronger muscle contraction is to stimulate the muscle at a higher frequency. 3. Muscle cells exhibit treppe, or the “staircase phenomenon”, in response to a series of stimuli of the same strength. This is probably due to the inability of the muscle cells to fully return calcium to the sarcoplasmic reticulum during a shot period between stimulations. 4. After a twitch, a short refractory period exists during which the muscle cannot respond to another stimulus. 5. If a second stimulation arrives before the end of the refractory period, the muscle will achieve temporal summation (or wave summation) and achieve a higher level of tension. 6. If the stimuli are frequent enough that the muscle cannot relax completely in between, a state of incomplete tetanus is reached. If there is no time to relax at all between stimuli, complete tetanus is achieved. C. Isometric and isotonic contraction 1. Isometric contraction is tensing of the muscles without a change in length. If two ends of a muscle are fixed such that it cannot shorten, and the muscle is stimulated to contract, tension develops in the muscle, but the length of a muscle does not change. 2. Isotonic contraction is contraction with a change in muscle length but no change in tension. VI. Skeletal muscle metabolism A. ATP sources 1. During exercise, muscles use energy produced by aerobic respiration (when there is an adequate supply of oxygen) and anaerobic fermentation (when oxygen is limited, and lactic acid accumulates). 2. For immediate energy, muscle tissue relies on the phosphagen system to supply ATP. 3. For short-term energy, after the phosphagen system is exhausted, muscles reply temporarily on the glycogen-lactic acid system for ATP 4. For long-term energy, the respiratory and cardiovascular systems catch up and deliver enough oxygen to meet the demands of aerobic respiration. B. Slow- and fast-twitch fibers 1. Slow-twitch fibers (red) – aerobic metabolism (using oxygen; fatigue resistent). 2. Fast-twitch fibers (white) – anaerobic metabolism (no oxygen; low endurance) 3. Although both slow and fast fibers are present in most muscles of the body, one or the other usually predominates. VII. Smooth muscle 1. Smooth muscle is composed of spindle – shaped myocytes, they contain only one nucleus, and no visible striations or sarcomeres. 2. There are no Z lines in smooth muscle, but its thin filaments attach to so called dense bodies. Smooth muscles lack T tubules of cellular membrane. 3. Calcium enters through channels in the sarcolemma. 4. Most calcium for smooth muscle contraction comes from the extracellular fluid, not the sarcoplasmic reticulum, and it binds to calmodulin, not to troponin. 5. The two functional categories of smooth muscle are multiunit and single-unit. 6. Partly because of its latch-bridge mechanism, smooth muscle can remain partially contracted for a prolonged period without additional nervous stimulation. This ability, plus its fatigue-resistance, enables smooth muscle to maintain smooth muscle tone. 7. The ability of an organ such as the stomach or urinary bladder to expand results partly from the stress-relaxation response of smooth muscle. VIII. Cardiac muscle A. Composition. 1. Single nucleus; fibers are smaller than in skeletal muscle. 2. T tubule – larger than in skeletal muscle and is located at the Z line rather than at the junction of A and I bands. B. Excitation - contraction coupling 1. Ca2+ induced Ca2+ release. Ca2+ release from SR is triggered by Ca2+, not by membrane depolarization!!! a. The T tbubule DHP receptor in cardiac muscle, unlike the DHPR in skeletal muscle, contains Ca2+ channel (or works as a Ca2+ channel), through which Ca2+ enters the cell during the action potential. See appropriate picture from the book. b. The SR RYR (ryanodine receptor) is opened by the influx of Ca2+ from the T tubule. Now compare it with skeletal muscle! See appropriate picture (book). 2. The amount of Ca2+ release is under physiologic control: a. The amount of Ca2+ entering the cell and within SR may be increased by catecholamines b. the amount of intracellular Ca2+ is regulated by the Na+-Ca2+ exchanger, an antiport mechanism driven by the Na+ gradient that transports one Ca2+ out of the cell for every 3 Na+ molecules that enter 3. Great amount of Ca2+ for heart contraction comes from T tubules, thus concentration in ECF (extracellular fluid) greatly influences strength of contraction C. Shortening and force development 1. Summation and tetanus are not possible (Cardiac cells have long AP and long twitches and do not show temporal summation) 2. The sarcomere length before contraction (the preload) depends on how much blood has entered the heart. 3. The force of contraction can vary at a given sarcomere length if the amount of Ca2+ entering the cell is changed. This is under physiologic control and, thus, is an important regulator of cardiac muscle contractile force. IX. Comparison of cardiac, skeletal, and smooth muscle Muscle type Role of Ca2+ Source of Ca2+ Mechanism of Ca2+ mobilization Regulation of force Skeletal Initiates contraction by binding to troponin Intracellular from SR. Enough Ca2+ is released to activate all muscle protein Depolarization of T-tubule Summation, recruitment, and preload are varied to vary force Cardiac Initiates contraction by binding to troponin Intracellular from SR. Extracellular through DHP receptor (L type) Ca2+ channels. Amount of Ca2+ released can be varied to vary contractile force. Ca2+-induced Ca2+ release Contractility and preload are varied to vary force; variations in contractility affect speed of contraction. Smooth Activates calmodulin, which in turn activates MLCK Intracellular from SR. Extracellular through voltage- and receptoractivated Ca2+ channels. IP3 increases release of Ca2+ ; protein kinase A increases release of Ca2+ by SR Recruitment, summation, preload, and contractility are varied to vary force. Formation of latch-bridges reduces speed of contractility.