Case Study 3 & 4
advertisement

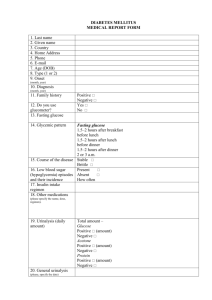
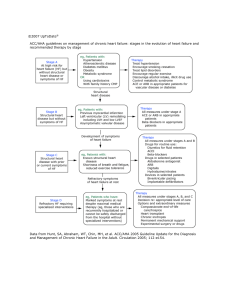
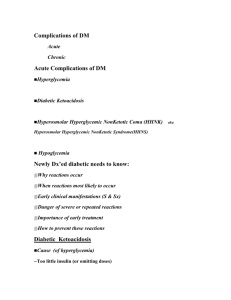
Running Head: CASE STUDY 3 & 4 (J. Gutsjo) 1 Case Study 3 & 4 Jessica L. Gutsjo Wright State University-CoNH Nur 7102 - 01 CASE STUDY 3 AND 4 (J. Gutsjo) 2 Case Study 3 1. What is this patient’s diagnosis? Explain your answer. Be certain to state diagnostic criteria. The patient’s diagnosis is Hyperglycemic Hyperosmolar Syndrome (HHS). This particular patient presented to the emergency department with a number of signs and symptoms congruent with the diagnosis of Hyperglycemic Hyperosmolar Syndrome (HHS). HHS develops over days or weeks whereas Diabetic Ketoacidosis (DKA) develops rapidly within a few hours of the precipitating event (Chaithongdi, Subauste, Koch, & Geraci, 2011). The patient’s symptoms had been present for the two weeks prior to seeking medical attention. There are a number of signs required to make the diagnosis of HHS. The patient must present with hyperglycemia, a serum glucose greater than 600 mg/dL (Chaithongdi et al., 2011 & Longo et al., 2011 & Kitabchi, Umpierrez, Miles, & Fisher, 2009), and this particular patient presents with a serum glucose of 1,489 mg/dL. In comparison, serum glucose between 240 and 600 mg/dL is indicative of DKA (Chaithongdi et al., 2011 & Longo et al., 2011 & Kitabchi et al., 2009). Another sign of HHS is a pH greater than 7.3 (Chaithongdi et al., 2011 & Kitabchi et al., 2009); an arterial blood gas was not obtained on this patient in order to assess pH. However, a pH less than 7.3 is indicative of DKA (Chaithongdi et al., 2011 & Kitabchi et al., 2009). In addition, a serum bicarbonate value greater than 15 mEq/L is indicative of HHS, whereas a value less than 18 mEq/L is indicative of DKA (Chaithongdi et al., 2011 & Kitabchi et al., 2009); 19mmol/L is this particular patient’s serum bicarbonate value. The patient’s urinalysis was positive for ketones and glucose; both are congruent findings with HHS (Kitabchi et al., 2009). Symptoms associated with HHS include; polyuria, polydipsia, weight loss, weakness, drowsiness, orthostatic dizziness, and dry mucous membranes (Chaithongdi et al., 2011 & Roppolo, 2007). The patient presented with polyuria, polydipsia, weight loss, and dry mucous CASE STUDY 3 AND 4 (J. Gutsjo) 3 membranes as evidenced by frequent urination up to 10 times per day, increased thirst and consumption of two gallons of fluid per day, and a loss of an undetermined amount of weight despite the consumption of fast foods, candy, and alcohol. Individuals who have a serum osmolality greater than 320 mOsm/kg may present with early mental status changes and is indicative of HHS (Chaithongdi et al., 2011 & Kitabchi et al., 2009), whereas a serum osmolality greater than 340 mOsm/kg typically results in coma or obtundation (Nugent, 2005). Confusion, stupor, and coma are late symptoms in severe cases of HHS or DKA (Chaithongdi et al., 2011); the patient did not present with any of the previously stated neurological changes. The patient’s serum osmolality was not provided with the case study; however, an estimate can be calculated by utilization of the following formula: “[2 x (serum sodium + serum potassium) + plasma glucose (mg/dL)/18 + BUN/2.8]” (Longo et al., 2011, p. 2979). 325 mOsm/mL is the patient’s calculated serum osmolality and is congruent with the findings of HHS and the patient was mildly agitated, an early mental status change, upon assessment. However, serum osmolality findings will be elevated with hyperglycemia but can be falsely lower due to alcohol use (Gomella & Haist, 2007), as evidenced by his oral intake of 12 to 20 beers daily for the prior seven years. 2. What are potential precipitants of HHS in this patient? Explain. Include information on the mechanism. This particular patient exhibits two precipitating factors for HHS, undiagnosed type-2 diabetes and substance abuse. There are a number of additional potential precipitating factors in the development of HHS; acute illnesses, medications, noncompliance, new-onset diabetes, substance abuse, and endocrine abnormalities (Chaithongdi et al., 2011). 32-60% of HHS events is due to infection and is the most common cause to HHS development (Chaithongdi et al., 2011 CASE STUDY 3 AND 4 (J. Gutsjo) 4 & Kitabchi et al., 2001). Viral diseases, pneumonia, pelvic inflammatory disease, urinary tract infection, dental infection, and sepsis are the most common infections linked to HHS (Chaithongdi et al., 2011, & Kitabchi, Umpierrez, Murphy, & Kreisberg, 2006, & Longo et al., 2011). Co-existing diseases including; cerebrovascular accident, myocardial infarction, major trauma, and other acute illnesses may also precipitate HHS (Chaithongdi et al., 2011, & Kitabch et al., 2006, & Longo et al., 2011). This particular patient admits to substance abuse, including the use of alcohol as evidenced by consuming 12-20 beers per day for the last seven days, crack cocaine and marijuana use in the last two days prior to seeking medical attention. Adrenal secretion of counter regulatory hormones, specifically epinephrine and norepinephrine, is stimulated by the use of cocaine (Chaithongdi et al., 2011). The ability to metabolize carbohydrates and the secretion of insulin by the pancreas is ceased when there is an increased production of epinephrine and norepinephrine (Chaithongdi et al., 2011). Glucose production is also increased when there is an increase of epinephrine production (Chaithongdi et al., 2011). Consequently, the patient presents with hyperglycemia and is partially attributed to the use of cocaine due to cocaine’s inhibitory effects on the secretion of insulin from the pancreas and increased levels of counter regulatory hormones (Abraham & Khardori, 1999 & Chaithongdi et al., 2011). A number of medications can precipitate the development of HHS; particularly medications affecting carbohydrate metabolism, medications causing dehydration, and medications increasing serum blood glucose (De Beer et al., 2008 & Kitabchi et al., 2001). Examples of medications include; calcium channel blockers, steroids, diuretics, and total parenteral nutrition (De Beer et al., 2008 & Kitabchi et al., 2001). CASE STUDY 3 AND 4 (J. Gutsjo) 5 Dehydration due to restricted water intake is another potential precipitating factor in the development of HHS. Restricted water intake can be seen in bedridden patients and patients with altered thirst response due to stroke or dementia (Kitabchi et al., 2009 & Longo et al., 2011). This particular patient has undiagnosed type-2 diabetes with a strong familial history and is the rationale for the development of HHS in 20% of individuals who are diagnosed with HHS (Kitabchi et al., 2009). When individuals are not diagnosed with diabetes, he or she is unable to recognize the symptoms of hyperglycemia and has not been receiving the correct medication treatment for their diabetes leading to severe dehydration (De Beer et al., 2008 & Kitabchi et al., 2009). In addition, the interruption of or deficient insulin therapy in type-2 diabetics can lead to HHS (Longo et al., 2011). Complications associated with peritoneal dialysis and hemodialysis can precipitate HHS (De Beer et al., 2008). Endocrine abnormalities; such as, acromegaly, thyrotoxicosis, and Cushing’s syndrome have also been linked to the development of HHS (Chaithongdi et al., 2011). 3. What type of IV replacement is appropriate for this patient? Be specific. Explain your rationale. Volume depletion, up to nine liters, is one of the key features in the diagnosis of HHS (Chaithongdi et al., 2011). Dehydration is typically more profound in HHS in comparison to DKA due to the longer duration of illness (Longo et al., 2011). The initial fluid therapy is focused towards expansion of intravascular, interstitial, and intracellular volume (Hillman, 1987). Another goal of fluid resuscitation is to replace half of the expected volume deficit over the first 12-24 hours (Chaithongdi et al., 2011). However, the rate of volume deficit correction needs to be monitored due to the risk of cerebral edema development associated with rapid volume correction (Brenner, 2006). In addition, an evaluation of cardiac compromise and renal CASE STUDY 3 AND 4 (J. Gutsjo) 6 function is critical prior to treatment to prevent fluid overload (Chaithongdi et al., 2011), neither is evident in this patient. If this particular patient were to be experiencing hypovolemic shock, as evidenced by at systolic blood pressure less than 90 mmHg and a heart rate greater than 100 beats per minute, isotonic fluid (0.9% sodium chloride) boluses would be administered one liter per hour to reinstate normotension and a normal heart rate (De Beer et al., 2008). However, this patient is not exhibiting signs of shock or hypotension and as a result the liter boluses of 0.9% sodium chloride are not indicated at this time. The patient appears to be hyponatremic as evidenced by serum sodium of 113 mmol/L and is caused by the excessive amount of circulating glucose in the blood causing a shift of water to the extracellular compartments from the intracellular compartments (Chaithongdi et al., 2011). A study suggests “for each 100mg/dL increment in serum glucose above normal resulted in an expected decrease of 2.4mmol/L (2.4mEq/L) in measured serum sodium” (Hillier, Abbott, & Barrett, 1999, p. 401). Therefore, corrected serum sodium needs to be calculated by utilization of the following formula: “measured sodium + 0.024 x serum glucose - 100)” (Hillier et al., 1999, p. 402). 135.22 mEq/L, normonatremia, is the corrected serum sodium for this particular patient. Due to the patients corrected serum sodium exhibiting normonatremia, 0.45% sodium chloride is the fluid of choice at a rate of 250-500mL/hour (Kitabchi et al, 2009 & Chaithongdi et al., 2011). However, if the patient was hyponatremic, 0.9% sodium chloride would be infused in its place at a rate of 15-20 mL/kg/hour, 1050-1400mL/hr based upon the patients weight of 70kg, during the first hour of fluid resuscitation (Kitabchi et al, 2009 & Chaithongdi et al., 2011). When blood glucose reaches 300 mg/dL the fluids will be changed to 5% dextrose with 0.45% sodium chloride at a rate of 150-250mL/hr to avoid hypoglycemia and cerebral edema CASE STUDY 3 AND 4 (J. Gutsjo) 7 and allows for the continued administration of insulin (Brenner, 2006 & Chaithongdi et al., 2011 & Kitabchi et al, 2009). 4. What is the proper initial insulin regimen for this 70-kg patient? Be specific. Explain your rationale. Prior to the start of insulin therapy, the patient’s serum potassium level should be assessed. Some patients may present with hypokalemia and the administration of insulin may decrease potassium levels even further, due to the insulin forcing the potassium into the cells (De Beer et al., 2008 & McNaughton, Self, & Slovis, 2011). The serum potassium value should be greater than 3.5 mEq/L prior to the start of insulin therapy (De Beer et al., 2008 & McNaughton et al., 2011). Hypokalemia leads to muscle weakness and life-threatening cardiac arrhythmias (De Beer et al., 2008 & McNaughton et al., 2011). This particular patient does not require supplemental potassium due to his potassium value of 5.5 mmol/L (5.5 mEq/L). There are a number of opinions on the route of administration for insulin therapy. Intravenous (IV) regular insulin therapy is recommended as the most effective method in comparison to subcutaneous (SQ) and intramuscular (IM) routes due to the unreliability of absorption (Chiasson et al., 2003 & McNaughton et al., 2011). The proper initial insulin regimen for this 70-kg patient is a bolus of IV regular insulin at a rate of 0.1 units/kg, to a maximum of 10 units, or 7 units (Longo et al., 2011& McNaughton et al., 2011). Subsequently, the infusion rate of regular insulin should be continued at 0.1units/kg/hour, 7 units/hour in this patient there after (Kitabchi et al., 2001 & Longo et al., 2011 & McNaughton et al., 2011). The objective of therapy is to reduce blood glucose by 2-3mmol/L/hour, 36-54mg/dL/hour. If the serum glucose is not decreasing at the desired rate, the CASE STUDY 3 AND 4 (J. Gutsjo) 8 IV regular insulin rate should be doubled every hour until there is a decrease of 3-4mmol/L/hour, or 54-72 mg/dL/hour (Chiasson et al., 2003 & Longo et al., 2011). The pathology of continuous IV therapy with regular insulin is the concept of insulin decreasing the serum glucose level by decreasing hepatic glucose production and increasing tissue glucose uptake and cessation of ketone production by decreasing lipolysis and glucagon excretion (Chaithongdi et al., 2011). A precaution with IV regular insulin therapy is the risk of cerebral edema due to the rapid decrease of serum glucose (Brenner, 2006). Also, patients with HHS are sensitive to insulin and extremely obese patients may require higher doses of insulin to decrease their serum glucose levels (De Beer et al., 2008). When blood glucose reaches 13.9-16.7 mmol/L, or 250-300mg/dL, the insulin rate should be decreased to 0.05-0.1units/kg/hour, 3.5-7units/hour in this patient, and the IV fluids would also be changed at this time (De Beer et al., 2008 & Longo et al., 2011). IV insulin therapy should be continued for 12-24 hours after the hyperglycemia has been corrected to clear ketones from the body (Chaithongdi et al., 2011). Also, the IV insulin therapy should not be discontinued until 1-2 hours after the start of SQ insulin therapy to ensure sufficient plasma insulin levels are sustained, therefore avoiding repeated hyperglycemia (Kitabchi & Nyenwe, 2006). Lastly, prescribing the patient with long-acting and rapid-acting SQ insulin is highly recommended to decrease the likelihood of hypoglycemia and delivers a better physiologic arrangement of control (Chaithongdi et al., 2011). 5. What differentiates HHS from DKA. Use table format. Be certain to address blood glucose levels, acidosis, serum bicarbonate levels, ketones, serum osmolality, and anion gap. Use a variety of references for the table. CASE STUDY 3 AND 4 (J. Gutsjo) 9 Table 1. Diagnostic Criteria of HHS and DKA. HHS DKA Serum glucose levels (mg/dL) >600 240–600 Arterial pH/Acidosis >7.3 Serum bicarbonate level >15 (HCO3-) (mmol/L) Mild DKA Moderate DKA Severe DKA 7.25-7.30 7.0-<7.24 <7.0 Mild DKA Moderate DKA Severe DKA 15-18 10-<15 <10 Urine & Serum Ketones Small Positive Serum osmolality (mmol/kg) >320 Variable (2 x sodium) + (glucose) Anion gap (Na) – [Cl + HCO3-(mmol/L)] Variable Mild DKA Moderate DKA Severe DKA >10 >12 >12 Table 1. Adapted from “Hyperglycemic crises in adult patients with diabetes,” by Kitabchi, A. E., Umpierrez, G. E., Miles, J. M., & Fisher, J. N., 2009, Diabetes Care, 32(7), p. 1336. Adapted with permission from authors. CASE STUDY 3 AND 4 (J. Gutsjo) 10 References Abraham, M., & Khardori, R. (1999). Hyperglycemic hyperosmolar nonketotic syndrome as initial presentation of type 2 diabetes in a young cocaine abuser. Diabetes Care, 22(8), 1380-1381. Brenner, Z. R. (2006). Management of hyperglycemic emergencies. AACN Clinical Issues, 17, 56-65. Chaithongdi, N., Subauste, J. S., Koch, C. A., & Geraci, S. A. (2011). Diagnosis and management of hyperglycemic emergencies. Hormones, 10(4), 250-260. Chiasson, J. L., Aris-Jilwan, N., Belanger, R., Bertrand, S., Beauregard, H., Ekoe, J. M., . . . Havrankova, J. (2003). Diagnosis and treatment of diabetic ketoacidosis and the hyperglycemic hyperosmolar state. Canadian Medical Association Journal, 168, 859866. De Beer, K., Michael, S., Thacker, M., Wynne, E., Pattni, C., Gomm, M., . . . Ullah, K. (2008). Diabetic ketoacidosis and hyperglycemic hyperosmolar syndrome – clinical guidelines. British Association of Critical Care Nurses, Nursing in Critical Care, 13(1), 5-11. Gomella, L. G., Haist, S. A. (2007). Clinician's pocket reference. New York: McGraw-Hill Companies, Inc. Hillier, T. A., Abbott, R. D., & Barrett, E. J. (1999). Hyponatraemia: evaluating the correction factor for hyperglycemia. American Journal of Medicine, 106, 399-403. Hillman, K. (1987). Fluid resuscitation in diabetic emergencies: a reappraisal. Intensive Care Medicine, 13, 4-8. Kitabchi, A. E., & Nyenwe, E. A. (2006). Hyperglycemic crisis in diabetes mellitus: Diabetic ketoacidosis and hyperosmolar state. Endocrinology and Metabolism Clinics of North America, 35, 725-751. CASE STUDY 3 AND 4 (J. Gutsjo) 11 Kitabchi, A. E., Umpierrez, G. E., Miles, J. M., & Fisher, J. N. (2009). Hyperglycemic crises in adult patients with diabetes. Diabetes Care, 32(7), 1335-1343. Kitabchi, A. E., Umpierrez, G. E., Murphy, M. B., Barrett, E. J., Kreisberg, R. A., Malone, J. I., & Wall, B. M. (2001). Management of hyperglycemic crisis in patients with diabetes. Diabetes Care, 24, 131-153. Kitabchi, A. E., Umpierrez, G. E., Murphy, M. B., & Kreisberg, R. A. (2006). Hyperglycemic crises in adult patients with diabetes. Diabetes Care, 29, 2739-2748. Longo, D. L., Kasper, D. L., Jameson, J. L., Fauci, A. S., Hauser, S. L., & Loscalzo, J. (2011). Harrison’s principles of internal medicine (18th ed.). New York, NY: McGraw-Hill Companies, Inc. McNaughton, C. D., Self, W. H., & Slovis, C. (2011). Diabetes in the emergency department: Acute care of diabetes patients. Clinical Diabetes, 29(2), 51-59. Nugent, B. W. (2005). Hyperosmolar hyperglycemic state. Emergency Medicine Clinics of North America, 23, 629-648. Roppolo, L. P. (2007). Emergency medicine handbook: Critical concepts for clinical practice. Philadelphia, PA: Mosby. CASE STUDY 3 AND 4 (J. Gutsjo) 12 Case Study 4 A 26-year old Caucasian female is seen in the emergency department with complaints of palpitations, fatigue, weakness, and menstrual irregularity. She reports having loose stools during the past four weeks, 30-pound weight loss in the past three months despite an insatiable appetite, and heat intolerance for the past two weeks. She admits to smoking one to two packs of cigarettes per day for the past nine years. She has experienced feelings of anxiousness, depression, and increased irritability as well. She denies fever, chills, headache, dyspnea, chest pain, and vertigo. On physical examination, she has a tremor in her hands with her arms extended. She weighs 90-pounds at 5 feet, 3 inches. Examination also revealed tachycardia, at 124 BPM, and hypertension, at 162/87 mm Hg. HEENT findings consists upper eyelid retraction and proptosis. Warm, moist skin was noted in addition to localized thickening of the pretibial area. The anterior aspect of her neck appeared full and firm upon palpation with no bruit noted. Other examination findings are within normal limits. The CXR is normal. Initial laboratory studies revealed serum calcium of 11.0 mg/dL, phosphorus of 1.9 mg/dL, magnesium of 1.7 mg/dL, glucose of 240mg/dL, potassium of 3.2mEq/L, and all other electrolytes are normal. Hematologic findings included: WBC of 7,000/mm3, Hb of 9.8 g/dL, HCT of 29.4%, and platelets of 200,000/mm3. Thyroid function studies found: TSH decreased/undetectable, total T4 of 15.8 µg/dL, free T4 of 3.8 ng/dL, total T3 of 252 ng/dL, and free T3 of 13.6 pg/dL. 1. What is this patient's diagnosis? Explain your answer. Be certain to state diagnostic criteria. This patient’s diagnosis is Graves’ disease (GD). This particular patient presents with a number of symptoms that are congruent with the findings of GD; irritability, anxiousness, depression, heat intolerance, palpitations, fatigue, weakness, menstrual irregularity, loose stools, and weight loss despite an insatiable appetite (Longo et al., 2011). Additionally, the patient’s signs are congruent with the diagnosis of GD; tachycardia, tremor, full and firm neck upon palpation; most likely a goiter, warm-moist skin, localized thickening of the pretibial area; most likely pretibial myxedema; and upper eyelid retraction and proptosis; ophthalmopathy (Longo et al., 2011). CASE STUDY 3 AND 4 (J. Gutsjo) 13 In the presence of GD, the thyroid stimulating hormone (TSH) will reveal a low or suppressed value while the total levels of triiodothyronine (T3) and thyroxine (T4) are increased, commonly in a ratio greater than 20:1 respectively (Longo et al., 2011 & Yanagisawa et al., 2005). This patient’s thyroid function studies revealed an undetectable level of TSH while total T3 and T4 were elevated with a ratio greater than 20:1 as evidenced by total T3 of 252 ng/dL and T4 of 15.8 µg/dL. In patients with GD, the diagnosis is confirmed with laboratory examination, palpation of a goiter, presence of ophthalmopathy, dermopathy, and personal or family history of autoimmune disorders (Longo et al., 2011 & Wondisford & Radovick, 2009). When ophthalmopathy and thyroid hyperfunction occur simultaneously, the diagnosis of GD is definitive (Wondisford & Radovick, 2009), as seen in this patient. Conversely, when a goiter is palpable on a patient in the presence of a normal TSH value the diagnosis of GD is excluded (Longo et al., 2011), but is not the case for this patient. 2. Provide an explanation why the patient is experiencing heat intolerance, tachycardia, weight loss, and hypertension. When an individual is experiencing thyrotoxicosis; a condition of thyroid hormone excess, their levels of thyroid hormones will be elevated due to an overactive thyroid gland producing a disproportionate amount of thyroid hormones (Longo et al., 2011), as seen in this patient. The patient’s heat intolerance for the past two weeks is caused by the increase in oxygen consumption due to the increased levels the T3 and T4 (Longo et al., 2011). The patient’s tachycardia is due to the thyroid hormones inducing the production of proteins, inducing the beta-1 receptors in the heart (Longo et al., 2011). Inducing the beta-1 receptors of the sinoatrial node, produce an increased heart rate, a positive chronotropic effect (Longo et al., 2011). The CASE STUDY 3 AND 4 (J. Gutsjo) 14 patient’s 30-pound weight loss in the past three months despite an insatiable appetite is due to the increased thyroid hormones causing an increase in the basal metabolic rate with an increase in nutrient and oxygen consumption (Longo et al., 2011). The patient’s hypertension is attributed to her increase in cardiac output caused by the tachycardia and increase of contractility (Longo et al., 2011). 3. Does this patient present with the manifestations indicating the need for a thyroidectomy? A number of signs and symptoms need to be manifested to indicate the need for a thyroidectomy; (1) patient preference, (2) thyrotoxicosis control, (3) pregnant individual or adolescent intolerant of anti-thyroid medications, (4) large goiter, with or without compressive symptoms, (5) severe ophthalmopathy, or (6) suspicious nodules (Winsa et al., 1994). The patient presents with a few signs that would indicate the probable need for a thyroidectomy. However, the patient’s preference and pregnancy status is not indicated in this case study. In addition, the patient is not an adolescent and has not been taking anti-thyroid medications. Antithyroid medications may be administered to rule out their effectiveness in correcting the thyroid hormones prior to deciding if the surgery is necessary. However, the anterior aspect of her neck appears full and is firm upon palpation with no bruit noted but compressive symptoms, difficulties with breathing or swallowing, are not noted in this patient. Additionally, the patient presents with ophthalmopathy but the severity is not noted in this case study. The severity of ophthalmopathy can be assessed by measuring the degree of proptosis, diplopia, and optic neuropathy (Bartalena, Pinchera, & Marcocci, 2000). Mild ophthalmopathy is indicated as a proptosis of 19-20mm, intermittent diplopia, and 9/10 visual acuity (Bartalena et al., 2000). Moderate ophthalmopathy is indicated as a proptosis of 21-23mm, variable diplopia, and 8/10- CASE STUDY 3 AND 4 (J. Gutsjo) 15 5/10 visual acuity (Bartalena et al., 2000). Severe ophthalmopathy is indicated as a proptosis of greater than 23mm, constant diplopia, and less than 5/10 visual acuity (Bartalena et al., 2000). However, only 3-5% of cases of ophthalmopathy are severe cases (Burch & Wartofsky, 1993). The patient does not present with suspicious nodules to indicate the necessity for surgery. 4. What increases the probability for developing ophthalmopathy and what teaching points are imperative to make with this patient? Ophthalmopathy associated with GD is the most common extrathyroidal sign (Wiersinga & Bartalena, 2002). Nearly half of the patients with GD will present with ophthalmopathy; however, this statistic increases when computed tomography, CT, imaging is performed (Ozgen et al., 1999). A major contributing factor to this patient’s ophthalmopathy is her habit of smoking one to two packets of cigarettes per day for the past nine years. Smoking increases ones risk of developing GD and particularly the development of ophthalmopathy in individuals who are diagnosed with GD (Vestergaard, 2002 & Pummel & Wiersinga, 1993). However, individuals with the most pronounced ophthalmopathy smoke the greatest (Vestergaard, 2002). Additionally, smoking enhances the advancement of ophthalmopathy after radioactive iodine treatment, a particular treatment for GD, and decreases the efficiency of orbital radiation and glucocorticoid therapy, additional specific treatment modalities for GD (Bartalena et al., 1998). Conclusively, smoking greatly affects the progression of ophthalmopathy and diminishes the effectiveness of established treatments. Smoking cessation is imperative for this patient due to her diagnosis of GD with ophthalmopathy involvement. CASE STUDY 3 AND 4 (J. Gutsjo) 16 References Bahn, R. S. (2002). TSH receptor expression in orbital adipose/connective tissues from patients with thyroid-associated ophthalmopathy. Thyroid, 12, 193-195. Bartalena, L. Marcocci, C., Tanda, M. L., Manetti, L., Dell’Unto, E., Bartolomei, M. P., . . . Pinchera, A. (1998). Cigarette smoking and treatment outcomes in Graves’ ophthalmopathy. Annals of Internal Medicine, 129(8), 632-635. Bartalena, L., Pinchera, A., & Marcocci, C. (2000). Management of Graves’ ophthalmopathy: Reality and perspectives. Endocrine Reviews, 21, 168-199. Besser, G. M., & Thorner, M. O. (2002). Comprehensive clinical endocrinology. Edinburgh: Mosby. Burch, H. B., & Wartofsky, L. (1993). Graves’ ophthalmopathy: Current concepts regarding pathogenesis and management. Endocrine Reviews, 14, 747-793. Fischbach, F. T., & Dunning, M. B. (2009). A manual of laboratory and diagnostic tests. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. Longo, D. L., Kasper, D. L., Jameson, J. L., Fauci, A. S., Hauser, S. L., & Loscalzo, J. (2011). Harrison’s principles of internal medicine (18th ed.). New York, NY: McGraw-Hill Companies, Inc. Ozgen, A., Alp, M. N., Ariyurek, M., Tutuncu, N. B., Can, I., & Gunlap, I. (1999). Quantitative CT of the orbit in Graves’ disease. The British Journal of Radiology, 72, 757-762. Pummel, M. F. & Wiersinga, W. M. (1993). Smoking and risk of Graves’ disease. Journal of the American Medical Association, 269, 479-482. Vestergaard, P. (2002). Smoking and thyroid disorders – a meta-analysis. European Journal of Endocrinology, 146, 153-161. CASE STUDY 3 AND 4 (J. Gutsjo) 17 Wiersinga, W. M. & Bartalena, L. (2002). Epidemiology and prevention of Graves’ ophthalmopathy. Thyroid, 12, 855-860. Wiersinga, W. M. & Prummel, M. F. (2001). Pathogenesis of Graves’ ophthalmopathy: Current understanding. Journal of Clinical Endocrinology & Metabolism, 86, 501-503. Winsa, B., Rastad, J., Larsson, E., Mandahl, A., Westermark, K., Johansson, H., . . . Akerström, G. (1994). Total thyroidectomy in therapy-resistant Graves’ disease. Surgery, 116, 10681074. Wondisford, F. E., & Radovick, S. (2009). Clinical management of thyroid disease. Philadelphia: Saunders/Elsevier. Yanagisawa, T., Sato, K., Kato, Y., Shimizu, S., & Takano, K. (2005). Rapid differential diagnosis of Graves ’ disease and painless thyroiditis using total T3/T4 ratio, TSH, and total alkaline phosphatase activity. Endocrine Journal, 52(1), 29-36.