RFP#901004 - Alameda County Government
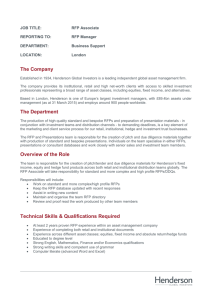
advertisement

**IMPORTANT NOTICE** The format of this RFP has been simplified. Only the following pages require signatures: 1. 2. Exhibit A – Bid Response Packet, Bidder Information and Acceptance page a. Must be signed by Bidder Exhibit A – Bid Response Packet, SLEB Partnering Information Sheet a. Must be signed by Bidder b. Must be signed by SLEB Partner if subcontracting to a SLEB Please read EXHIBIT A – Bid Response Packet carefully, INCOMPLETE BIDS WILL BE REJECTED. Alameda County will not accept submissions or documentation after the bid response due date. COUNTY OF ALAMEDA REQUEST FOR PROPOSAL No. 901004 for Behavioral Health Management Information System For complete information regarding this project, see RFP posted at http://www.acgov.org/gsa_app/gsa/purchasing/bid_content/contractopportunities.jsp or contact the County representative listed below. Thank you for your interest! Contact Person: Ryan DeCoud, Contracts Specialist I Phone Number: (510) 208-9619 E-mail Address: ryan.decoud@acgov.org RESPONSE DUE by 2:00 p.m. on May 2, 2013 at Alameda County, GSA–Purchasing 1401 Lakeside Drive, Suite 907 Oakland, CA 94612 Alameda County is committed to reducing environmental impacts across our entire supply chain. If printing this document, please print only what you need, print double-sided, and use recycledcontent paper. 1401 Lakeside Drive, Suite 907 Oakland, CA 94612 Phone: 510-208-9600 Website: http://www.acgov.org/gsa/departments/purchasing/ I:\PURCHASING\Contracting Opportunities\Purchasing\Behavioral Health Management Information System \RFP_BHMIS.doc Revision 2012-11-02 COUNTY OF ALAMEDA REQUEST FOR PROPOSAL No. 901004 SPECIFICATIONS, TERMS & CONDITIONS for Behavioral Health Management Information System TABLE OF CONTENTS Page I. II. III. IV. STATEMENT OF WORK ........................................................................................................... 4 A. INTENT ................................................................................................................................. 4 B. SCOPE................................................................................................................................... 4 C. BACKGROUND ..................................................................................................................... 5 D. VENDOR QUALIFICATIONS .................................................................................................. 7 E. SPECIFIC REQUIREMENTS .................................................................................................... 8 F. DELIVERABLES/REPORTS ................................................................................................... 12 CALENDAR OF EVENTS ......................................................................................................... 13 G. NETWORKING / BIDDERS CONFERENCES .......................................................................... 13 COUNTY PROCEDURES, TERMS, AND CONDITIONS ............................................................... 14 H. EVALUATION CRITERIA / SELECTION COMMITTEE............................................................ 14 I. CONTRACT EVALUATION AND ASSESSMENT .................................................................... 20 J. NOTICE OF INTENT TO AWARD ......................................................................................... 20 K. TERM / TERMINATION / RENEWAL ................................................................................... 21 L. BRAND NAMES AND APPROVED EQUIVALENTS ............................................................... 21 M. QUANTITIES ....................................................................................................................... 22 N. PRICING .............................................................................................................................. 22 O. AWARD .............................................................................................................................. 23 P. METHOD OF ORDERING .................................................................................................... 24 Q. WARRANTY ........................................................................................................................ 25 R. INVOICING ......................................................................................................................... 25 S. ACCOUNT MANAGER / SUPPORT STAFF ........................................................................... 26 INSTRUCTIONS TO BIDDERS ................................................................................................. 26 T. COUNTY CONTACTS ........................................................................................................... 26 U. SUBMITTAL OF BIDS .......................................................................................................... 27 V. RESPONSE FORMAT ........................................................................................................... 29 ATTACHMENTS Exhibit A – Bid Response Packet Exhibit B – Insurance Requirements Exhibit C – Functional / Technical Requirements Detail Specifications, Terms & Conditions for Behavioral Health Management Information System I. STATEMENT OF WORK A. INTENT It is the intent of these specifications, terms and conditions to describe the Behavioral Health Management Information System (BHMIS) including a certified Electronic Health Record (EHR) module required by the County of Alameda Department of Behavioral Health Care Services (ACBHCS). The County intends to award a three-year contract with option to renew to the bidder selected as the most responsible bidder whose response conforms to the RFP and meets the County’s requirements. B. SCOPE ACBHCS is seeking a modern state-of-the-art integrated BHMIS through acquisition of the necessary software, hardware, and implementation services. This system will support all mental health and substance abuse programs and related clinical, financial, management, and reporting activities at Alameda County. The Contractor will be responsible for the enhancement, customization, configuration, and maintenance of all system components for the BHMIS and EHR. Any proposed solution must fully comply with all Federal and State laws concerning the operational requirements with which all California counties are obligated to comply. The complexity of the various laws is reflected in the many subordinate behavioral/mental health business processes that California counties support. The Specific Requirements section below outlines the functional, technical, and business requirements that the system must be able to support, and specific services to be provided, under this Request for Proposal. Exhibit C provides the Functional Requirements detail. The selected vendor must bring the entire range of necessary corporate and key staff capabilities and experience, either as a single Contractor or in conjunction with complementary subcontractors or partners. A single organizational entity must assume responsibility for all work and services performed under the executed contract regardless of whether any subcontractors or partners are involved. As such, the successful respondent may be a BHMIS Contractor, the supplier of other Behavioral Health systems, or a systems integrator. RFP No. 901004 Page 4 Specifications, Terms & Conditions for Behavioral Health Management Information System C. BACKGROUND ACBHCS provides direct care to adults, adolescents and children who are mentally ill and/or substance abusers through its own outpatient clinics and through contracted providers. ACBHCS is also responsible for administration of other County Behavioral Health programs including Medi-Cal mental health managed care, vocational rehabilitation, and employment services. ACBHCS currently uses a 16 year-old system to track patients as they progress through treatment, the system is primarily a billing system but has been modified over time to track patient information. The system is called InSyst and is maintained by the vendor (Echo Group). The County currently relies on a wide variety of legacy and ad hoc data source systems to track data of all types: billing and financial, client services, and mandated state and other government reporting. It is ACBHCS’s intent to eliminate the disparate information systems and/or databases that are identified in this RFP by having the Contractor assist in completing a needs assessment for each disparate system that includes, but is not limited to, business process and system functionality review and data analysis for the purpose of transitioning the data, functionality and reporting requirements into the proposed BHCMIS. For purposes of vendor awareness, following is a list of some of the processes for which California Counties are accountable per California law, in the delivery of behavioral health services: 1. Managed Care a. 2. ACBHCS is both an intermediary for a subcontracted managed care provider network and a direct provider of services. ACBHCS participates in capitated managed care and contracts for services on that basis. ACBHCS requires that the BHMIS system have a robust managed care module. This module must be capable of supporting ACBHCS role as a managed care administrator (with contracted sub-capitated or otherwise reimbursed providers) and as a network provider. Uniform Method of Determining Ability to Pay (UMDAP) a. The UMDAP process is a sliding scale based on the client’s or responsible party’s ability to pay for the costs of mental health services provided. Other required activities inherent in the UMDAP process include billing, RFP No. 901004 Page 5 Specifications, Terms & Conditions for Behavioral Health Management Information System accounts receivable maintenance and reporting, and collections and write off. 3. Client and Service Information (CSI) a. 4. The CSI System is the State data system that collects, edits, and reports client demographic, diagnostic service, and outcome information on the entire California public mental health population. Each California County is responsible for ongoing data collection and monthly transmission of that data electronically via the Department of Mental Health (DMH) Information Technology Web Services (ITWS) system. Alcohol / Drug Medi-Cal Reimbursement a. Certain alcohol and drug services are covered for Medi-Cal eligible clients. Unlike other services provided by counties, Drug Medi-Cal (DMC) is a statewide entitlement program. b. There are four different treatment services that can be billed to DMC: (1) Narcotic Treatment Programs (NTP) (a) Methadone Dosing (b) LAAM Dosing (c) Individual Counseling (d) Group Counseling (2) Day Care Habilitative (DCH) (3) Perinatal Residential (RES) (4) Outpatient Drug Free (ODF) (a) Individual Counseling (b) Group Counseling RFP No. 901004 Page 6 Specifications, Terms & Conditions for Behavioral Health Management Information System 5. California Outcomes Measurement System (CalOMS) a. 6. Prevention Services a. D. CalOMS is a centralized alcohol and other drug (AOD) data collection system. Reporting participant data to CalOMS involves collecting of information each time a participant is enrolled for AOD treatment services at a reporting facility and subsequent transfers or changes in service. Providers submit CalOMS data (to include “Private Pay” clients) to their county throughout each month. The data, submitted by the county to Alcohol and Drug Programs (ADP), is processed through an electronic computerized data system for inclusion in the statewide CalOMS data repository. Preventative services are considered the first level of healthcare and are designed to prevent disease and promote health. The system will be required to capture de-identified, aggregate demographic data as related to prevention services. System must also have the capability of tracking people that do not have a mental health diagnosis. VENDOR QUALIFICATIONS 1. Vendor Minimum Qualifications a. Bidder shall be regularly and continuously engaged in the business of providing a fully functional behavioral health client record management, electronic health record, billing, claiming and managed care system software, maintenance and support for at least three (3) years, to a California County. b. Bidder shall be a certified Electronic Health Records System software provider, according to the electronic health record certification standards established by the Centers for Medicare and Medicaid Services, under the U.S. Department of Health and Human Services. c. Bidder shall possess all permits, licenses and professional credentials necessary to supply product and perform services as specified under this RFP. RFP No. 901004 Page 7 Specifications, Terms & Conditions for Behavioral Health Management Information System E. SPECIFIC REQUIREMENTS Contractor must provide all elements required to install a BHMIS and EHR, including software, a complete list of hardware including price quotations required for system operability, and implementation, including data migration, and training as required. See Exhibit C for the Specific Requirements detail. 1. Overall services and components to be acquired through this RFP encompass the following: a. A “state-of-the-art” integrated BHMIS that includes support for: (1) practice management; (2) electronic clinical records; (3) call management; (4) managed care; (5) eligibility verification; (6) claims processing; (7) Coordination of Benefits (COB)/Third Party Liability (TPL); (8) financial reporting; (9) electronic prescriptions; (10) data warehouse; and (11) report writing. b. Automated verification with the California Medi-Cal Eligibility Data System (MEDS). c. Electronic digital signature (client and clinical staff) functionality supporting the electronic clinical record. d. Imaging and document management capabilities. e. Interoperability and external system interface capabilities. RFP No. 901004 Page 8 Specifications, Terms & Conditions for Behavioral Health Management Information System 2. 3. f. Project management, training, data conversion and system documentation. g. Ongoing system support and maintenance. h. A distributive data process achieved by sharing data bi-directionally including but not limited to: (1) report repository; (2) web services; (3) data mining services; and (4) analytical modeling services. Software must support the following functional areas (see Exhibit C, pages 1 - 56, for detail): a. Appointment Scheduling; b. Authorizations; c. Benefits and Eligibility Administration and Management; d. Billing; e. Claims Administration; f. Client Registration; g. Online Order Entry; and h. Service Delivery Management. Software must support the following technical areas (see Exhibit C, pages 56 – 72, for detail): a. System Architecture; b. Database; c. Reporting; RFP No. 901004 Page 9 Specifications, Terms & Conditions for Behavioral Health Management Information System 4. d. Security; e. EDI; f. Ease of use; g. System Reliability; h. Production Scheduling and Control; i. Other Environments; j. Systems Standards; and k. Interfaces. Hardware a. 5. 6. Implementation a. Integration of past data into the new system. b. Training. c. Bidders must provide a proposed 18-24 month implementation plan with optimum timeline, steps, and phases. Testing a. 7. Bidders must provide a complete list including price quotations of all hardware and software required to implement and operate the proposed system and be prepared to provide those items as the price stated. Contractor must perform tests required to verify the system performs all functions described above. Vendor solution must provide the necessary functionality to replace ACBHCS’s existing disparate systems which include: a. INSYST: (1) The County’s current client data and billing system, INSYST, contains over twenty years of historical client demographic and episodic data. The new system must be able to import to its database all current client and episodic data. RFP No. 901004 Page 10 Specifications, Terms & Conditions for Behavioral Health Management Information System b. eCURA Historical Data: (1) c. Clinician’s Gateway: (1) d. Eighty-five percent of the services delivered by ACBHCS are provided through contracts with community based organizations (CBO). Currently these organizations utilize commercial and in-house developed client data and billing systems. The new BHMIS system must have automated processes to import administrative and service level data directly from CBO systems (e.g. Netsmart). Primary Care Health Center (PCHC) Client Data and Billing Systems: (1) f. The County’s current electronic health records and other data sets are called Clinician’s Gateway. The new system must be able to import/export client, episodic and service data with Clinician’s Gateway or an interface must be provided. Contractor Client Data and Billing Systems: (1) e. The County’s current managed care system, eCURA, contains over twelve years of client data, billing and physician payment history. The new system must be able to import to the database all current client and physician data or an interface must be provided. ACBHCS has integrated services with PCHCs that require a capacity to exchange client and service data. The new system must be able to import/export data with PCHC systems (e.g. NextGen, Epic, etc.). Medi-Cal and DCR (Denied Correction Report) Database: (1) Currently the County utilizes a SQL database, developed by in house staff, to manage and monitor the current status of the Medi-Cal 837/835 claiming processes. The new system must include this functionality for the purpose of reconciling 837 claim lines to receipt of 835 and the warrant; as well as the ability to allow providers to correct denials via user screens. This functionality can be provided through the use of a module that is fully integrated with the main database. RFP No. 901004 Page 11 Specifications, Terms & Conditions for Behavioral Health Management Information System F. DELIVERABLES/REPORTS 1. Provide a Gap Analysis. 2. Provide a list of software, applications, training materials, etc. to be delivered. Include estimated due dates and the responsible member of the vendor’s implementation team for each. 3. Before work begins, provide a final Implementation Schedule and timeline. 4. Conduct weekly status meetings during implementation via conference call with County Project staff and bidder’s implementation team. 5. Maintain an issues log and provide view access via the Internet. 6. Provide a training schedule and training materials including updates and revisions as required throughout the life of the system. 7. Upon completion of implementation, vendor is to provide a complete listing and comprehensive description of all system documentation regarding system setup, modifications and/or other changes made to the rudimentary product during implementation. RFP No. 901004 Page 12 Specifications, Terms & Conditions for Behavioral Health Management Information System II. CALENDAR OF EVENTS EVENT Request Issued Written Questions Due DATE/LOCATION February 27, 2013 by 5:00 pm on April 2, 2013 Networking/Bidders Conference #1 April 1, 2013 at 2:00 p.m. Networking/Bidders Conference #2 April 2, 2013 at 10:00 a.m. Addendum Issued Response Due Evaluation Period Vendor Interviews Board Letter Issued Board Award Date Contract Start Date April 17, 2013 May 2, 2013 May 2, 2013 – May 23, 2013 May 22 - 23, 2013 July 9, 2013 July 23, 2013 August 1, 2013 at: Social Services Agency 6th Floor, Room 637 24100 Amador Street Hayward, CA 94545 at: General Services Agency Room 1107, 11th Floor 1401 Lakeside Dr. Oakland, CA 94612 Note: Award and start dates are approximate. G. NETWORKING / BIDDERS CONFERENCES Networking/bidders conferences will be held to: 1. Provide an opportunity for small, local, and emerging businesses (SLEBs) and large firms to network and develop subcontracting relationships in order to participate in the contract(s) that may result from this RFP. 2. Provide an opportunity for bidders to ask specific questions about the project and request RFP clarification. 3. Provide the County with an opportunity to receive feedback regarding the project and RFP. All questions will be addressed, and the list of attendees will be included, in an RFP Addendum following the networking/bidders conferences. RFP No. 901004 Page 13 Specifications, Terms & Conditions for Behavioral Health Management Information System III. COUNTY PROCEDURES, TERMS, AND CONDITIONS H. EVALUATION CRITERIA / SELECTION COMMITTEE All proposals will be evaluated by a County Selection Committee (CSC). The County Selection Committee may be composed of County staff and other parties that may have expertise or experience in managing or implementing health information systems. The CSC will select a contractor in accordance with the evaluation criteria set forth in this RFP. The evaluation of the proposals shall be within the sole judgment and discretion of the CSC. All contact during the evaluation phase shall be through the GSA–Purchasing Department only. Bidders shall neither contact nor lobby evaluators during the evaluation process. Attempts by Bidder to contact and/or influence members of the CSC may result in disqualification of Bidder. The CSC will evaluate each proposal meeting the qualification requirements set forth in this RFP. Bidders should bear in mind that any proposal that is unrealistic in terms of the technical or schedule commitments, or unrealistically high or low in cost, will be deemed reflective of an inherent lack of technical competence or indicative of a failure to comprehend the complexity and risk of the County’s requirements as set forth in this RFP. Bidders are advised that in the evaluation of cost it will be assumed that the unit price quoted is correct in the case of a discrepancy between the unit price and an extension. As a result of this RFP, the County intends to award a contract to the responsible bidder(s) whose response conforms to the RFP and whose bid presents the greatest value to the County, all evaluation criteria considered. The combined weight of the evaluation criteria is greater in importance than cost in determining the greatest value to the County. The goal is to award a contract to the bidder(s) that proposes the County the best quality as determined by the combined weight of the evaluation criteria. The County may award a contract of higher qualitative competence over the lowest priced response. The basic information that each section should contain is specified below, these specifications should be considered as minimum requirements. Much of the material needed to present a comprehensive proposal can be placed into one of the sections listed. However, other criteria may be added to further support the evaluation process whenever such additional criteria are deemed appropriate in considering the nature of the goods and/or services being solicited. RFP No. 901004 Page 14 Specifications, Terms & Conditions for Behavioral Health Management Information System Each of the Evaluation Criteria below will be used in ranking and determining the quality of bidders’ proposals. Proposals will be evaluated according to each Evaluation Criteria, and scored on the zero to five-point scale outlined below. The scores for all Evaluation Criteria will then be added, according to their assigned weight (below), to arrive at a weighted score for each proposal. A proposal with a high weighted total will be deemed of higher quality than a proposal with a lesser-weighted total. The final maximum score for any project is five hundred fifty (550) points, including the possible fifty (50) points for local and small, local and emerging, or local preference points (maximum 10% of final score). The evaluation process may include a two-stage approach including an initial evaluation of the written proposal and preliminary scoring to develop a short list of bidders that will continue to the final stage of oral presentation and interview and reference checks. The preliminary scoring will be based on the total points, excluding points allocated to references, oral presentation and interview. If the two-stage approach is used, the three (3) bidders receiving the highest preliminary scores and with at least 200 points will be invited to an oral presentation and interview. Only the bidders meeting the short list criteria will proceed to the next stage. All other bidders will be deemed eliminated from the process. All bidders will be notified of the short list participants; however, the preliminary scores at that time will not be communicated to bidders. RFP No. 901004 Page 15 Specifications, Terms & Conditions for Behavioral Health Management Information System The zero to five-point scale range is defined as follows: 0 Not Acceptable 1 Poor 2 Fair 3 Average 4 Above Average / Good 5 Excellent / Exceptional Non-responsive, fails to meet RFP specification. The approach has no probability of success. If a mandatory requirement this score will result in disqualification of proposal. Below average, falls short of expectations, is substandard to that which is the average or expected norm, has a low probability of success in achieving objectives per RFP. Has a reasonable probability of success, however, some objectives may not be met. Acceptable, achieves all objectives in a reasonable fashion per RFP specification. This will be the baseline score for each item with adjustments based on interpretation of proposal by Evaluation Committee members. Very good probability of success, better than that which is average or expected as the norm. Achieves all objectives per RFP requirements and expectations. Exceeds expectations, very innovative, clearly superior to that which is average or expected as the norm. Excellent probability of success and in achieving all objectives and meeting RFP specification. The Evaluation Criteria and their respective weights are as follows: Evaluation Criteria A. B. Weight Completeness of Response: Responses to this RFP must be complete. Responses that do not include the proposal content requirements identified within this RFP and subsequent Addenda and do not address each of the items listed below will be considered incomplete, be rated a Fail in the Evaluation Criteria and will receive no further consideration. Responses that are rated a Fail and are not considered may be picked up at the delivery location within 14 calendar days of contract award and/or the completion of the competitive process. Pass/Fail Financial Stability (See Exhibit A – Bid Response Packet) Pass/Fail RFP No. 901004 Page 16 Specifications, Terms & Conditions for Behavioral Health Management Information System C. D. Debarment and Suspension: Bidders, its principal and named subcontractors are not identified on the list of Federally debarred, suspended or other excluded parties located at www.sam.gov. Pass/Fail Functional and Technical Criteria: In each area described below, an evaluation will be made of the probability of success of and risks associated with, the proposal response. Using the information provided by the bidder in Exhibit C, each required feature will be evaluated for: 1. Overall System Design - A comparison will be made of the proposed BHMIS systems. Additional credit will be given for features of the proposed design that offer enhanced utility, ease of use or ease of integration with existing ACBHCS equipment and systems. The proposed software capabilities will be compared with the requirements of this RFP in terms of the software’s ability to replace existing ACBHCS management and data processing systems and meet all State and Federal requirements, including certification. (6 Points) 2. Life-Cycle Support - An assessment will be made of the scope and extent of resources required to operate and maintain the proposed BHMIS system. (5 Points) 3. Functional Requirements, pages 1 – 56 , Exhibit C (8 points) a. Appointment Scheduling Requirements (1 point) b. Authorization Requirements (1 point) c. Benefits Insurance Requirements (1 point) d. Billing Requirements (1 point) e. Claims Administration Requirements (1 point) f. Client Registration Requirements (1 point) g. Online Order Entry Requirements (1 point) h. Service Delivery Requirements (1 point) 4. Technical Requirements pages 56 – 72, Exhibit C (11 points) i. System Architecture Requirements (1 point) j. Database Requirements (1 point) k. Reporting Requirements (1 point) l. Security Requirements (1 point) m. EDI Requirements (1 point) n. Ease of Use Requirements (1 point) 30 Points RFP No. 901004 Page 17 Specifications, Terms & Conditions for Behavioral Health Management Information System o. System Reliability Requirements (1 point) p. Production Scheduling and Control Requirements q. Other Environments Requirements (1 point) r. System Standards Requirements (1 point) s. Interfaces Requirements (1 point) E. Cost: The points for Cost will be computed by dividing the amount of the lowest responsive bid received by each bidder’s total proposed cost. While not reflected in the Cost evaluation points, an evaluation may also be made of: 1. Reasonableness (i.e., does the proposed pricing accurately reflect the bidder’s effort to meet requirements and objectives?); (5 Points) 2. Realism (i.e., is the proposed cost appropriate to the nature of the products and services to be provided?); and (5 Points) 3. Affordability (i.e., the ability of the County to finance the equipment/system and services). (5 Points) F. G. Consideration of price in terms of overall affordability may be controlling in circumstances where two or more proposals are otherwise adjudged to be equal, or when a superior proposal is at a price that the County cannot afford. 15 Points Implementation Plan and Schedule: An evaluation will be made of the likelihood that Bidder’s implementation plan and schedule will meet the County’s schedule. Additional credit will be given for the identification and planning for mitigation of schedule risks which Bidder believes may adversely affect any portion of the County’s schedule. 5 Points Relevant Experience: Proposals will be evaluated against the RFP specifications and the questions below: 1. Do the individuals assigned to the project have experience on similar projects? (3 Points) 2. Are résumés complete and do they demonstrate backgrounds that would be desirable for individuals 10 Points RFP No. 901004 Page 18 Specifications, Terms & Conditions for Behavioral Health Management Information System engaged in the work the project requires? (3 Points) 3. How extensive is the applicable education and experience of the personnel designated to work on the project? (4 Points) H. References (See Exhibit A – Bid Response Packet) If a short list process is used for a solicitation, references are only performed on the short list vendors and the score is not included in the preliminary short list score 5 Points I. Overall Proposal 5 Points J. Oral Presentation, Interview, and System Demonstration: Following evaluation of the written proposals, bidders receiving the highest scores may be invited to an oral presentation to demonstrate their system before a County Selection Committee and a group of end users. Bidders will be given from 9:00 a.m. to 4:00 p.m. to present their proposed system. K. L. System demonstration will be followed by an oral interview. The oral interview shall not exceed sixty (60) minutes in length. The oral interview will consist of standard questions asked of each of the bidders and specific questions regarding the specific proposed system. The proposals may then be re-evaluated and re-scored based on the oral presentation and interview. 15 Points Understanding of the Project: Proposals, including Exhibit C, will be evaluated against the RFP specifications and the questions below: 1. Has proposer demonstrated a thorough understanding of the purpose and scope of the project? (2 Points) 2. How well has the proposer identified pertinent issues and potential problems related to the project? (2 Points) 3. Has the proposer demonstrated that it understands the deliverables the County expects it to provide? (3 Points) 10 Points Methodology: Proposals, including Exhibit C, will be evaluated against the RFP specifications and the questions below: 1. Does the methodology depict a logical approach to fulfilling the requirements of the RFP? (2 Points) 2. Does the methodology match and contribute to achieving the objectives set out in the RFP? (1 Points) 5 Points RFP No. 901004 Page 19 Specifications, Terms & Conditions for Behavioral Health Management Information System 3. Does the methodology interface with the County’s time schedule? (2 Points) SMALL LOCAL EMERGING BUSINESS PREFERENCE I. Local Preference- Points equaling five percent (5%) of bidder’s total score, for the above Evaluation Criteria, will be added. This will be the bidder’s final score for purposes of award evaluation. Five Percent (5%) Small and Local or Emerging and Local Preference- Points equaling five percent (5%) of bidders total score, for the above Evaluation Criteria, will be added. This will be the bidder’s final score for purposes of award evaluation. Five Percent (5%) CONTRACT EVALUATION AND ASSESSMENT During the initial sixty (60) day period of any contract, which may be awarded to Contractor, the CSC and/or other persons designated by the County will meet with the Contractor to evaluate the equipment/system performance and to identify any issues or potential problems. The County reserves the right to determine, at its sole discretion, whether: 1. Contractor has complied with all terms of this RFP; and 2. Any problems or potential problems with the proposed equipment/system were evidenced which make it unlikely (even with possible modifications) that such proposed equipment/system have met the County requirements. If, as a result of such determination, the County concludes that it is not satisfied with Contractor, Contractor’s performance under any awarded contract and/or Contractor’s goods and/or services as contracted for therein, the Contractor will be notified of contract termination effective forty-five (45) days following notice. Contractor shall be responsible for the removal of equipment/system and shall return County facilities to their pre-installation state at no charge to the County. The County will have the right to invite the next highest ranked bidder to enter into a contract. The County also reserves the right to re-bid this project if it is determined to be in its best interest to do so. J. NOTICE OF INTENT TO AWARD 1. At the conclusion of the RFP response evaluation process (“Evaluation Process”), all bidders will be notified in writing by e-mail or fax, and certified mail, of the RFP No. 901004 Page 20 Specifications, Terms & Conditions for Behavioral Health Management Information System contract award recommendation, if any, by GSA – Purchasing. The document providing this notification is the Notice of Intent to Award. The Notice of Intent to Award will provide the following information: 2. 3. K. L. a. The name of the bidder being recommended for contract award; and b. The names of all other parties that submitted proposals. At the conclusion of the RFP process, debriefings for unsuccessful bidders will be scheduled and provided upon written request and will be restricted to discussion of the unsuccessful offeror’s bid. a. Under no circumstances will any discussion be conducted with regard to contract negotiations with the successful bidder. b. Debriefing may include review of successful bidder’s proposal with redactions as appropriate. The submitted proposals shall be made available upon request no later than five (5) business days before approval of the award and contract is scheduled to be heard by the Board of Supervisors. TERM / TERMINATION / RENEWAL 1. The term of the contract, which may be awarded pursuant to this RFP, will be three (3) years. 2. By mutual agreement, any contract which may be awarded pursuant to this RFP, may be extended for one additional two-year term at agreed prices with all other terms and conditions remaining the same. BRAND NAMES AND APPROVED EQUIVALENTS 1. Any references to manufacturers, trade names, brand names and/or catalog numbers are intended to be descriptive, but not restrictive, unless otherwise stated, and are intended to indicate the quality level desired. Bidders may offer any equivalent product that meets or exceeds the specifications. Bids based on equivalent products must: a. Clearly describe the alternate offered and indicate how it differs from the product specified; and, RFP No. 901004 Page 21 Specifications, Terms & Conditions for Behavioral Health Management Information System b. M. Include complete descriptive literature and/or specifications as proof that the proposed alternate will be equal to or better than the product named in this bid. 2. The County reserves the right to be the sole judge of what is equal and acceptable and may require Bidder to provide additional information and/or samples. 3. If Bidder does not specify otherwise, it is understood that the referenced brand will be supplied. QUANTITIES Quantities listed herein are estimates and are not to be construed as a commitment. No minimum or maximum is guaranteed or implied. N. PRICING 1. All pricing as quoted will remain firm for the term of any contract that may be awarded as a result of this RFP. 2. Unless otherwise stated, Bidder agrees that, in the event of a price decline, the benefit of such lower price shall be extended to the County. 3. All prices are to be F.O.B. destination. Any freight/delivery charges are to be included. 4. Any price increases or decreases for subsequent contract terms may be negotiated between Contractor and County only after completion of the initial term. 5. All prices quoted shall be in United States dollars and "whole cent," no cent fractions shall be used. There are no exceptions. 6. Price quotes shall include any and all payment incentives available to the County. 7. Bidders are advised that in the evaluation of cost, if applicable, it will be assumed that the unit price quoted is correct in the case of a discrepancy between the unit price and an extension. RFP No. 901004 Page 22 Specifications, Terms & Conditions for Behavioral Health Management Information System O. 8. Federal and State minimum wage laws apply. The County has no requirements for living wages. The County is not imposing any additional requirements regarding wages. 9. Prevailing Wages: Pursuant to Labor Code Sections 1770 et seq., Contractor shall pay to persons performing labor in and about Work provided for in Contract not less than the general prevailing rate of per diem wages for work of a similar character in the locality in which the Work is performed, and not less than the general prevailing rate of per diem wages for legal holiday and overtime work in said locality, which per diem wages shall not be less than the stipulated rates contained in a schedule thereof which has been ascertained and determined by the Director of the State Department of Industrial Relations to be the general prevailing rate of per diem wages for each craft or type of workman or mechanic needed to execute this contract. AWARD 1. Proposals will be evaluated by a committee and will be ranked in accordance with the RFP section entitled “Evaluation Criteria/Selection Committee.” 2. The committee will recommend award to the bidder who, in its opinion, has submitted the proposal that best serves the overall interests of the County and attains the highest overall point score. Award may not necessarily be made to the bidder with the lowest price. 3. Small and Emerging Locally Owned Business: The County is vitally interested in promoting the growth of small and emerging local businesses by means of increasing the participation of these businesses in the County’s purchase of goods and services. As a result of the County’s commitment to advance the economic opportunities of these businesses, Bidders must meet the County’s Small and Emerging Locally Owned Business requirements in order to be considered for the contract award. These requirements can be found online at: http://acgov.org/auditor/sleb/overview.htm For purposes of this bid, applicable industries include, but are not limited to, the following NAICS Code(s): 541511, 541512, and 541519 as having no more than $25,500,000 in average annual gross receipts over the last three (3) years. RFP No. 901004 Page 23 Specifications, Terms & Conditions for Behavioral Health Management Information System An emerging business, as defined by the County, is one that has less than onehalf (1/2) of the preceding amount and has been in business less than five (5) years. 4. The County reserves the right to reject any or all responses that materially differ from any terms contained in this RFP or from any Exhibits attached hereto, to waive informalities and minor irregularities in responses received, and to provide an opportunity for bidders to correct minor and immaterial errors contained in their submissions. The decision as to what constitutes a minor irregularity shall be made solely at the discretion of the County. 5. The County reserves the right to award to a single or multiple contractors. 6. The County has the right to decline to award this contract or any part thereof for any reason. 7. Board approval to award a contract is required. 8. A contract must be negotiated, finalized, and signed by the intended awardee prior to Board approval. 9. Final Standard Agreement terms and conditions will be negotiated with the selected bidder. Bidder may access a copy of the Standard Services Agreement template can be found online at: http://www.acgov.org/gsa/purchasing/standardServicesAgreement.pdf The template contains minimal Agreement boilerplate language only. 10. P. The RFP specifications, terms, conditions and Exhibits, RFP Addenda and Bidder’s proposal, may be incorporated into and made a part of any contract that may be awarded as a result of this RFP. METHOD OF ORDERING 1. A written PO and signed Standard Agreement contract will be issued upon Board approval. 2. POs and Standard Agreements will be faxed, transmitted electronically or mailed and shall be the only authorization for the Contractor to place an order. 3. POs and payments for products and/or services will be issued only in the name of Contractor. RFP No. 901004 Page 24 Specifications, Terms & Conditions for Behavioral Health Management Information System Q. 4. Contractor shall adapt to changes to the method of ordering procedures as required by the County during the term of the contract. 5. Change orders shall be agreed upon by Contractor and County and issued as needed in writing by County. WARRANTY 1. R. Bidder expressly warrants that all goods and services to be furnished pursuant to any contract awarded it arising from the Bid will conform to the descriptions and specifications contained herein and in supplier catalogs, product brochures and other representations, depictions or models, and will be free from defects, of merchantable quality, good material and workmanship. Bidder expressly warrants that all goods and services to be furnished pursuant to such award will be fit and sufficient for the purpose(s) intended. This warranty shall survive any inspections, delivery, acceptance or payment by the County. Bidder warrants that all work and services furnished hereunder shall be guaranteed for a period of 2 years from the date of acceptance by the County. INVOICING 1. Contractor shall invoice the requesting department, unless otherwise advised, upon satisfactory receipt of product and/or performance of services. 2. Payment will be made within thirty (30) days following receipt of invoice and upon complete satisfactory receipt of product and performance of services. 3. County shall notify Contractor of any adjustments required to invoice. 4. Invoices shall contain County PO number, invoice number, remit to address and itemized products and/or services description and price as quoted and shall be accompanied by acceptable proof of delivery. 5. Contractor shall utilize standardized invoice upon request. 6. Invoices shall only be issued by the Contractor who is awarded a contract. 7. Payments will be issued to and invoices must be received from the same Contractor whose name is specified on the POs. 8. The County will pay Contractor monthly or as agreed upon, not to exceed the total lump sum price quoted in the bid response. RFP No. 901004 Page 25 Specifications, Terms & Conditions for Behavioral Health Management Information System S. IV. ACCOUNT MANAGER / SUPPORT STAFF 1. Contractor shall provide a dedicated competent account manager who shall be responsible for the County account/contract. The account manager shall receive all orders from the County and shall be the primary contact for all issues regarding Bidder’s response to this RFP and any contract which may arise pursuant to this RFP. 2. Contractor shall also provide adequate, competent support staff that shall be able to service the County during normal working hours, Monday through Friday. Such representative(s) shall be knowledgeable about the contract, products offered and able to identify and resolve quickly any issues including but not limited to order and invoicing problems. 3. Contractor account manager shall be familiar with County requirements and standards and work with BHCS to ensure that established standards are adhered to. 4. Contractor account manager shall keep the County Specialist informed of requests from departments as required. INSTRUCTIONS TO BIDDERS T. COUNTY CONTACTS GSA–Purchasing is managing the competitive process for this project on behalf of the County. All contact during the competitive process is to be through the GSA–Purchasing Department only. The evaluation phase of the competitive process shall begin upon receipt of sealed bids until a contract has been awarded. Bidders shall not contact or lobby evaluators during the evaluation process. Attempts by Bidder to contact evaluators may result in disqualification of bidder. RFP No. 901004 Page 26 Specifications, Terms & Conditions for Behavioral Health Management Information System All questions regarding these specifications, terms and conditions are to be submitted in writing, preferably via e-mail by 5:00 p.m. on April 2, 2013 to: Ryan DeCoud, Contract Specialist I Alameda County, GSA–Purchasing 1401 Lakeside Drive, Suite 907 Oakland, CA 94612 E-Mail: ryan.decoud@acgov.org PHONE: (510) 208-9619 The GSA Contracting Opportunities website will be the official notification posting place of all Requests for Interest, Proposals, Quotes and Addenda. Go to http://www.acgov.org/gsa_app/gsa/purchasing/bid_content/contractopportunities.jsp to view current contracting opportunities. U. SUBMITTAL OF BIDS 1. All bids must be SEALED and must be received at the Office of the Purchasing Agent of Alameda County BY 2:00 p.m. on the due date specified in the Calendar of Events. NOTE: LATE AND/OR UNSEALED BIDS CANNOT BE ACCEPTED. IF HAND DELIVERING BIDS PLEASE ALLOW TIME FOR METERED STREET PARKING OR PARKING IN AREA PUBLIC PARKING LOTS AND ENTRY INTO SECURE BUILDING. Bids will be received only at the address shown below, and by the time indicated in the Calendar of Events. Any bid received after said time and/or date or at a place other than the stated address cannot be considered and will be returned to the bidder unopened. All bids, whether delivered by an employee of Bidder, U.S. Postal Service, courier or package delivery service, must be received and time stamped at the stated address prior to the time designated. The Purchasing Department's timestamp shall be considered the official timepiece for the purpose of establishing the actual receipt of bids. 2. Bids are to be addressed and delivered as follows: Behavioral Health Management Information System RFP No. 901004 Alameda County, GSA–Purchasing 1401 Lakeside Drive, Suite 907 * Oakland, CA 94612 RFP No. 901004 Page 27 Specifications, Terms & Conditions for Behavioral Health Management Information System Bidder's name, return address, and the RFP number and title must also appear on the mailing package. *PLEASE NOTE that on the bid due date, a bid reception desk will be open between 1:00 p.m. – 2:00 p.m. and will be located in the 1st floor lobby at 1401 Lakeside Drive. 3. Bidders are to submit one (1) original hardcopy bid (Exhibit A – Bid Response Packet, including additional required documentation), with original ink signatures, plus five (5) copies of their proposal. Original proposal is to be clearly marked “ORIGINAL” with copies to be marked “COPY”. All submittals should be printed on plain white paper, and must be either loose leaf or in a 3-ring binder (NOT bound). It is preferred that all proposals submitted shall be printed doublesided and on minimum 30% post-consumer recycled content paper. Inability to comply with the 30% post-consumer recycled content recommendation will have no impact on the evaluation and scoring of the proposal. Bidders must also submit an electronic copy of their proposal. The electronic copy must be in a single file (PDF with OCR preferred), and shall be an exact scanned image of the original hard copy Exhibit A – Bid Response Packet, including additional required documentation. The file must be on disk or USB flash drive and enclosed with the sealed original hardcopy of the bid. 4. BIDDERS SHALL NOT MODIFY BID FORM(S) OR QUALIFY THEIR BIDS. BIDDERS SHALL NOT SUBMIT TO THE COUNTY A SCANNED, RE-TYPED, WORDPROCESSED, OR OTHERWISE RECREATED VERSION OF THE BID FORM(S) OR ANY OTHER COUNTY-PROVIDED DOCUMENT. 5. No email (electronic) or facsimile bids will be considered. 6. All costs required for the preparation and submission of a bid shall be borne by Bidder. 7. Only one bid response will be accepted from any one person, partnership, corporation, or other entity; however, several alternatives may be included in one response. For purposes of this requirement, “partnership” shall mean, and is limited to, a legal partnership formed under one or more of the provisions of the California or other state’s Corporations Code or an equivalent statute. 8. Each bid received, with the name of the bidder, shall be entered on a record, and each record with the successful bid indicated thereon shall, after the award of the order or contract, be open to public inspection. RFP No. 901004 Page 28 Specifications, Terms & Conditions for Behavioral Health Management Information System V. 9. California Government Code Section 4552: In submitting a bid to a public purchasing body, the bidder offers and agrees that if the bid is accepted, it will assign to the purchasing body all rights, title, and interest in and to all causes of action it may have under Section 4 of the Clayton Act (15 U.S.C. Sec. 15) or under the Cartwright Act (Chapter 2, commencing with Section 16700, of Part 2 of Division 7 of the Business and Professions Code), arising from purchases of goods, materials, or services by the bidder for sale to the purchasing body pursuant to the bid. Such assignment shall be made and become effective at the time the purchasing body tenders final payment to the bidder. 10. Bidder expressly acknowledges that it is aware that if a false claim is knowingly submitted (as the terms “claim” and “knowingly” are defined in the California False Claims Act, Cal. Gov. Code, §12650 et seq.), County will be entitled to civil remedies set forth in the California False Claim Act. It may also be considered fraud and the Contractor may be subject to criminal prosecution. 11. The undersigned Bidder certifies that it is, at the time of bidding, and shall be throughout the period of the contract, licensed by the State of California to do the type of work required under the terms of the Contract Documents. Bidder further certifies that it is regularly engaged in the general class and type of work called for in the Bid Documents. 12. The undersigned Bidder certifies that it is not, at the time of bidding, on the California Department of General Services (DGS) list of persons determined to be engaged in investment activities in Iran or otherwise in violation of the Iran Contracting Act of 2010 (Public Contract Code Section 2200-2208). 13. It is understood that County reserves the right to reject this bid and that the bid shall remain open to acceptance and is irrevocable for a period of twelve (12) months, unless otherwise specified in the Bid Documents. RESPONSE FORMAT 1. Bid responses are to be straightforward, clear, concise and specific to the information requested. 2. In order for bids to be considered complete, Bidder must provide responses to all information requested. See Exhibit A – Bid Response Packet. 3. Bid responses, in whole or in part, are NOT to be marked confidential or proprietary. County may refuse to consider any bid response or part thereof so RFP No. 901004 Page 29 Specifications, Terms & Conditions for Behavioral Health Management Information System marked. Bid responses submitted in response to this RFP may be subject to public disclosure. County shall not be liable in any way for disclosure of any such records. Please refer to the County’s website at: http://www.acgov.org/gsa/departments/purchasing/policy/proprietary.htm for more information regarding Proprietary and Confidential Information policies. RFP No. 901004 Page 30 EXHIBIT A BID RESPONSE PACKET RFP No. 901004 – Behavioral Health Management Information System To: The County of Alameda From: (Official Name of Bidder) AS DESCRIBED IN THE SUBMITTAL OF BIDS SECTION OF THIS RFP, BIDDERS ARE TO SUBMIT ONE (1) ORIGINAL HARDCOPY BID (EXHIBIT A – BID RESPONSE PACKET), INCLUDING ADDITIONAL REQUIRED DOCUMENTATION), WITH ORIGINAL INK SIGNATURES, PLUS FIVE (5) COPIES AND ONE (1) ELECTRONIC COPY OF THE BID IN PDF (with OCR preferred) BIDDERS SHALL NOT MODIFY THIS BID RESPONSE PACKET IN ANY WAY OR QUALIFY THEIR BIDS BIDDERS SHALL NOT SUBMIT TO THE COUNTY A SCANNED, RE-TYPED, WORD-PROCESSED, OR OTHERWISE RECREATED VERSION OF EXHIBIT A – BID RESPONSE PACKET OR ANY OTHER COUNTY-PROVIDED DOCUMENT ALL PRICES AND NOTATIONS MUST BE PRINTED IN INK OR TYPEWRITTEN; NO ERASURES ARE PERMITTED; ERRORS MAY BE CROSSED OUT AND CORRECTIONS PRINTED IN INK OR TYPEWRITTEN ADJACENT, AND MUST BE INITIALED IN INK BY PERSON SIGNING BID BIDDER MUST QUOTE PRICE(S) AS SPECIFIED IN RFP BID RESPONSE PACKET (EXHIBIT A) MUST BE SUBMITTED IN TOTAL WITH ALL REQUIRED DOCUMENTS ATTACHED THERETO; ALL INFORMATION REQUESTED MUST BE SUPPLIED BIDDERS THAT DO NOT COMPLY WITH THE REQUIREMENTS, AND/OR SUBMIT INCOMPLETE BID PACKAGES, SHALL BE SUBJECT TO DISQUALIFICATION AND THEIR BIDS REJECTED IN TOTAL IF BIDDERS ARE MAKING ANY CLARIFICATIONS AND/OR AMENDMENTS, OR TAKING EXCEPTION TO POLICIES OR SPECIFICATIONS OF THIS RFP, INCLUDING THOSE TO THE COUNTY SLEB POLICY, THESE MUST BE SUBMITTED IN THE EXCEPTIONS, CLARIFICATIONS, AMENDMENTS SECTION OF THIS EXHIBIT A – BID RESPONSE PACKET IN ORDER FOR THE BID RESPONSE TO BE CONSIDERED COMPLETE BIDDER INFORMATION AND ACCEPTANCE Exhibit A – RFP No. 901004 Page 1 1. The undersigned declares that the Bid Documents, including, without limitation, the RFP, Addenda, and Exhibits have been read. 2. The undersigned is authorized, offers, and agrees to furnish the articles and/or services specified in accordance with the Specifications, Terms & Conditions of the Bid Documents of RFP No. 901004 – Behavioral Health Management Information. 3. The undersigned has reviewed the Bid Documents and fully understands the requirements in this Bid including, but not limited to, the requirements under the County Provisions, and that each Bidder who is awarded a contract shall be, in fact, a prime contractor, not a subcontractor, to County, and agrees that its Bid, if accepted by County, will be the basis for the Bidder to enter into a contract with County in accordance with the intent of the Bid Documents. 4. The undersigned acknowledges receipt and acceptance of all addenda. 5. The undersigned agrees to the following terms, conditions, certifications, and requirements found on the County’s website: 6. Bid Protests / Appeals Process [http://www.acgov.org/gsa/departments/purchasing/policy/bidappeal.htm] Debarment / Suspension Policy [http://www.acgov.org/gsa/departments/purchasing/policy/debar.htm] Iran Contracting Act (ICA) of 2010 [http://www.acgov.org/gsa/departments/purchasing/policy/ica.htm] General Environmental Requirements [http://www.acgov.org/gsa/departments/purchasing/policy/environ.htm] Small Local Emerging Business Program [http://acgov.org/auditor/sleb/overview.htm] First Source [http://acgov.org/auditor/sleb/sourceprogram.htm] Online Contract Compliance System [http://acgov.org/auditor/sleb/elation.htm] General Requirements [http://www.acgov.org/gsa/departments/purchasing/policy/genreqs.htm] Proprietary and Confidential Information [http://www.acgov.org/gsa/departments/purchasing/policy/proprietary.htm] The undersigned acknowledges that Bidder will be in good standing in the State of California, with all the necessary licenses, permits, certifications, approvals, and authorizations necessary to perform all obligations in connection with this RFP and associated Bid Documents. Exhibit A – RFP No. 901004 Page 2 7. It is the responsibility of each bidder to be familiar with all of the specifications, terms and conditions and, if applicable, the site condition. By the submission of a Bid, the Bidder certifies that if awarded a contract they will make no claim against the County based upon ignorance of conditions or misunderstanding of the specifications. 8. Patent indemnity: Vendors who do business with the County shall hold the County of Alameda, its officers, agents and employees, harmless from liability of an nature or kind, including cost and expenses, for infringement or use of any patent, copyright or other proprietary right, secret process, patented or unpatented invention, article or appliance furnished or used in connection with the contract or purchase order. 9. Insurance certificates are not required at the time of submission. However, by signing Exhibit A – Bid Response Packet, the contractor agrees to meet the minimum insurance requirements stated in the RFP. This documentation must be provided to the County, prior to award, and shall include an insurance certificate and additional insured certificate, naming the County of Alameda, which meets the minimum insurance requirements, as stated in the RFP. 10. The undersigned acknowledges ONE of the following (please check only one box): Bidder is not local to Alameda County and is ineligible for any bid preference; OR Bidder is a certified SLEB and is requesting 10% bid preference (Bidder must check the first box in SLEB PARTNERING INFORMATION SHEET and provide its SLEB Certification Number); OR Bidder is LOCAL to Alameda County and is requesting 5% bid preference, and has attached the following documentation to this Exhibit: Copy of a verifiable business license, issued by the County of Alameda or a City within the County; and Proof of six (6) months business residency, identifying the name of the vendor and the local address. Utility bills, deed of trusts or lease agreements, etc., are acceptable verification documents to prove residency. Exhibit A – RFP No. 901004 Page 3 Official Name of Bidder: Street Address Line 1: Street Address Line 2: City: State: Zip Code: Webpage: Type of Entity / Organizational Structure (check one): Corporation Joint Venture Limited Liability Partnership Partnership Limited Liability Corporation Non-Profit / Church Other: Jurisdiction of Organization Structure: Date of Organization Structure: Federal Tax Identification Number: Primary Contact Information: Name / Title: Telephone Number: Fax Number: E-mail Address: SIGNATURE: Name and Title of Signer: Dated this day of 20 Exhibit A – RFP No. 901004 Page 4 BID FORM(S) Cost shall be submitted on Exhibit B as is. No alterations or changes of any kind are permitted. Bid responses that do not comply will be subject to rejection in total. The cost quoted below shall include all taxes and all other charges, including travel expenses, and is the cost the County will pay for the three-year term of any contract that is a result of this bid. Quantities listed herein are annual estimates based on past usage and are not to be construed as a commitment. No minimum or maximum is guaranteed or implied. Bidder hereby certifies to County that all representations, certifications, and statements made by Bidder, as set forth in this Bid Form and attachments are true and correct and are made under penalty of perjury pursuant to the laws of California. Year 1 DESCRIPTION SOFTWARE Software shall include support for the following: Practice Management Electronic Clinical Records Call Management, Managed care Eligibility Verification Claims Processing Coordination of Benefits (COB)/Third Party Liability (TPL) Financial Reporting, Electronic Prescriptions Data Warehouse Security Report Writing (C) Unit Cost (D) Extended Cost Year 2 (A) Unit of Measure (B) Quantity Each Each Each Each Each Each 1 1 1 1 1 1 $ $ $ $ $ $ $ $ $ $ $ $ $ $ $ $ $ $ Each 1 $ $ $ Each Each Each Each Each 1 1 1 1 1 $ $ $ $ $ $ $ $ $ $ $ $ $ $ $ Subtotal (E) Unit Cost (F) Extended Cost Year 3 (G) Unit Cost (H) Extended Cost Total Cost D+F+H $ HARDWARE - As Required to Implement Software: Additional Hardware can be listed on a separate page. Exhibit A – RFP No. 901004 Page 5 Year 1 (A) Unit of Measure (B) Quantity Each 1 Each 1 Each 1 Each 1 Each 1 Each 1 Each 1 Each 1 Each 1 Implementation Consulting Per Hour 1040 Software Setup / Installation Per Hour 2080 Project Management Per Hour 2080 Integration with Current System Per Hour 2080 Testing Per Hour 160 Training Per Hour 1040 Yearly 1 Per Hour 1040 Yearly 1 DESCRIPTION (C) Unit Cost $ $ $ $ $ $ $ $ $ Year 2 (D) Extended Cost $ $ $ $ $ $ $ $ $ (E) Unit Cost Year 3 (F) Extended Cost (G) Unit Cost (H) Extended Cost Total Cost D+F+H $ $ $ $ $ $ $ $ $ Subtotal IMPLEMENTATION SETUP $ $ $ $ $ $ $ $ $ $ $ $ $ $ $ $ $ $ Subtotal Other Services Licensing Technical Support Extended Warranty $ $ $ $ $ $ $ $ $ $ $ $ $ $ $ $ $ Total Cost of Additional Hardware from Bid Form, Page 7 Tax TOTAL 3 YEAR COST: $ $ Bidder agrees that the price(s) quoted are firm during the term of any contract awarded FIRM: _________________________SIGNATURE:______________________DATE:_______________________ PRINTED NAME: __________________________________TITLE:______________________________________ Exhibit A – RFP No. 901004 Page 6 BID FORM(S) COUNTY OF ALAMEDA RFP No.901004 Additional Hardware Hardware Unit of Measure Quantity Each Each Each Each Each Each Each Each Each Each Each 1 1 1 1 1 1 1 1 1 1 1 Unit Cost $ $ $ $ $ $ $ $ $ $ $ Extended Cost $ $ $ $ $ $ $ $ $ $ $ Total Cost for Additional Hardware: $ Bidder agrees that the price(s) quoted are firm during the term of any contract awarded FIRM: _________________________SIGNATURE:______________________DATE:___________ PRINTED NAME: __________________________________TITLE:__________________________ Exhibit A – RFP No. 901004 Page 7 REQUIRED DOCUMENTATION AND SUBMITTALS All of the specific documentation listed below is required to be submitted with the Exhibit A – Bid Response Packet in order for a bid to be deemed complete. Bidders shall submit all documentation, in the order listed below and clearly label each section with the appropriate title (i.e. Table of Contents, Letter of Transmittal, Key Personnel, etc.). 1. Table of Contents: Bid responses shall include a table of contents listing the individual sections of the proposal and their corresponding page numbers. Tabs should separate each of the individual sections. 2. Letter of Transmittal: Bid responses shall include a description of Bidder’s capabilities and approach in providing its goods and/or services to the County, and provide a brief synopsis of the highlights of the Proposal and overall benefits of the Proposal to the County. This synopsis should not exceed three (3) pages in length and should be easily understood. 3. Key Personnel: Bid responses shall include a complete list of all key personnel associated with the RFP. This list must include all key personnel who will provide services/training to County staff and all key personnel who will provide maintenance and support services. For each person on the list, the following information shall be included: (a) (b) (c) (d) (e) The person’s relationship with Bidder, including job title and years of employment with Bidder; The role that the person will play in connection with the RFP; Address, telephone, fax numbers, and e-mail address; Person’s educational background; and Person’s relevant experience, certifications, and/or merits. 4. Description of the Proposed Equipment/System: Bid response shall include a description of the proposed equipment/system, as it will be finally configured during the term of the contract. The description shall specify how the proposed equipment/system will meet or exceed the requirements of the County and shall explain any advantages that this proposed equipment/system would have over other possible equipment/systems. The description shall include any disadvantages or limitations that the County should be aware of in evaluating the proposal/quotation. Finally, the description shall describe all product warranties provided by Bidder. Proposals must contain a narrative and a completed Exhibit C. 5. Implementation Plan and Schedule: Bid responses shall include an implementation plan and schedule that includes the bidders process / timeframe for the implementation of the new Behavioral Health Management Information System. 6. Description of the Proposed Services: Bid response shall include a description of the terms and conditions of services to be provided during the contract term including response times. The description shall contain a basis of estimate for services including its scheduled start and Exhibit A – RFP No. 901004 Page 8 completion dates, the number of Bidder’s and County personnel involved, and the number of hours scheduled for such personnel. Finally, the description must: (1) specify how the services in the bid response will meet or exceed the requirements of the County; (2) explain any special resources, procedures or approaches that make the services of Bidder particularly advantageous to the County; and (3) identify any limitations or restrictions of Bidder in providing the services that the County should be aware of in evaluating its Response to this RFP. 7. References: (a) (b) (c) 8. Exceptions, Clarifications, Amendments: (a) (b) 9. Bidders must use the templates on pages 12 - 13 of this Exhibit A – Bid Response Packet to provide references. Bidders are to provide a list of five (5) current and (5) former clients. References must be satisfactory as deemed solely by County. References should have similar scope, volume and requirements to those outlined in these specifications, terms and conditions. Bidders must verify the contact information for all references provided is current and valid. Bidders are strongly encouraged to notify all references that the County may be contacting them to obtain a reference. The County may contact some or all of the references provided in order to determine Bidder’s performance record on work similar to that described in this request. The County reserves the right to contact references other than those provided in the Response and to use the information gained from them in the evaluation process. This shall include clarifications, exceptions and amendments, if any, to the RFP and associated Bid Documents, and shall be submitted with your bid response using the template on page 13 of this Exhibit A – Bid Response Packet. THE COUNTY IS UNDER NO OBLIGATION TO ACCEPT ANY EXCEPTIONS, AND SUCH EXCEPTIONS MAY BE A BASIS FOR BID DISQUALIFICATION. SLEB Partnering Information Sheet: (a) Every bidder must fill out and submit a signed SLEB Partnering Information Sheet, (found in Exhibit A immediately following this paragraph) indicating their SLEB certification status and, if not certified, the name, identification information, and goods/services to be provided by the SLEB partner(s) with whom the bidder will subcontract to meet the County SLEB participation requirement. If a SLEB subcontractor(s) is named, the Exhibit must be signed by the SLEB(s) according to the instructions. Exhibit A – RFP No. 901004 Page 9 SMALL LOCAL EMERGING BUSINESS (SLEB) PARTNERING INFORMATION SHEET RFP No. 901004 – Behavioral Health Management Information System In order to meet the Small Local Emerging Business (SLEB) requirements of this RFP, all bidders must complete this form as required below. Bidders not meeting the definition of a SLEB (http://acgov.org/auditor/sleb/overview.htm) are required to subcontract with a SLEB for at least twenty percent (20%) of the total estimated bid amount in order to be considered for contract award. SLEB subcontractors must be independently owned and operated from the prime contractor with no employees of either entity working for the other. This form must be submitted for each business that bidders will work with, as evidence of a firm contractual commitment to meeting the SLEB participation goal. (Copy this form as needed.) Bidders are encouraged to form a partnership with a SLEB that can participate directly with this contract. One of the benefits of the partnership will be economic, but this partnership will also assist the SLEB to grow and build the capacity to eventually bid as a prime on their own. Once a contract has been awarded, bidders will not be able to substitute named subcontractors without prior written approval from the Auditor-Controller, Office of Contract Compliance (OCC). County departments and the OCC will use the web-based Elation Systems to monitor contract compliance with the SLEB program (Elation Systems: http://www.elationsys.com/elationsys/index.htm). BIDDER IS A CERTIFIED SLEB (sign at bottom of page) SLEB BIDDER Business Name: SLEB Certification #: SLEB Certification Expiration Date: NAICS Codes Included in Certification: BIDDER IS NOT A CERTIFIED SLEB AND WILL SUBCONTRACT GOODS/SERVICES: % WITH THE SLEB NAMED BELOW FOR THE FOLLOWING SLEB BIDDER Business Name: SLEB Certification #: SLEB Certification Status: SLEB Certification Expiration Date: Small / Emerging NAICS Codes Included in Certification: SLEB Subcontractor Principal Name: SLEB Subcontractor Principal Signature: Date: Upon award, prime contractor and all SLEB subcontractors that receive contracts as a result of this bid process agree to register and use the secure web-based ELATION SYSTEMS. ELATION SYSTEMS will be used to submit SLEB subcontractor participation including, but not limited to, subcontractor contract amounts, payments made, and confirmation of payments received. Bidder Signature: Date: Exhibit A – RFP No. 901004 Page 10 CURRENT REFERENCES RFP No. 901004 – Behavioral Health Management Information System Bidder Name: Company Name: Address: City, State, Zip: Contact Person: Telephone Number: E-mail Address: Services Provided / Date(s) of Service: Company Name: Address: City, State, Zip: Services Provided / Date(s) of Service: Contact Person: Telephone Number: E-mail Address: Company Name: Address: Contact Person: Telephone Number: City, State, Zip: Services Provided / Date(s) of Service: E-mail Address: Company Name: Address: City, State, Zip: Services Provided / Date(s) of Service: Contact Person: Telephone Number: E-mail Address: Company Name: Address: Contact Person: Telephone Number: City, State, Zip: Services Provided / Date(s) of Service: E-mail Address: Exhibit A – RFP No. 901004 Page 11 FORMER REFERENCES RFP No. 901004 – Behavioral Health Management Information System Bidder Name: Company Name: Address: Contact Person: Telephone Number: City, State, Zip: Services Provided / Date(s) of Service: E-mail Address: Company Name: Address: City, State, Zip: Services Provided / Date(s) of Service: Contact Person: Telephone Number: E-mail Address: Company Name: Address: City, State, Zip: Services Provided / Date(s) of Service: Contact Person: Telephone Number: E-mail Address: Company Name: Address: City, State, Zip: Services Provided / Date(s) of Service: Contact Person: Telephone Number: E-mail Address: Company Name: Address: City, State, Zip: Services Provided / Date(s) of Service: Contact Person: Telephone Number: E-mail Address: Exhibit A – RFP No. 901004 Page 12 EXCEPTIONS, CLARIFICATIONS, AMENDMENTS RFP No. 901004 – Behavioral Health Management Information System Bidder Name: List below requests for clarifications, exceptions and amendments, if any, to the RFP and associated Bid Documents, and submit with your bid response. The County is under no obligation to accept any exceptions and such exceptions may be a basis for bid disqualification. Reference to: Description Page No. Section Item No. p. 23 D 1.c. Vendor takes exception to… *Print additional pages as necessary Exhibit A – RFP No. 901004 Page 13 EXHIBIT B INSURANCE REQUIREMENTS Insurance certificates are not required at the time of submission; however, by signing Exhibit A – Bid Packet, the bidder agrees to meet the minimum insurance requirements stated in the RFP, prior to award. This documentation must be provided to the County, prior to award, and shall include an insurance certificate and additional insured certificate, naming the County of Alameda, which meets the minimum insurance requirements, as stated in this Exhibit B – Insurance Requirements. The following are the minimum insurance limits, required by the County of Alameda, to be held by the contractor performing on this RFP: *** see next page for County of Alameda minimum insurance requirements *** Exhibit B – RFP No. 901004 Page 1 EXHIBIT B COUNTY OF ALAMEDA MINIMUM INSURANCE REQUIREMENTS Without limiting any other obligation or liability under this Agreement, the Contractor, at its sole cost and expense, shall secure and keep in force during the entire term of the Agreement or longer, as may be specified below, the following insurance coverage, limits and endorsements: TYPE OF INSURANCE COVERAGES MINIMUM LIMITS A Commercial General Liability $1,000,000 per occurrence (CSL) Premises Liability; Products and Completed Operations; Contractual Bodily Injury and Property Damage Liability; Personal Injury and Advertising Liability; Abuse, Molestation, Sexual Actions, and Assault and Battery B Commercial or Business Automobile Liability $1,000,000 per occurrence (CSL) All owned vehicles, hired or leased vehicles, non-owned, borrowed and Any Auto permissive uses. Personal Automobile Liability is acceptable for individual Bodily Injury and Property Damage contractors with no transportation or hauling related activities C Workers’ Compensation (WC) and Employers Liability (EL) WC: Statutory Limits Required for all contractors with employees EL: $100,000 per accident for bodily injury or disease D Professional Liability/Errors & Omissions $1,000,000 per occurrence Includes endorsements of contractual liability and defense and $2,000,000 project aggregate indemnification of the County E Endorsements and Conditions: 1. ADDITIONAL INSURED: ALL INSURANCE REQUIRED ABOVE WITH THE EXCEPTION OF PROFESSIONAL LIABILITY, PERSONAL AUTOMOBILE LIABILITY, WORKERS’ COMPENSATION AND EMPLOYERS LIABILITY, SHALL PROVIDE AN ADDITIONAL INSURANCE ENDORSEMENT PAGE THAT NAMES AS ADDITIONAL INSURED: COUNTY OF ALAMEDA, ITS BOARD OF SUPERVISORS, THE INDIVIDUAL MEMBERS THEREOF, AND ALL COUNTY OFFICERS, AGENTS, EMPLOYEES AND REPRESENTATIVES. 2. DURATION OF COVERAGE: All required insurance shall be maintained during the entire term of the Agreement with the following exception: Insurance policies and coverage(s) written on a claims-made basis shall be maintained during the entire term of the Agreement and until 3 years following termination and acceptance of all work provided under the Agreement, with the retroactive date of said insurance (as may be applicable) concurrent with the commencement of activities pursuant to this Agreement. 3. REDUCTION OR LIMIT OF OBLIGATION: All insurance policies shall be primary insurance to any insurance available to the Indemnified Parties and Additional Insured(s). Pursuant to the provisions of this Agreement, insurance affected or procured by the Contractor shall not reduce or limit Contractor’s contractual obligation to indemnify and defend the Indemnified Parties. 4. INSURER FINANCIAL RATING: Insurance shall be maintained through an insurer with a minimum A.M. Best Rating of A- or better, with deductible amounts acceptable to the County. Acceptance of Contractor’s insurance by County shall not relieve or decrease the liability of Contractor hereunder. Any deductible or self-insured retention amount or other similar obligation under the policies shall be the sole responsibility of the Contractor. 5. SUBCONTRACTORS: Contractor shall include all subcontractors as an insured (covered party) under its policies or shall maintain separate certificates and endorsements for each subcontractor. All coverage’s for subcontractors shall be subject to all of the requirements stated herein. 6. JOINT VENTURES: If Contractor is an association, partnership or other joint business venture, required insurance shall be provided by any one of the following methods: – Separate insurance policies issued for each individual entity, with each entity included as a “Named Insured (covered party), or at minimum named as an “Additional Insured” on the other’s policies. – Joint insurance program with the association, partnership or other joint business venture included as a “Named Insured. 7. CANCELLATION OF INSURANCE: All required insurance shall be endorsed to provide thirty (30) days advance written notice to the County of cancellation. 8. CERTIFICATE OF INSURANCE: Before commencing operations under this Agreement, Contractor shall provide Certificate(s) of Insurance and applicable insurance endorsements, in form and satisfactory to County, evidencing that all required insurance coverage is in effect. The County reserves the rights to require the Contractor to provide complete, certified copies of all required insurance policies. The require certificate(s) and endorsements must be sent to: - Department/Agency issuing the contract Certificate C-2C Page 1 of 1 Form 2003-1 (Rev. 3/31/10) Exhibit B – RFP No. 901004 Page 2 EXHIBIT C FUNCTIONAL & TECHNICAL REQUIREMENTS DETAIL RFP NO. 901004 – BEHAVIORAL HEALTH MANAGEMENT INFORMATION SYSTEM VENDORS MUST INDICATE WHETHER THEIR SOLUTION SUPPORTS THE FOLLOWING FUNCTIONAL AREAS. FUCTIONAL REQUIREMENTS A=Currently Available B=In Development (within 6 month) C=Available but Requires User/Client Modification D=Available via Vendor Modification E=Available Through Third Party Software F=Not Available A 1. Appointment Scheduling Requirements: 1. “Appointment Scheduling” shall have the ability to: (a) Provide on-line scheduling of appointments for client services; (b) Enter the following information in the appointment screen: i. Client name, language(s) spoken, and phone number ii. Medical Record Number/Client Number(s) (multiple numbers); iii. Funding source/Insurance (multiple sources); iv. Presenting problem; and symptoms v. Referral source; vi. Authorization number; vii. Method for client to receive reminders (email, text, phone) and opt-out option; viii. New variables as required. (c) Schedule recurring services for a client with one entry; (d) Schedule clinicians, therapists and other direct service providers; Schedule sites and/or equipment; (e) Schedule out of the office activities; (f) Schedule add-in clients (i.e. Add client to schedule without time slot); (g) Schedule more than one client at a time (i.e., dual or group sessions); (h) Double-book clients, clinicians, staff, and resources; B C D E F Comments f Exhibit C – RFP No. 901004 Page 1 A B C D E F Comments (i) 2. 3. 4. Schedule new clients with incomplete client demographic information; (j) Cancel or change an appointment, and record reason; (k) Reschedule appointments without having to re-enter data; (l) Track and manages schedule changes; (m) Reassign appointments to another clinician; (n) Schedule multiple services for a client to be performed at multiple sites (o) Schedule two or more resources simultaneously; (p) Automatically record identity of person entering appointment information; and (q) Color code appointment slots. “Appointment Display/Search” shall have the ability to: (a) Provide on-line graphic displays of schedules and available slots; (b) Display more than one day's schedule and more than one clinic's schedule at a time; (c) Display client’s appointment history and print it; and (d) Automatically find available appointment slot for a client by day of week; time of day; length of appointment; clinician; type of appointment; office or location; and funding source. “Appointment Templates” shall have the ability to: (a) Create individualized templates by provider/resource/site; (b) Allow scheduling template changes for a defined time period in the future without requiring manual cancellation of existing appointments; (c) Support patterns of physician schedules that may be used either continuously or by specifying day of the week; (d) Perform wave scheduling (i.e., set up appointments by type in time slots); (e) Schedule blocks of time for specific procedures or services; (f) Schedule blocks of times for clinicians; and (g) Define the double booking or overbooking limits. “Appointment Check-In” shall have the ability to: (a) Indicate a client has appeared for their appointment; (b) Automatically notify clinician that client has checked-in for their appointment; (c) Indicate that a client was a "walk-in;" (d) Assign a tracking number for all clients appearing, including walk-ins, (e) Reconcile check-ins with service capture and charge entry; Exhibit C – RFP No. 901004 Page 2 A 5. 2. B C D E F Comments and (f) Monitor clients within clinic after check in. “Appointment Wait List Management” shall have the ability to: (a) Maintain a wait list; (b) Provide an on-line data entry screen with user-defined fields for wait list; (c) Update wait list information as client circumstances change; and (d) Generate Waiting Lists containing the following client information: i. Date and time of entry; ii. Referral type; iii. Reason for wait list; iv. Priority; v. Expected appointment date; vi. Program or benefit information; and vii. User-defined fields. Authorization Requirements: 1. “Creation and Receipt of Service Authorizations” shall have the ability to: (a) Create service authorization requests for the following types of services: i. Inpatient (Treatment Authorization Request); Residential; ii. Emergency services; Outpatient services (RES/RCR's & CQRT); and iii. Wrap around services. (b) Add new types of service authorizations as necessary; (c) Accept, capture, store and generate a Referral Certification and Authorization transaction, using standard data protocol; (d) 2. Create authorization requests through a secure web-based portal; (e) Receive and generate electronic signatures to/from a third party ; (f) Automatically detects potential duplicate authorization requests upon entry, and can generate alerts; and (g) Review and override authorization status. “Processing of Service Authorizations” shall have the ability to: Exhibit C – RFP No. 901004 Page 3 A (a) (b) (c) (d) (e) (f) (g) (h) (i) (j) (k) (l) (m) (n) (o) (p) iv. (q) B C D E F Comments Create and attach a user-defined status indicator to a service authorization; Approve, deny or defer a service authorization request; Automatically generate Notice of Action letters with userdefined responses for electronic or hard copy transmission; Track Notice of Action letters sent, by querying the system by sent date, provider, reason for system audit; Track the status of a service authorization request as authorized, denied, or pending (including reason); Provide workflow-related rules to direct the flow of service authorizations, and ability to override (based on security); Provide unlimited authorization level notes with date stamp and time stamp, with ability to insert initials/name of reviewer; notes can be from self-created notes libraries; Provide role-based access capability for notes, status determination and opening and closing of service authorization requests; Provide ability to retain history of authorization notes; Provide capability to verify authorized services against benefit plan and accumulators before approving; Allow authorization module to interface with client master file; Allow authorization module to interface with provider master file; Provide automatic verification of client eligibility at time of authorization request entry, with ability to authorize even when eligibility cannot be verified; Automatically verifies provider contract status at time of authorization request entry; Offer different authorization screen formats based on type of service (e.g., inpatient, outpatient); Automatically inactivate authorizations: i. After a user-defined period of time without receipt of claims; ii. Upon termination of eligibility; iii. When referral provider terminates contract; and The ability to manually override any of the above automated processes. Create alerts when eligibility terminates or changes; Exhibit C – RFP No. 901004 Page 4 A B C D E F Comments (r) 3. 4. Authorized services can be stipulated by: i. Procedure code groupings; ii. HCPCS groupings; iii. ICD-9, ICD10, DSM-IV or DSM-V codes; iv. Provider; v. Provider taxonomy; and vi. Place of service. (s) Create a single authorization letter for multiple procedure codes (for client and provider respectively); (t) Provide linkage to clinical protocols to review guidelines and alternatives prior to authorizing specific procedures for a given diagnosis or condition; (u) Set and track limits on authorization based on any or all of the following data elements: i. Number of visits; ii. Units of service; iii. Level of service codes; iv. Date parameters; v. Cost (dollars); and vi. User defined elements. (v) Interface with claims adjudication module to update authorization usage; (w) Automatically sets authorization status to closed when all services have been claimed and claims have been adjudicated; and (x) Link authorizations for an individual client. “FFS Inpatient” shall have the ability: (a) Generate authorizations and authorization data that meets the State Treatment Authorization Request (TAR) specifications; (b) Submit approved TARs to the State fiscal intermediary electronically; (c) Generate a State TAR Update Transmittal (TUT) form; (d) Set field indicators for medical necessity reviews and decisions; and (e) Enter State TAR appeal level information. “Reporting” shall have the ability: (a) Provide reporting capability to capture statistics for: i. Submissions; ii. Approvals; iii. Denials; Exhibit C – RFP No. 901004 Page 5 A B C D E F Comments iv. v. vi. (b) Provider type; Age of Authorization; and Other. Produce the following reports: i. Authorization turnaround reports; ii. Authorization productivity reports by authorizing user; iii. Trending of authorizations by: a. b. c. d. e. 3. Referring provider; Referred to provider; Referred to provider specialty; Status (Approved / denied / pending); and Combinations of the above. Benefits/Insurance Requirements: 1. “Benefit Structure & Administration” shall have the ability to: (a) Provide a structured and automatically guided function for building benefit plans, benefit levels and financial risk levels; (b) Guided benefit function that provides: i. Copy and edit features; ii. Start dates and termination dates by plan and plan component, with the capacity to store historical information; and iii. Identifies start date and termination date by component. (c) Provide for the inclusion of detailed benefit text accessible from all modules; (d) Allow inquiry access to detailed benefits including, but not limited to, co-pays, coinsurance, exclusions, maximums, carve-out services and notes; (e) Support definition of benefits at a code specific level including groupings of CPT/HCPCs codes (i.e. individual codes, modifiers and ranges of codes); (f) Support the same definition groupings from benefits to be shared in defining authorization, provider contract and claims payment rules; (g) Support varying benefit parameters (e.g., co-payments, Exhibit C – RFP No. 901004 Page 6 A 2. B C D E F Comments limits, exclusions) including: i. Place of service (inpatient, outpatient, home, etc.); ii. Type of Bill (UB04 facility claims/billings); iii. Provider type code; iv. Procedure codes, code ranges and categories; v. Procedure code modifier; vi. Diagnosis code, code ranges and categories; vii. Age/gender restrictions; viii. In-network/out-of-network; ix. Referral requirements; x. Prior authorization requirements; xi. Type of service; xii. Emergency/Urgent/Elective status; xiii. User defined field; and xiv. Any combination of the above. (h) Support the following calculation/measurement stipulations for all benefit parameters including: i. Co-payment/coinsurance; ii. Flat amount; iii. Percent of billed charges; iv. Out-of-pocket stop-loss/out of pocket maximums; v. Per individual; vi. Per family; vii. Percent of Fee Schedule (i.e. RBRVS); viii. Medi-Cal Share of Cost; ix. Per Diem; and x. Benefit periods, including capacity to store historical data. (i) Set/define logic when multiple benefit rules/stipulations overlap such as when two or more rules apply (e.g., apply deductible then calculate co-pay on the balance); (j) Identify time frames associated with benefit limits (10 visits per year); (k) Full integration of benefit logic and adjudication with utilization and claims modules; and (l) Provide benefit summary grids lookup for users. “Eligibility Management” shall have the ability to: (a) Support assignment of a unique client number for individual; (b) Allow a client to retain this unique identification number if they move among payers; Exhibit C – RFP No. 901004 Page 7 A B C D E F Comments (c) 3. 4. Support additional identification numbers including: i. CIN numbers; ii. Beneficiary IDs; iii. Medicare IDs; iv. Social security numbers; v. Family ID; vi. Medi-Cal ID; and vii. User defined IDs. (d) Allow sorting and selecting by user-defined fields; (e) Allow re-labeling of user-defined fields; (f) Maintain historical values/information; (g) Support capture and maintenance of COB information; (h) Support free-text notes; (i) Provide secured access to notes varying by note type; (j) Date/time stamp notes and include user ID/Name; (k) Support client searching/inquiry by all of the above identification numbers; (l) Provide access to the following additional client data from all of the above functions: i. Benefit accumulators; and ii. Case Manager assignments (including history). (m) Support linking of individuals to a family/head of household account/record; (n) Allow data changes made at the subscriber/head of household level to be reflected in dependent records; (o) Support full integration with correspondence module; (p) Provide audit trail of all eligibility updates indicating which are user versus system generated; and (q) Maintain a full history of all user/system changes. “Financial Screening / California UMDAP” that: (a) Supports on-line, real-time financial assessment feature, for gathering and determining financial responsibility; (b) UMDAP - Supports flexibility in defining the benefit period: ability to check service activity, and allow adjustment of the date to be based on service activity; (c) Provides annual tickler for required UMDAP redetermination; and (d) Supports the ability for the financial assessment process to produce printed forms to be given to clients at the conclusion of the financial assessment. “Eligibility Loading” that: Exhibit C – RFP No. 901004 Page 8 A B C D E F Comments (a) 5. Supports monthly loading of the Medi-Cal Eligibility Determination System (MEDS) files from the state; (b) Assures that all eligible enrollees have a new record added to the county system for Medi-Cal eligibility each month, including all retroactive additions to Medi-Cal; (c) Alerts staff of retroactive additions and removals that may have an impact on claims; (d) Maintains eligibility records for all county eligible in the state monthly download file, not just individuals who are enrolled as clients; (e) Supports eligibility loading, processing and automatic update capabilities for Medicare; (f) Supports eligibility loading, processing and automatic update capabilities for other insurance companies and health plans; (g) Supports adhoc loading of eligibility records, directly into the primary database; (h) Supports batch processing to the MEDS system (270/271 transaction); (i) Supports the OHC (Other Health Coverage) file upload requirement; and (j) Allows for the entry of one or more third party payor(s) name. “Eligibility Verification” that: (a) Provides for eligibility of registered clients to be evaluated against the downloaded eligibility files and updated as necessary based on a matching algorithm; (b) Supports a real-time interface to the Medi-Cal Point of Service AEVS database for viewing a client’s current eligibility status for Medi-Cal and other healthcare coverage information; (c) Supports review and update of client records for special handling conditions including: i. Partial eligibility match requiring investigation; ii. Medi-Cal Share of Cost; includes ability to include indicators for Share of Cost status; iii. State Aid codes; iv. Medicare; and v. Other County responsibility; (d) Supports entry of the Medi-Cal Eligibility Verification Code (EVC); (e) Supports entry of the Medi-Cal Primary and Secondary Aid Exhibit C – RFP No. 901004 Page 9 A 6. 7. 4. B C D E F Comments Codes and County Code to support the eligibility status; (f) Supports special indicator review and processing (ex: pregnancy and emergency); (g) Supports user-defined indicators; and (h) Supports entry of Other Health Coverage (OHC). “Benefits / Eligibility / Insurance” that supports: (a) Clearance of a client’s Share of Cost obligation; (b) An algorithm to identify clients with changes in eligibility status and retroactive billing opportunities and on-demand user defined re-billing opportunities and provides for user alerts. “Eligibility Information Access” that: (a) Supports access to a client’s eligibility records from other system modules (e.g., Call Logging, Appointment Scheduling, and Registration). Billing Requirements: 1. “Billing General” shall have the ability to: (a) Provide multi-site billing with centralized billing office model (includes shadow billing). Must allow for multiple tax identification, EIN (employer ID number, multiple provider/legal entity, etc); (b) Provide multi-site billing with de-centralized billing office model (including shadow billing); (c) Integrate or interface with registration, appointment scheduling, clinical EHR, authorizations, and eligibility components; (d) Use multiple fee schedules and multi-tiered fee schedules in billing process, with capacity to override and store historical information with start/stop dates; (e) Provide fee schedule update capability at the individual fee code level, and store historical data; (f) Provide global update of fee schedules; (g) Upload billing, EOB, RA, and Denial Information from various sources (835/837) or the defined Federal standard; (h) Upload reference tables, including: i. CPT-4; ii. CPT-4 Modifiers; iii. DSM-IV; iv. DSM-V; Exhibit C – RFP No. 901004 Page 10 A B C D E F Comments v. ICD9 diagnosis codes; vi. ICD10 diagnosis codes; vii. HCPCS; viii. HCPCS Modifiers; ix. Revenue codes; x. Place of service codes; xi. Local codes; xii. DRG; xiii. Bill Type; xiv. NDC; xv. US Postal tables (plus four); and xvi. User defined tables. (i) Manually modify reference tables; (j) Create reference tables; (k) Establish user defined billing rules, such as exclusion rules for unique billing circumstances; (l) Bill using sliding fee schedules; (m) Incorporate Medi-Cal (Phase II) regulations into billing component; (n) Track Medi-Cal Share of Cost history; (o) Provide annual liability calculations and tracks limits; (p) Incorporate Medicare regulations into billing component, including billing units (minutes, hours, time or rate based); (q) Tracks user, date and time of any additions, changes or deletions of billing related transactions; (r) Manage multiple reimbursement methodologies, including but not limited to: i. Fee-for-Service; ii. Case rates; iii. Per diem; iv. Capitation; v. Fixed rates; vi. Grant-in-aid; vii. Bundling and unbundling of service codes by payer and/or provider; viii. Self-pay; and ix. Sliding fee schedule. (s) Handle coordination of benefits / sequential billing of payers, ensuring that the sequence is based on coverage the client has and the services that are covered by the plans; Exhibit C – RFP No. 901004 Page 11 A B C D E F Comments (t) 2. 3. Manage the coordination of benefits and sequential billing that is based on provider contractual parameters. Can handle multiple contractual coverage/reimbursement schemes; (u) Bill for a single client who has multiple distinct episodes; and (v) Bill multiple clients to a single guarantor / responsible party. “Service Entry / Charge Capture” shall have the ability to: (a) Provide manual, batch-based charge entry with drop down menus; (b) Bill administrative and educational services that are not related to a specific client; (c) Enter multiple co-staff; (d) Record and bill Medi-Cal Administrative Activities (MAA); (e) Record and bill Medi-Cal Quality Assurance activities (QA); (f) Record and bill County Defined Services; (g) May generate services and charges based on progress note documentation; (h) Offer coding assistance to providers based on client record documentation and number of clients in a group and do appropriate calculation of service time; (i) Detect duplicate service entry with provider or crossproviders, and alerts provider at time of entry; (j) Link appointment tracking number to charges for reconciliation purposes; (k) Edit, delete, rollback, or rebill charges at a user-restricted level; (l) Transfer service entry from one client number to another client number, based on user profile/security level; (m) Perform service entry transfer based on user definition such as date range etc.; and (n) Define and upload service data from external providers (including 835/837 formats). “Charge Generation” shall have the ability to: (a) Calculate charges based on: i. Time or duration of service; ii. Units of service by service codes; and iii. Incident-to and non-Incident-to services by program. (b) Split charges or prorate charges amongst treatment staff (c) Calculate fees for group an d subgroup service billing, which may include multiple programs/providers. Exhibit C – RFP No. 901004 Page 12 A 4. 5. B C D E F Comments “Charge Review” that provides: (a) A review stage and release option; (b) Automatic billing edits to validate: i. Treatment staff credentials and discipline are appropriate to service rendered; ii. Staff allowed program locations; iii. System can store or access external staff certification system; iv. Site and treatment staff certification is appropriate to payer; v. Checks time durations for validity, allowing application of edits dependent on payor source; vi. Checks service location appropriate to service rendered; vii. Aid code or other restrictions (emergency/pregnancy indicator) and have ability to make corrections individually or in batch; and viii. Detects duplicate service entry, within a provider and cross-providers, with alerts. “Claim Submission” shall have the ability to: (a) Support HIPAA compliant EDI formats for claims submission; (b) Support on-line entry of claims with the same full complement of data fields; (c) Support the full audit trail tracking of claims submissions/resubmissions and actions according State/County/Federal guidelines; (d) Support ability to force cascade billing based on County parameters; (e) Support inclusion of zero balances in cascade billing based on County parameters; (f) Schedule re-verification of Medi-Cal eligibility prior to claim processing using 270/271 in batch, with ability to store 271 responses in table and as an image; (g) Flag and hold claims from submission based upon userdefined criteria; (h) Release flagged claims based upon user-defined criteria; (i) Support on-line entry/EDI upload screen data elements to allow input, including: i. CMS 1500; and ii. UB04 format. (j) Print and reprint the following billing forms according to Exhibit C – RFP No. 901004 Page 13 A (k) (l) (m) (n) (o) (p) (q) (r) (s) (t) (u) (v) (w) (x) (y) (z) (aa) (bb) (cc) (dd) (ee) B C D E F Comments industry standards with appropriately completed and formatted data: i. UB-04; and ii. CMS 1500; System will pre-populate provider and client information for each new entry; Provide electronic submission of claims in the ASC X12N 837I and 837P transaction formats; Provide ability to submit and accept ASC X12N 837I / P transactions and ability to segregate claims based on user defined billing groups within these four categories: i. Claims processing module; ii. External payers, including commercial insurance; iii. Medi-Cal; iv. Medicare; and v. Contract Providers; Provide Medicare or other crossover billing; Bill services to a default payer of last resort other than the client or guarantor; Bill multiple funds for services not covered by other payers; Bill third party insurance carriers; Maintain Medi-Cal and MediCare names (that may be unique to that system); Apply manual adjustments as well as adjustments with COB functionality to outstanding balances; Apply manual adjustments to the annual liability limit; End-user to apply special user-defined payment arrangements; Design custom client statements; Use pre-printed client statements; Print client statements on demand; Print client statements in user-defined groupings or cycles; Suppress printing of bill; Create user-defined messages for letter generation; Allow user to view the statement in the same format as the client; Reprint previous statements; Set up and track grants, or other financial source as a funding source; and Reset claiming information in order to produce a “rebill” (eg: new primary insurance info received and need to generate Exhibit C – RFP No. 901004 Page 14 A 6. 7. B C D E F Comments revised claim to comply with cascade billing). “Payment / Annual Liability / Share of Cost” shall have the ability to: (a) Receive and process an ASC X12N 835 transaction remittance file from multiple payers; (b) Track service to full payment; (c) Receive process and disperse ASC X12N 835 Transaction remittance file(s) received from the State to individual providers; (d) Produce ASC X 12N 835 transaction remittance files to contract providers; (e) Provide automatic, line item posting of payments, adjustments and denials based on ASC X12N 835 remittance file; (f) Manually post payments, adjustments and denials to a line item (or account); (g) Provide automatic batch posting of payments; (h) Handle overpayments and credit balances, and future payments; (i) Develop/maintain user defined rules/system tables for payment and adjustment codes, including the ability to define category and manner in which the system processes these payment and adjustment codes; (j) Provide time of service posting of: i. Co-payments; ii. Share of Cost payments; iii. Annual liability payments; and iv. Balance due payments. (k) Generate cash deposit reports for cash drawer reconciliation; (l) Automatically transfer balances from one payer to the next; (m) Automatically generate bill to next payer once payment is posted; and (n) Provide refund or retention management for overpaid claims or claims paid in error. “Accounts Receivable / Collections Management” shall have the ability to: (a) Show client transaction register real-time, on-line; (b) View the client transaction register with multiple filtering options, including: i. By date range; ii. By provider; iii. By location; and Exhibit C – RFP No. 901004 Page 15 A B C D E F Comments iv. 8. 5. By service payment balance. (c) Transmit account data to outside collection agency (d) Upload claim submission verification from a variety of sources and attach to claim (via PDF) (e) Allow the entry of a claim sent date and use this date to monitor A/R and produce aged A/R reports “Reporting” shall have the ability to: (a) Track missing charges by comparing appointments to charges (b) Provide detailed and summary level accounts receivable aging reports sorted by: i. Payer; ii. Provider; and iii. Location. (c) Produce accounts receivable aging reports based on system generated claim production date or claim sent date; (d) Provide detailed and summary level aged credit balance reports; (e) Provide management reports; (f) Provide reports of charges; (g) Provide reports of payments; (h) Provide reports of adjustments; (i) Provide reports of denials; (j) Provide daily and monthly audit reports for services with or without payer information; (k) Provide daily/weekly/monthly reports for un-finalized progress notes; (l) Define report layouts and choose fields; (m) Generate Medi-Cal cost report; (n) Generate Medicare cost report; (o) Electronically distribute management reports; (p) Write to or modify the database; (q) Access all tables and master files; (r) Produce reports in easily exportable form (ie: flat file, excel or other); and (s) Run potential claim lines through a pre-claim edit process and produce exception reports to allow correction prior to claim submission. Claims Administration Requirements: Exhibit C – RFP No. 901004 Page 16 A 1. B C D E F Comments “Claim Structure” shall have the ability to: (a) Use and validate HIPAA compliant code sets, including: i. CPT-4; ii. CPT-4 Modifiers; iii. DSM-IV; iv. DSM-V; v. ICD9 diagnosis codes; vi. ICD10 diagnosis codes; vii. HCPCS; viii. HCPCS Modifiers; ix. Revenue codes; x. Place of service codes; xi. Local codes; xii. DRG; xiii. Bill Type; xiv. NDC; and xv. Combinations of the above on a single claim. (b) Calculate time across days (past midnight); (c) Add free-text notes to claim; (d) Track claim notes to individual claims; (e) Track user name, date and time on claim notes; (f) Support attachments of scanned documents to a claim; (g) Allow optional front-end claims data entry of partial claim data (Mail room logging, claims entry), including source of file; (h) Support override of adjudication results and codes based on user-specified security levels; (i) Support automatic adjudication rules based on defined business rules by product line, provider specialty and coding specifics; (j) Maintain and create the procedure code master file including multiple modifiers and descriptions; (k) Maintain the diagnosis code master file, including descriptions; (l) Maintain code history in order to adjudicate claims and adjustments with service dates prior to code updates; (m) Receive and process provider submitted ASC X12N 837 Health Claims or Equivalent Encounter Information; (n) Accept Medi-Cal claims submitted by contracted providers in required transaction format; Exhibit C – RFP No. 901004 Page 17 A B C D E F Comments (o) (p) (q) 2. Manually enter CMS-1500 claims; Manually enter UB-04 claims; Provide a data structure with standard claim fields that allows for electronic receipt and upload of ASC X12N 837 format; (r) Provide online access for provider claim entry with edits; (s) Provide separate modules for institutional and professional claims with screen formats that capture all data elements from the CMS-1500 and UB-04; (t) Receive and process the UB-04 format; (u) Perform on-line adjudication; (v) Provide automatic assignment of claim number and retains that number; (w) Track adjudicated claim history with MediCal claim history; (x) Track and match internal claim numbers with Medi-Cal claim numbers when 835 file is received from the State; (y) Bill an adjudicated and paid service on the 837; (z) Bill and track adjudicated local code to billing code on the 837 and retain history; (aa) Convert local adjudicated code to appropriate claiming code and track code history; (bb) Create, configure and maintain the following: i. Claims adjudication rules (as defined by user, and unique to provider); and ii. Claims edits (as defined by user, and unique to provider). Claims Administration: (a) Provider contract specific edits; (b) Fee schedules; (c) Remittance Advice remark codes; (d) Claims adjustment reason codes and descriptions; (e) Claims denial codes and descriptions; (f) Claims suspend codes and descriptions; (g) Claims payment disposition codes and descriptions; (h) Ability to configure and maintain benefit tables and history; (i) Ability to use multiple group or vendor IDs; (j) Ability to use the National Provider Identifier (NPI), designated as facility or individual; (k) Interfaces with the Eligibility module to verify client eligibility; (l) Eligibility data contains start and end dates for current and Exhibit C – RFP No. 901004 Page 18 A B C D E F Comments historical eligibility segments; (m) Ability to enter a reject/denial code which would hold and release claims based on user action; (n) Interfaces with the Authorization module during claims processing; (o) Provides logic to automatically match claim to open authorization based on: i. Procedure codes within a designated range of authorized procedures; ii. Down-coded or up-coded procedures based on system table or program settings; iii. Provider practicing within the same group as the authorized provider or under the same vendor ID; iv. Legal entity or provider within program; v. Client name; vi. Client ID; vii. Type of service; and viii. Date of service. (p) Interfaces with Provider modules and allows claims examiners to look-up provider information; (q) Provides automatic pricing of claim based on the provider's contracted fee schedule and allows manual override; (r) Provides logic to detect user-defined timely filing limits based on service date and claim receipt date and allows manual override; (s) Provides logic to detect Medi-Cal and State Department of Mental Health allowable late codes and adjudicate the claim appropriately; (t) Ability to create user-defined rules for determining whether provider payment for unauthorized services will be pended or paid; (u) Ability to create user-defined rules for determining whether provider payment for unauthorized services will be pended or paid; (v) Ability to identify and validate frequency and duration of service; (w) Provides access to the following additional information from the claims screen during adjudication without losing data entered: i. Client eligibility; ii. Provider contract, affiliation and pricing; Exhibit C – RFP No. 901004 Page 19 A B C D E F Comments iii. iv. v. vi. vii. 3. Procedure auto-coding tools; Diagnosis auto-coding tools; Authorizations; Claims history; and Claims history notes. (x) Ability to initiate global change of claims when benefit plan changes are made. “Pricing” shall have the ability to: (a) Use multiple contractor agreements; (b) Provide logic to price claims with services funded by multiple payers and differing benefit designs; (c) Price service by staff discipline and do manual override; (d) Price claims using multiple payers for a client and the ability to track for each payer: i. Benefit limits; ii. Deductibles; iii. Co-pay; and iv. Co-insurance. (e) Track covered and non-covered services; (f) Price claims using multiple provider reimbursement rate methodologies including: i. Fee-for-Service; ii. Case rates; iii. Per diem; iv. Capitation; v. Fixed rates; vi. Grant-in-aid; vii. Bundling and unbundling of service codes by payer and/or provider; viii. Self-pay; and ix. Sliding fee schedule. (g) Price claims using multiple fee schedules by payer and/or provider, and time period, including state-specific fee schedules; (h) Price claims according to one-time negotiated fee arrangements; (i) Support all industry standard code tables for contract pricing including DSM IV and DSM V; (j) Maintain all standard code tables historically; (k) Support electronic load of code tables; Exhibit C – RFP No. 901004 Page 20 A (l) (m) (n) (o) (p) B C D E F Comments Automatically calculate and load unit values and allow multiple sets of unit value tables (RBRVS, Medi-Cal, etc.); Support integration of contract loading with CPT 4, HCPCS, Rev Codes and ICD-9 and ICD-10 coding software; Support modifier guidelines by product/payer and/or provider, and time period; Support contracts at both the network and individual provider level; Price claims using multiple provider reimbursement rate methodologies including: i. Payment terms and payor/programs the provider is contracted for; ii. Delegation status (for each delegated responsibility); iii. Referral network; iv. Covering provider relationships; v. Support the following contract payment terms: a. b. Percentage of fee schedule; c. d. e. f. g. h. i. j. k. l. Percentage of billed charges; m. Geographic Area Factors (GAF) pricing modifiers; n. o. p. Per Diem rates; Multiple base fee schedules (Medicare and Medicaid); RBRVS (allows percentage of RBRVS); By work unit; By service unit; California Medi-Cal Relative Value Units; DRG - Diagnosis Related Groups; County defined maximum allowed rates; Ability to support recovery and withholds; Inpatient Hospital Care Acute/Admin; Long Term Care Hospital, including PHF (Psych Health Facility) and IMD (Institute of Mental Disorder); Case rates; Differing rates by level of licensure Exhibit C – RFP No. 901004 Page 21 A B C D E F Comments (behavioral health); q. r. s. t. Global all-inclusive rates; Medicaid timely payment reductions; Capitation with exclusions; and Combinations of all of the above. Allow variance for any of the above contract terms by: i. Place of Service; ii. Level of care; iii. Age of member; iv. Diagnosis classification; and v. CPT/HCPCS modifier. (r) Support effective dates for each fee schedule. “Adjudication and Payment” shall have the ability to: (a) Produce a check or EFT (electronic fund transfer) with a unique tracking number that is linked to the claim and any subsequent processes; (b) Allow for manual adjudication of claims (based on user security level); (c) Automatically adjudicates claims on a per claim basis; (d) Adjudicate claims based on: i. User-defined rules; ii. Calculate group service codes based on number in group; iii. Payer eligibility; iv. Service included within benefit plan; v. Provider eligibility including validation of credential status; vi. Covered diagnoses; vii. Primary payer; viii. Secondary or other subsequent payer; and ix. Other user-defined fund source rules. (e) Calculate payment based on credit or debit balances; (f) Provide line item adjudication with whole claim pricing; (g) Enter payment and denial information from coordination of benefits (COB) payers where the County is not the primary payer and calculate the balance due; (h) Provide logic to require COB information prior to County payment of secondary or tertiary benefits, and allows override capability (i) Provide complete COB (coordination of benefits) adjudication (q) 4. Exhibit C – RFP No. 901004 Page 22 A (j) (k) B C D E F Comments including the ability to: i. Price at a secondary and tertiary level; ii. Process claims attachments; iii. Scan and retain claims attachments in the system, and associate them with the appropriate claim; iv. Support direct interaction with the authorization management module to limit claims payment to specific services or service category, lengths of stay, frequency, dates, and providers authorized and decrement counters and amounts authorized as claims are posted against authorizations; and v. Manually override authorization based on security level. Support automated authorization matching, including: i. Procedure codes within a designated range of authorized procedures; ii. Down coded versus up coded procedures; iii. Provider practicing within the same group as the authorized provider or under the same vendor ID; iv. For those instances where auto matching is not possible, support ability to browse open authorizations and system propose best match; v. Support integration with bundling/unbundling software systems; vi. Support line item adjudication with whole claim pricing; vii. Support automated pricing according to one-time negotiated fee arrangements for designated out-ofnetwork care; viii. Support override of adjudication results and codes based on user-specified security levels; ix. Support automatic adjudication based on defined business rules; and x. Ability to configure claims to pend for review based on user-defined criteria. Sets claims to "deny" status when: i. Authorization is required and a matching authorization cannot be found (and identify reason for non-match); ii. Client is not found in eligibility files; iii. Provider is not certified to perform service; and Exhibit C – RFP No. 901004 Page 23 A B C D E F Comments iv. 5. Provider is not found. (l) Generate a user alert when "deny" status occurs; (m) Manually deny claims and attach a reason (code and note); (n) Deny claim based upon provider contract parameters; (o) Provide auto-population and manual entry of the following information on a claim: i. Co-payments; ii. Deductibles; iii. Out-of-pocket maximums; iv. Share of Cost; v. Annual liability; and vi. Co-insurance. (p) Detect duplicate claims or possible duplicate claims; (q) Flag claims as duplicates or possible duplicates and post a duplicate override code; (r) Track service limits for each type of authorization including: i. Number of visits or days; ii. Number of client service hours/minutes; iii. Number of clinician service hours; iv. Number of days, weeks, or months; v. Specific service codes, eligibility codes and plans; vi. Service codes clusters; and vii. Specific dollar limits. (s) Automatically generate reminders to service providers when authorization limits have been reached or nearly reached; (t) Calculate interest based on user-defined parameters; (u) Calculate interest based on provider contract stipulations; (v) Track provider claims appeals and denials from inception to resolution; (w) Provide individual work queues for claims processors and examiners, and supervising staff; (x) Automatically routes claims to queues to the appropriate level of examiner; (y) Allow staff to route claims to a specific work queue, based on security level; (z) Permit claims overrides based on security levels and fields; and (aa) Apply Medi-Cal lock-out rules when adjudicating claims. “Adjustment Processing” shall have the ability to: (a) Link adjustments (e.g., voids and additional payments) of Exhibit C – RFP No. 901004 Page 24 A 6. 7. B C D E F Comments claims to original claim; (b) Adjudicate adjustment claims; (c) Void claims; (d) Suspend or pend certain lines within a claim for research or additional documentation; (e) Produce refunds to clients or providers; and (f) Apply adjustments to provider credit and debit balances. “Auditing” that: (a) Validates each service performed by an identified staff person; (b) Checks services to determine valid time durations and location of service; (c) Checks services for duplicate service entry checks, with error notification at time of data entry at a single provider and across providers; (d) Provides the following random sampling approaches for auditing by: i. Percentage of claims; ii. Provider; iii. Client; iv. Examiner; v. Status (e.g., processed, pending, adjudicated, paid); vi. Dollar thresholds; vii. Specified date; and viii. Funding source / payer type. (e) Provides flagging of claims by category for mandatory auditing; (f) Flags audited claims to avoid inclusion in subsequent audits (flag needs to be customizable); and (g) Provides audit sampling for both prepayment and post payment timeframes. “Provider Network Management” shall have the ability to: (a) Support contract generation and monitoring for provider contracts; (b) Support network and provider maintenance across: i. Lines of business/products; and ii. Companies. (c) Support direct interface with credentialing for adding/updating provider demographic data via: i. Internal credentialing module; ii. External credentialing system; and Exhibit C – RFP No. 901004 Page 25 A B C D E F Comments iii. Provider credentialing status should interface with contract parameters. (d) Allow capture and maintenance of the following demographic data for each provider: i. Multiple addresses (Payment, correspondence, physical, tax ID address, etc.); and ii. Multiple practice/service Locations. (e) Capture and access provider information by service locations/sites including: i. Hours of operation; ii. Provider hours in the location; iii. Directions; iv. NPI Number; v. Language(s) of the provider; vi. Language(s) spoken by the staff; vii. Specialty(ies) based on county definitions; viii. Specialty Board Certifications; ix. Provider Type; x. Panel status (e.g. open, closed established patients only, female only, etc.); xi. Covering provider relationships; xii. Administrative contact person; xiii. User-defined specialty code(s); and xiv. Alias names (first, last). (f) Support effective dates by location; (g) Support multiple language and ethnicity/cultural indicators for an individual provider; (h) Allow for automatic and/or manual generation of vendor numbers separate from provider and network identification numbers; (i) Allow for a vendor number to be assigned to a provider or a network with effective/termination dates; (j) Allow for multiple vendors at one address; (k) Identify a W-9 on file for a vendor; (l) Support free-text provider notes; (m) Provide secured access to notes varying by note type; (n) Support user-defined fields at the provider level; (o) Allow sorting and selecting by user-defined fields; (p) Allow re-labeling of user- defined fields; (q) Allow setting of logic rules for user-defined fields (e.g. Exhibit C – RFP No. 901004 Page 26 A (r) (s) (t) (u) B C D E F Comments allowable table values, additional entry requirements, screen requirements); Allow a provider (with one unique provider number) to have multiple contracting/non- contracting affiliations; Allow stipulation and historical tracking of the following for a provider/vendor by line of business/product line: i. Contracting vs. non-contracting status; ii. User-defined Network affiliation, including multiples; iii. Provider type (Cap, FFS, etc.); iv. Provider status (preferred, terminated, pending, etc.); v. Provider classification code (e.g., PCP, Specialist); vi. Provider group within a Network; vii. Vendor (payee for claims and capitation); and viii. Multiple provider hospital affiliations with specific provider privileges. Support provider searching/inquiry by all of the above identification numbers; Additionally support provider searching/inquiry by combinations of the following criteria: i. Name; ii. Partial Name; iii. Alias Last Name; iv. Multiple alias last names; v. Alias First Name; vi. Multiple alias first names; vii. Specialty populations based on county definitions; viii. Panel status (e.g., open, closed); ix. License number; x. Vendor number; xi. Tax Payer ID number; xii. NPI Number; xiii. Network affiliation; xiv. Provider status (preferred, terminated, pending, etc.); xv. Hospital affiliations; xvi. Funding source; xvii. Location/site; xviii. Zip code; Exhibit C – RFP No. 901004 Page 27 A B C D E F Comments xix. xx. xxi. (v) (w) (x) (y) (z) (aa) (bb) (cc) (dd) (ee) 6. Certifications for specific programs; Open/closed panel status; and Combinations of all of the above. Support network inquiry access displaying providers within the network; Allow provider display to be filtered based on: i. Provider classification code (e.g., PCP, Specialist); ii. Specialty; iii. Provider status (Preferred, Terminated, Pending, etc.); iv. Ethnic/cultural or language Indicators; v. Provider contract type (Cap, FFS, etc.); vi. Location/site; and vii. User defined provider specialty. Provide inquiry access to all network and provider demographic and contract (including history) data from all functions within the system including: i. Customer service; ii. Claims processing; and iii. Authorization/utilization management. Allow linking of clinicians for on-call coverage; Support claims pricing logic and benefit determination for on-call coverage (i.e. payment according to provider being covered rates and terms); Provide a means of merging provider records in the event of duplicate entry with historical tracking of activity and is searchable; Support automatic transfer of all transaction and related information to the new identification number; Provide full workflow integration (i.e., work queues, ticklers/reminders, routing); Interface fully with correspondence module; and Produce checks or electronic fund transfers. Client Registration Requirements: 1. “Contact Logging” shall have the ability to: (a) Log contacts (i.e., incoming telephone calls and walk-in inquiries) and store the information in an on-line database; (b) Provide real-time logging and data collection during contact Exhibit C – RFP No. 901004 Page 28 A (c) (d) (e) (f) (g) (h) (i) (j) (k) (l) (m) (n) (o) B C D E F Comments inquiry; Provide prompting during contact dialogue; Create a user-defined on-line form for capturing contact information; Capture and retain the following data fields: i. Contact name; ii. Additional Name(s)/Alias; iii. Billing Name (may be unique to multiple payors); iv. Additional identifier; v. Funding source / Insurance; vi. Date of call set by system; vii. Time of call set by system; viii. Telephone number(s); ix. Language requirement/Primary language; x. E-mail address; xi. Referring party; xii. Referring party telephone number; xiii. Referring party fax number; xiv. Referring party address; xv. Staff member responding (set by system); xvi. Type of contact; xvii. Notes area; xviii. Reason field; and xix. User-defined fields. Record client contact information without the requirement of opening a case; Identify and link repeat contacts; View contact histories; Assign a unique number to each contact for identification and tracking purposes; Provide decision tree logic based on the type of call or incident for prompting operator; Prompt user to route calls according to user-defined guidelines; Automatically assign the call to staff for research and resolution (workflow integration); Automatically escalate calls according to user-defined time and priority criteria; Document contact and disposition; Provide reports on contact statistics; Exhibit C – RFP No. 901004 Page 29 A B C D E F Comments (p) 2. Provide geographical search capability to provider network information; and (q) Access and / or link to the information and referral database. “Client Registration – General” shall have the ability to: (a) Permit a single client record to be used across multiple modules; (b) Provide a Master Patient Index (MPI); (c) Record a unique client ID number; (d) Generate a unique client ID number; (e) Make available of all client registration data in all modules as needed, without the need for duplicate entry of information; (f) Provide on-line, real-time registration feature for gathering and retrieving the following information: i. Client information, with start/stop dates for demographic data (such as citizenship, address, name, etc); ii. Financial information; and iii. Clinical data information. (g) Search the State MMEF (locally stored copy) for client preregistration to identify Medi-Cal eligibility, and import client data into system; (h) Block entry of duplicate CIN or SSN (based on administrative system settings); (i) Flag client window if user attempts entry of duplicate CIN or SSN (based on administrative system settings); (j) Have system "pend" a new client registration, if client is not found in MMEF, with authorization to approve or delete registration based on user profile; (k) Support de-centralized client registration with audit capacity; (l) Import demographic and financial data from external system; (m) Once entered, all demographic and financial fields can be used on user- defined on-line forms, reports generation and printable documents; (n) Track clients by means of a client status with user-defined levels (e.g., pre-registered, discharged, etc.); (o) Provide inquiry and search capability with duplicate record checking; (p) Provide cross check of name inquiries to identify alias names; (q) Link family members; (r) Retain history of all changes to each registration field, including user, date and time, previous entry; Exhibit C – RFP No. 901004 Page 30 A B C D E F Comments (s) 3. Utilize popup windows or other method to select from predefined tables or dictionaries (e.g., dictionary of city names, zip codes, referral sources); (t) Create unlimited user-defined fields; (u) Add user-defined fields to existing windows, with the option of a field being "required"; (v) Allow for user-definition of which fields are required for registration process to be complete; (w) Include duplicate record management options: i. Merge all information from two patient records into a single record, including patient records with claim history across programs (Mental Health, Alcohol/Drug Treatment, Managed Care, etc); ii. Deactivate records; and iii. Reactivate records. (x) Display potential duplicate (or multiple duplicates) client records on screen simultaneously for review, with line by line comparison, for update or new registration; and (y) Block display of client information based on security settings. Demographic Information: (a) “Client” shall have the ability to: i. Collect client demographic data, including: a. b. c. d. e. f. g. h. i. j. k. l. m. n. First name, last name, middle name, suffix; o. Ethnicity; Multiple alias; Address; "Homeless" indicator; Phone numbers; Employer name; Employer address; Multiple employers; Funding source / Insurance; E-mail address; Social Security number; Date of birth; Sex; Marital status; Exhibit C – RFP No. 901004 Page 31 A ii. iii. p. q. r. s. Primary language; a. b. c. d. e. Consent forms; a. b. c. d. e. f. g. h. i. j. k. l. m. First name, last name, middle name, suffix; B C D E F Comments Referral source (how client was referred); Legal status; and User-defined fields. Assign multiple legal statuses to a single client; Record the date of client signature on the following forms: Client assignment of benefits information; HIPAA notification forms information; Advance Directive indication; and Other user-defined forms. Set a date associated with forms as a reminder to take future action; v. Integrate external documents (scanned/imported) into the clinical record; and vi. Access integrated documents and images from within the client record. “Client Contacts” shall have the ability to: i. Record multiple collateral contacts per client; ii. Collect demographic data for each collateral contact, including: iv. (b) Address; Phone numbers; Employer name; Employer address; Multiple employers; Primary language; Social Security number; Date of birth; Gender; Marital status; and Relationship to client. Client consent to collateral contact receipt Exhibit C – RFP No. 901004 Page 32 A (c) B C D E F Comments of information; iii. Capture effective and termination dates of collateral contact relationship (e.g., conservatorship, payeeship); iv. Link one collateral contact to multiple clients; v. Capture effective and termination dates of collateral contact; and vi. Retain history or archive of previous collateral contacts associated with a client. “Insurance” shall have the ability to: i. Maintain all current and historic insurance company information, including subscriber and effective dates; ii. Record multiple active insurance carriers with primary, secondary and tertiary notation; iii. Classify insurance carrier into user-defined financial class categories for billing rules and reporting purposes; iv. Prompt user to obtain pre-authorization if required; v. Collect insurance coverage data, including: a. b. c. d. e. f. g. h. i. Insurance carrier name; j. k. l. m. n. o. p. Subscriber address, city, state, zip code; Insurance carrier address; Insurance carrier phone number; Group name; Group number; Subscriber ID number; Client ID number; Client relationship to subscriber; Subscriber first name, last name, middle name, suffix; Subscriber phone numbers; Subscriber employer name; Subscriber employer address; Subscriber Social Security number; Subscriber date of birth; Subscriber gender; Exhibit C – RFP No. 901004 Page 33 A q. r. (d) B C D E F Comments Subscriber marital status; Coverage primary, secondary and tertiary; and s. Coverage effective and termination dates. “Client Inquiry / Look-up” shall have the ability to: i. Retrieve patient profile in single view (face sheet), including admission and discharge diagnosis information; ii. Provide inquiry or search feature to determine if a client is new to the system; iii. Provide client search features utilize the following techniques to locate existing client records: iv. v. vi. vii. viii. ix. x. a. b. Soundex; and a. b. c. d. e. f. g. h. Name; a. b. Missing user-defined data elements; and Other search algorithms. Search or inquire for a client by: Partial name; Aliases; Date of birth; Social Security number; Internal client ID number; Client Index Number (CIN); and Combinations of the above. Provide seamless access to client registration if client is not already in the system; Define alert conditions and corresponding messages that will appear when viewing an individual client record; Set alerts in the client record for the following conditions: Bad debt indicator. Display multiple messages and alerts; Include message setting and display functionality based on user security levels; and Set prompt intervals for message alerts to staff for updating client demographic information. Exhibit C – RFP No. 901004 Page 34 A (e) a. b. c. v. 7. B C D E F Comments “Episode Management” shall have the ability to: i. Define and track episodes of care for clients; ii. Open and close client episodes as appropriate; iii. Have multiple client episodes open at same time; iv. Provide standard statistical reporting on episodes, including number of open or closed episodes by: Provider; Location; and Diagnosis. Copy/transfer episodes in a group from one Program Code (Reporting Unit) to another Program Code (Reporting Unit). Online Order Entry Requirements: 1. “Laboratory” shall have the ability to: (a) Provide for on-line order entry of laboratory (lab) tests; (b) Allow only authorized users to order lab tests; (c) Create user defined prompts or alerts when ordering specific lab tests; (d) Print laboratory orders; (e) Transmit a HIPAA compliant electronic laboratory order; (f) Receive lab results electronically; (g) Direct lab results received electronically to provider in-box for review; (h) Monitor/manage lab tests ordered but not yet resulted; (i) Alert staff when lab results are outside of normal limits; (j) Store lab results as discrete values; (k) Provide authorized on-line access to historical lab results; (l) Review and easily compare historical lab test results over time; and (m) Review and update vital statistics. 2. “Formulary Management” shall have the ability to: (a) Manage multiple formularies; (b) Update formularies; (c) Interface with external formulary databases; (d) Use generic and brand name drugs; (e) Identify and flag medications that require periodic lab testing; (f) Capture all data related to a formulary medication including: Exhibit C – RFP No. 901004 Page 35 A 3. B C D E F Comments i. Generic medication name; ii. Brand name medication; iii. National drug code (NDC); iv. Drug class; v. Strength; vi. Dosage Form (e.g., tablet, liquid, etc.); vii. Cost; and viii. Other user-defined fields. “Prescribing / Medication Management” shall have the ability to: (a) Provide for on-line order entry for pharmacy requests, with options to: i. Print a written script; and ii. Transmit a secure HIPAA compliant transaction to an external pharmacy. (b) Ensure that only privileged users can order medications; (c) Capture client medication allergy data; (d) Include presentation of client medication allergy information to providers; (e) Capture and displays client food and herbal allergy information to providers; (f) Create a provider specific medication "favorites" list; (g) Provide on-line order entry for prescriptions with the following options: i. Pick list of formulary medications; ii. Fixed dosage; iii. Security override of fixed dosage; iv. Fixed administration; v. Security override of fixed administration; vi. Refill number; and vii. Prescription expiration date. (h) Create pop-up dialogue box related to a specific dosing, nonformulary process or administration restriction; (i) Dispense and document medications; (j) Interface with auto-dispensing medication machines; (k) Provide dosage assistance logic relating to age and Body Mass Index (BMI); (l) Include a formulary checking feature supporting the following: i. Formulary based on payer; ii. Default formulary as defined by user; Exhibit C – RFP No. 901004 Page 36 A B C D E F Comments iii. iv. v. vi. vii. viii. (m) (n) (o) (p) (q) (r) (s) (t) (u) (v) Drug status; Cost index; Therapeutic class / subclass; NDC number; Lab testing requirements; and Approval process for prescription of non-formulary medication. Require entry of reason for non-formulary choice from dropdown menu or comment field; Include drug interaction checking, with ability to modify to display only moderate / severe interactions; Provide embedded or interfaced drug information databases; Perform the following checks utilizing a drug interaction database: i. Drug-to-drug; ii. Drug-to-allergy; iii. Drug-to-disease; iv. Drug-to-lab test results; and v. Ability to interface with Clinical Pharmacology for items above. Provide a comprehensive medication history including the following information: i. Medication order added to medication history; ii. Medication history updated upon filled notification from the pharmacy; iii. Notification to prescriber of medications not filled; iv. Notification to prescriber of refill requested; and v. Notation of lost medication. Generate county-customizable client consent forms by medication; Print medication instruction sheet for client including the following items: i. Dosage; ii. Administration instructions; iii. Description of medication; iv. Side effects; and v. Adverse reactions. Link to county-specific medication information sheets; Provide on-screen warnings or instructions to providers; Provide alerts to providers if lab testing is recommended; Exhibit C – RFP No. 901004 Page 37 A B C D E F Comments (w) 4. 5. Create rules which account for the relationship between dosage, dosing schedule, maximum quantity and maximum days; and (x) Automatically bill for medication management services. “Transmission and Receipt of Prescription Information” shall have the ability to: (a) Provide e-Prescribing technology; (b) Support physician orders (ie medical orders) for changes in medication and/or other medical-related activities; (c) Provide bi-directional transmission of prescription via "clearinghouse;" (d) Provide messaging and query capability from pharmacy to prescribing provider; (e) Automatically initiate a refill prescription request to and from pharmacy; (f) Include notification to prescribing provider of filled prescription; (g) Link with orders placed by providers; (h) Keep pharmacy orders "open" until filled notification received; (i) Update the medication history when prescription filled notification is received; (j) Add the pharmacy prescription number to medication record; (k) Auto fax prescriptions to pharmacy; and (l) Print prescription. “Reporting” that: (a) Provides standard and ad-hoc reporting capabilities; (b) Includes the following standard reports: i. List of clients currently or previously on a particular medication(s); ii. Total monthly costs; iii. Most frequently prescribed drugs; and iv. Top prescribers of drugs. (c) Reports of prescribed medications by: i. Prescriber; ii. Clinic; iii. Medication; iv. Client; v. Diagnosis; vi. Payor class; and Exhibit C – RFP No. 901004 Page 38 A vii. 8. B C D E F Comments Time period. Service Delivery Requirements: 1. “Screening / Triage” shall have the ability to: (a) Create user-defined on-line forms to assist in the determination of which services the client requires; (b) Access historical client demographic and episode data; (c) Add user-defined fields for staff to track screening and triage efforts; and (d) Specialty population designators, based on county definitions, are available with start and stop dates, and history maintenance. 2. “DSM Assignment” shall have the ability to: (a) Use of DSM IV codes; (b) Collect Axis I - Axis V data; (c) Record multiple diagnoses by Axis; (d) Designate one diagnosis as 'primary'; (e) Designate a diagnosis as "rule-out" or "provisional;" (f) Look-up DSM-IV or DSM-V codes by partial description; (g) Look up DC-03 code (0-5 children); (h) Use ICD-9 codes; (i) Use ICD-10 codes; (j) Provide a cross-walk table to translate diagnoses from one classification system to another; (k) Enter and track multiple diagnoses including client selfreported information and capture narrative data; and (l) Track historical diagnosis information by system date and duration. 3. “Clinician Assignment” shall have the ability to: (a) Assign and track a case manager / coordinator; (b) Display the case manager / coordinator in the client's demographic information; (c) Assign only one primary case manager / coordinator to a client within a program at any given time; (d) Have a secondary case manager/coordinator to a client within a program at any given time; (e) Maintain history of case coordinator / case manager assignments with effective dates; and (f) Associate multiple providers with a single episode of care. Exhibit C – RFP No. 901004 Page 39 A 4. ii. 5. 6. 7. B C D E F Comments Electronic Health Record: (a) Online Documents: i. Vendor supplies a varied library of industry standard forms for: a. b. Assessments; c. d. e. Medication Support; Treatment Planning - need to be able to search through a catalogue of options, and use/create unique treatment plans per county specifications; Service documentation; and Diagnosis. Standard forms can be customized to meet the needs of specific service entities with ability to add fields/data points. Modifiability: (a) Agency should be able to modify, add and delete, without the involvement of the vendor: i. Forms; ii. Reports; iii. Fields; iv. Data dictionaries; v. Workflow definitions, rules, and processes; vi. User types; and vii. Validation rules. User Interface: (a) Easy to navigate, minimizes "clicks" to access features; (b) Use standard Microsoft, or industry standard, user interface conventions; (c) Possess the ability to search system to locate key words; (d) Allow windows displayed and accessibility shortcuts that are configurable by end user to meet personal preferences. Workflow Management: (a) Workflow management tools that can be specific to user classification; (b) Includes, but not limited to: i. Intuitive sequencing of required tasks; ii. Easy accessibility of related tasks (e.g. progress notes, scheduling next appointment, client Exhibit C – RFP No. 901004 Page 40 A 8. 9. 10. 11. B C D E F Comments diagnosis/history); iii. Forward population of fields in subsequent tasks with information obtained in prior tasks; iv. Cascading decision support; and v. Automated user notification of pending tasks (e.g. upcoming Recovery Plan updates, expiring authorizations for specific interventions, finalization of e‐docs, etc.) May include tickler messaging, notes on scheduling tool, onscreen flags, email notification, etc. and flexibility to create flags for client issues. System supports user multi‐tasking: (a) Allows users to concurrently open, modify, and save data on multiple client files, i.e. more than one client file may be open and editable at a time; (b) Allows users to concurrently open, modify, and save data on multiple "forms" (e.g. treatment plan and progress note) for a single client; and (c) Allows users to flexibly arrange concurrent processes (multiple client sessions and/or multiple forms per client) in tiled windows in a manner consistent with Windows standards. Video Conferencing: (a) Provides telemedicine capability by allowing user ability to securely transmit and display live streaming audio/video data in a manner that supports real‐time video conferencing with clients working from secure workstations. User constraints: (a) User‐definable/modifiable constraints (field level validations/edits, workflow constraints, error detection tools) designed to prevent common user‐ generated errors; and (b) Application limits user to in‐scope activities. Decision Support: (a) Extensive tools supporting critical assessment and treatment decisions that will improve the internal consistency of: i. Client‐specific case conceptualization (e.g. coordination of symptoms, dysfunctions, and diagnosis); ii. Treatment planning (coordination of diagnosis with best practices); and iii. Resource brokerage (extensive resource catalogs, Exhibit C – RFP No. 901004 Page 41 A 12. 13. 14. 15. 16. B C D E F Comments dynamic resources information, like current beds available in contract shelters). (b) All informational data elements must be available to facilitate the re-creation of accurate data snapshots for any time period in the systems data history. eg: All data elements in an 837 file to be retrievable via a query or direct access to a table; and (c) Meds Validation - Medical Claiming should Pre-Validate via online Meds utilizing EVC certification and OHC. Scheduling: (a) Provides for user and/or clerk managed scheduling; (b) Allows for non‐client‐related scheduled activities; (c) Allows scheduling for unregistered "clients;" and (d) Generates reminders, such as automated telephone calls, texts, emails, letters. Data types: (a) Allows for a broad array of field‐types, including but not limited to: i. Free text fields; ii. Dropdown fields and lists populated by user defined data dictionaries; iii. Dynamic dropdown lists that filter list items according to existing information; iv. Checkboxes; v. Option buttons; vi. Boxes; and vii. Sliders. Spelling and grammar checking: (a) Has ability to replace / interchange abbreviations for long spelling of words, and provide definition of abbreviations; (b) Has spelling and grammar checking that conforms to industry standards; Messaging: (a) Provides extensive clinical and administrative messaging capability within a provider organization and with external organizations; and (b) Allows automated messaging integrated with workflow, scheduling, supervisory and other functionality. Voice dictation capability: (a) Ability for users to use standard voice dictation software to enter data into the system. Exhibit C – RFP No. 901004 Page 42 A 17. 18. 19. 20. 21. B C D E F Comments Integrates with Other Modules: (a) Billing, Scheduling by treatment modality; (b) Generate services and charges based on progress note documentation; and (c) Offers coding assistance to providers based on client record documentation. Assessments: (a) Library of assessments that can added to and modified by the agency; including client self-assessment. Diagnosis: (a) Previously identified symptoms and dysfunctions are incorporated in decision support for identifying a diagnosis. Planning: (a) Symptoms, dysfunctions, and diagnoses are incorporated in decision support for the treatment planning process; (b) Decision support is provided for treatment planning purposes, including a library of best and promising practices. The library is actively updated by the vendor and updatable by the agency/ end user; and (c) Authorized services must be planned by staff with appropriate credentials that include the service in their scope of practice. “Progress Notes” shall have the ability to: (a) Link progress note to specific treatment plan or goal; (b) Record user, date and time of each modification (e.g. update, change, deletion) to the clinical record; (c) Create note formats specific to service entities and group or individual modalities; (d) Sort progress notes for viewing in chronological or reverse chronological order by encounter date; (e) Filter progress notes by service provider, service type, risk factors, service location, etc.; (f) Incorporate assessment tools into progress note based on treatment goals, symptoms, and dysfunctions to support progress trending functions, including client input; (g) Include electronic signature capability, including the following: i. Provides for electronic provider signature; ii. Allows multiple providers to sign a single record; iii. Permits electronic co‐signatures; iv. Provides for electronic client signatures; Exhibit C – RFP No. 901004 Page 43 A B C D E F Comments v. 22. 23. Finalization of the record requires signature and locks the record for further editing; vi. Provides ability to amend documentation after signing/locking/finalization (allows for amendments as legally allowed); vii. Provides online prompts where signatures or co‐signature are required in the completion of medical records documentation to avoid charting deficiencies; viii. Ability to use "speed notes" in progress note (for repetitive text entries); ix. Ability to attach comment to progress note within the authorization hierarchy, prior to final approval (comment section); and x. Provides for authorization hierarchy for sign‐off and record finalization. “Client History” shall have the ability to: (a) Record client's medical history; (b) Restrict medical data as "confidential;" (c) Record client's behavioral health treatment history; (d) Record client's family history; (e) Record client's substance use history; (f) Record client's specimen results (eg saliva/urine); (g) Record client's criminal history; (h) Record client's social, legal, employment and education history ; (i) Record client's medication history including: i. Prescription medications; ii. Over the counter medications; and iii. Vitamins and herbal supplements. (j) Ability to record client's allergy information including: i. Medication allergy; ii. Food allergy; iii. Other allergy; and iv. Ability to record client's current medical conditions and known prescription side effects. “General Documentation” shall have the ability to: (a) Provide on-line charting and documentation; (b) Provide multiple types of service documentation, including: i. Pre-defined treatment plans; and ii. Online progress notes, both group and individual. Exhibit C – RFP No. 901004 Page 44 A B C D E F Comments (c) 24. 25. Provide multiple methods of service documentation: i. Free text entry; ii. Drop down menus; iii. Point-and-click selection; iv. Ability to create user-defined templates to assist with documentation; and v. Combination of the above. (d) Provide spell-check of service documentation notes; (e) Record treatment goals; (f) Track progress against treatment goals; (g) Link progress notes to treatment plan and goals in treatment plan; (h) Prompt provider to complete documentation pertinent to a particular condition or program; (i) Include clinical database of evidence-based practice guidelines; (j) Establish user-defined evidence-based practice guidelines; (k) Include the ability to document and trend quantitative test results; (l) Documentation of client service automatically drives service capture or transactions; (m) Record client input/grievances with data fields that can capture the type for reporting purposes; and (n) Preserve the content for approved notes if subsequent modifications are made to it. “Client Care / Coordination Plan” shall have the ability to: (a) Provide user-defined treatment plan and crisis management plan templates customizable by multiple variables including: i. Location; ii. Program; iii. Target population; iv. Ability to develop treatment plan libraries; and v. Ability to print treatment plan for client review and signature. (b) Provide the technology to accommodate entry of WRAP or other similar types of consumer recovery plans in the client record; and (c) Provide ability to accommodate flexible modes of searching for Treatment Plan items from an extensive pick list, including customized drop-down boxes and key words. “Special Services” shall have the ability to: Exhibit C – RFP No. 901004 Page 45 A 26. 27. 28. 29. B C D E F Comments (a) Add new programs and service categories within programs. “Group Services” shall have the ability to: (a) Provide management of group services, which can be configured by name; (b) Add and delete clients from groups; (c) Provide single screen documentation and service entry for entire group and ability to add individual notes for residential, outpatient, and bundled day treatment; and (d) Provide independent recording of therapist and co-therapist time, documentation and billing. “Case Management” shall have the ability to: (a) Targeted case management services staff to update parts of the client record including: i. Medical history; ii. Medication history; iii. Educational history; iv. Socialization progress; v. Vocational and Community Service history; vi. Substance use history; vii. Ability to add or modify components of client record; and viii. Ability to create rules to identify when case management services are billable vs. non-billable. “Client Linkage Activities” shall have the ability to: (a) Provide tools to document and track all client referrals in and out of the clinic, department or program; (b) Record and store name of individual or program referring client into department; (c) Record notes associated with referral sources; and (d) Set reminders and triggers for staff based on referral information. “Referral Tracking” shall have the ability to: (a) Generate a referral form to link clients to approved treatment, or recovery, and aftercare support services; (b) Define standard reasons for referral for use on referral form; (c) Record multiple referrals per client; (d) Capture all of the following data elements related to referring a client to another provider: i. Agency; ii. Program / Individual Provider; iii. Contact person or none identified (can leave blank); Exhibit C – RFP No. 901004 Page 46 A B C D E F Comments iv. v. vi. vii. viii. ix. x. xi. 30. Client name and ID; Admit date / Referral date; Requested Services; Authorized services (yes/no); User-defined reasons for referral; Referred from and referred to; Discharge or aftercare plan; and User-defined fields. (e) Set alerts, triggers, or reports at the client record level for periodic follow-up on progress and treatment coordination; and (f) Transfer key components of client record to other program via electronic and paper methods. “Discharge Planning and Management” shall have the ability to: (a) Create a client discharge summary containing the following data elements: i. Admission date; ii. Discharge date; iii. Reason for admission or presenting information; iv. Services received; v. Client response to services or treatments; vi. Provides for collection of Axis I - Axis V DSM IV Diagnosis data; vii. Multiple diagnoses by Axis using current diagnostic standards; viii. Designation of one diagnosis as 'primary'; ix. Medications prescribed; x. Disposition and recommendations; and xi. State required fields, and additional user-defined fields. (b) Provide reporting on episode closures that includes the following data fields: i. Client name; ii. Discharge date; iii. Referral out code, and reason; iv. Referring provider; v. Legal status; vi. Diagnoses; and vii. State required fields, and additional user-defined fields. Exhibit C – RFP No. 901004 Page 47 A B C D E F Comments (c) (d) (e) 31. 32. Re-open a closed episode when client returns for services; Modify a discharge date within legal parameters; Provide reports of client records that have not received services within user-defined periods; (f) Provide user-defined fields to enter clinical review notes on discharge summary including: i. Continued treatment needs; ii. Educational needs; iii. Supervision needs; iv. Progress notes; and v. Medications. (g) Provide reporting capability to capture: i. Open episodes without service activities for 30, 60, 90, 120, 180 days; ii. Closed episodes with referral out; iii. Closed episodes with no referral to external entity; and iv. Ability to write free text notes. (h) Track notes linked to each client episode by a system supplied audit trail that includes: i. User name; ii. Date; and iii. Time. (i) Generate a release to follow-up with client upon discharge. “Health Record Management” shall have the ability to: (a) Define one or more reports as the formal health record for disclosure purposes; (b) Generate hardcopy print of all or part of the health record; (c) Generate electronic copies of all or part of the health record; (d) Maintain administrative files that catalog requests and release of health record information; (e) Maintain administrative files that catalog receipt of and information released via subpoena or court order; (f) Maintain administrative files that catalog medical record information requested and released in cases involving litigation; and (g) Automatically track billing and payment information related to medical record correspondence. “Quality Management / Reporting” shall have the ability to: (a) Create user-defined outcome measures; (b) Generate outcome measure reports; Exhibit C – RFP No. 901004 Page 48 A B C D E F Comments (c) 33. Provide outcome measurement and reporting based on the State DMH MHSA CSS; (d) Generate staffing level reports by facility; (e) Generate caseload reports by clinician; (f) Generate caseload reports by facility or site; (g) Provide daily/weekly/monthly reports for un-finalized progress notes; and (h) Generate productivity reports by clinician, unit, site, or facility. “Workflow Support” shall have the ability to: (a) Provide each clinician with display and printed listing of his or her clients that are active and open; (b) Provide tools for planning and organizing the clinicians’ work; (c) Review progress note history in different formats (by week, month, etc); (d) Provide a summary level user-defined screen (e.g., in-box or dashboard) which can be customized by the clinician to assist with workflow organization; (e) Customize chart layout by clinician; (f) Provide on-line authorized access to a client's historical clinical data including past diagnoses, treatment plans, services and medications; (g) Create multiple views of clinical history depending on level of user; (h) "Flip through" the client data in a manner similar to reviewing a paper chart; (i) Define program or pharmacy benefit plan eligibility based on financial, client and utilization criteria; and (j) Flag a provider when a client meets program or pharmacy benefit plan eligibility criteria, or loses eligibility, or gains other health care coverage. TECHNICAL REQUIREMENTS A=Currently Available B=In Development (within 6 month) C=Available but Requires User/Client Modification D=Available via Vendor Modification E=Available Through Third Party Software F=Not Available Exhibit C – RFP No. 901004 Page 49 A 9. B C D E F Comments System Architecture: 1. The General System shall have the ability to: (a) Provide a multi-tiered web-based environment (based on user permissions); (b) Access all user components via a web browser; (c) Provide enterprise Master Patient Index (MPI) supporting unique client identifiers; (d) Link to a secondary practice management system's MPI (Master Patient Index); (e) Operate on current Microsoft-based operating systems (back end); (f) Include queue management, forms management and print distribution capabilities; (g) Allow vendor to securely access the system remotely via VPN for locally hosted system; (h) Provide a flexible architecture to address integration of multiple systems/utilities using industry standard connectivity protocols; (i) Provide a technical architecture to address WAN/Inter-Site Network connectivity; and (j) Provide Service Oriented Architecture (SOA; Web Services). 2. Network shall have the ability to: (a) Execute application in a Microsoft Terminal Services environment; (b) Execute application in LAN/WAN environment; (c) Designated staff to send or display broadcast messages, alerts and notices within the system; (d) Connect to a Data Warehouse; (e) Connect (import and export) to decentralized media: i. Databases; ii. Reporting Services; and iii. Web Services. 3. Application shall: (a) Provide ability to link documents to a Document Management System (MS SharePoint, FileNet, etc); (b) Provide for sending and receiving an e-fax directly from the system; (c) Provide Application Programming Interfaces (API); and (d) Support mobile devices. Exhibit C – RFP No. 901004 Page 50 A 10. B C D E F Comments Database Requirements: 1. Database shall have the ability to: (a) Utilize SQL Server 2005 enterprise or higher as the Relational Database Management System (RDBMS) or equivalent; (b) Include Entity Relationship Diagram (ERD) of logical design available electronically; (c) Include ERD of physical table design (including attributes) available electronically; (d) Include functional descriptions of stored procedures within the database; (e) Include a complete dynamic electronic data dictionary that includes user-defined fields; (f) Load meta-data into a reporting repository; (g) Provide a normalized data model for processing of data; (h) Provide ad-hoc data access to the production database for trouble-shooting purposes; (i) Make global changes to data in the primary database via back-end; (j) Automatically roll back dead-locked processes; (k) Convert data into XML format; (l) Provide support for Structured Query Language (SQL) for queries; (m) Provide a diagnostic tool or utility to identify contaminated and corrupt files and locate the contamination within the file; (n) Provide a tool or utility to select individual records and execute an update and related downstream data; (o) Provide a tool or utility to select a group of records and execute a mass update and related downstream data; (p) Create data interface forms that are bound to table data; (q) Respond to form events, including ability to pre-populate; (r) Support monthly loading of the Medi-Cal Monthly Eligibility File (MMEF) from the State; (s) Support monthly loading of Other Health Coverage file(s) from other health insurance providers; (t) Support OHC (other health coverage) lookup through a 270/271 online transaction; (u) Support for database mirroring to another server; (v) System design supports methods for archiving, reporting on active and archived records, and retrieving inactive client records; Exhibit C – RFP No. 901004 Page 51 A (w) (x) (y) (z) (aa) 11. B C D E F Comments Allow users to export data (menu driven method) in the following formats: i. .csv, xls; ii. standard text; iii. XML; and iv. Other formats. Support distributive data processing for web or reporting services; Perform distributive data processing: i. Automatically; ii. On or By Schedule; and iii. Manually. Support data importing from external data media; and Ability to partner with vendor for database structural changes. Reporting Requirements: 1. “Reporting Repository” shall have the ability to: (a) Support a reporting repository that is separate from the production database and is synchronized to the production database on a predefined and/or ad hoc schedule; (b) Generate reports without impacting production environment data entry or processing scheduled events; (c) Allow all data elements in system to download to a reporting repository; (d) Generate reports from multiple data repositories ; (e) Capture data from user-defined fields and screens; (f) Access data within a reporting repository by: i. Standard menus and screens; ii. User-defined menus and screens; iii. Standardized reports; and iv. Ad-hoc reports. (g) Create tables with user-defined elements within a reporting repository. 2. “Report Writing” shall have the ability to: (a) Provide one integrated report writer with access to all fields, including user-defined fields (non-proprietary); (b) Provide predefined views of data sets that combine files from multiple tables into logical reporting groupings; Exhibit C – RFP No. 901004 Page 52 A B C D E F Comments (c) (d) (e) (f) Provide a report writer that is menu driven; Provide wizard driven report writing capabilities; Provide a report writer for use by users; Provide a reports menu for users to run pre-specified reports (vendor/county developed); (g) Provide a dynamic and complete data dictionary; (h) Provide help text available within the report writer; (i) Write queries and save them; (j) Output report to a screen; (k) Save reports in the various formats: i. Adobe (.pdf); ii. MS-Excel; iii. MS-Word; iv. MS Access; v. ASCII Plain Text (.csv, .txt); vi. Delimited text format; vii. Data Interchange Format (DIF); viii. HTML; ix. XML; and x. Other. (l) Deliver reports through secure e-mail; (m) Recognize PHI in reports and restrict distribution based upon system settings; (n) Deliver reports to the web (HTTPS, SFTP); (o) Provide data mining tools; (p) Provide specialized reports: i. Decision Analysis Support; ii. Potential Waste; iii. Potential Abuse; and iv. Ad-hoc Analysis Reports. 12. Security Requirements: 1. “Application Access Control” shall have the ability to: (a) Restrict rights, privileges or access at the user and group level; (b) Assign rights, privileges or access to processes for specified tasks; (c) Authorize administrators to manage restrictions or privileges associated with users, groups, and processes including: Exhibit C – RFP No. 901004 Page 53 A B C D E F Comments i. ii. iii. iv. 2. Defining levels of access; Assigning levels of access; Modifying a level of access; and Removing a level of access. (d) Associate permissions with a user using the following access controls: i. User-based (i.e., access rights assigned to each user); ii. Role-based (i.e., users are grouped and access rights assigned to these groups); and iii. Context-based (i.e., role-based with additional access rights assigned or restricted based on the context of the transactions, such as time-of- day, workstation-location, emergency-mode, etc.). (e) Limit user functionality based on the following access rights: i. Read; ii. Write; iii. Modify; iv. Transmit; v. Download; vi. Print; vii. View; and viii. Extract. (f) Revoke the access privileges of a user without requiring deletion of the user; (g) Provide integrated security managed in a central accounts database; (h) Retain history of user accounts and access level; (i) View list of users logged on to system in real-time; (j) Terminate user session in real time; (k) Lock users out of application modules in real time; (l) Add user defined messages to log-on screen based on user profile; (m) Allow system access by authorized users via secure internet connections or county provided VPN connection; (n) User to "break the glass" based upon pre-determined (emergency) criteria; (o) Lock client chart against any data entry or revisions; and (p) Mark any or all of patient's specific information as confidential, prohibiting access to all other users. “Audit Control” shall have the ability to: Exhibit C – RFP No. 901004 Page 54 A B C D E F Comments (a) (b) 3. Generate an audit record for all activity of a given user ; Generate an audit record down to the field level for activity associated with a transaction, from creation to completion, including logging of data additions, changes, and deletions; (c) Meet all State of CA and Federal audit requirements; (d) Provide authorized administrators with the capability to read all audit information from the audit records in user-friendly format; and (e) Alert/notify System Administrators on record tampering activities by users. “Authentication” shall have the ability to: (a) Authenticate the user before any access to protected resources (e.g., PHI) is allowed; (b) Authenticate the user before any access from standalone devices (e.g., mobile devices) to protected resources (e.g., PHI) is allowed; (c) Support complex passwords; (d) Support integration with Active Directory for authentication; (e) Require the user to change their password on a defined schedule; (f) Prevent further viewing and access to the proposed system upon detection of inactivity that remains in effect until the user re-establishes access; (g) Log all unsuccessful access attempts to log-on to the system; (h) Lock-out a user due to user account inactivity (inactivity parameters can be customized); (i) Prevent another log-on attempt for specified time after an unsuccessful log-on attempt; (j) Provide a customizable exception report of all unsuccessful login attempts or attempts to make unauthorized changes; (k) Configure the length of time of user account inactivity (logout process should take user back to login screen); (l) Set a maximum number of unsuccessful logon attempts after which user is locked out of the system; (m) Provide security authorization for a predefined/temporary period of time to individuals (ex. audits); (n) Manually or automatically disable accounts after a defined period of inactivity; (o) Provide an administrative function that resets passwords; (p) An administrator to delegate authority, by user group, to reset password; Exhibit C – RFP No. 901004 Page 55 A B C D E F Comments (q) 4. 5. 13. An administrator to delegate authority, by user group, to restore system access of locked out user; (r) Require the password to be changed by a user at the next successful logon; (s) An authenticated user to change their password; (t) Install two-factor authentication mechanisms for access (e.g., RSA tokens); and (u) Support for biometric devices for user authentication (fingerprint, smart card, facial recognition, retinal scan, etc.). “Protection” shall have the ability to: (a) Provide secure information delivery over the Internet via encryption by the most current encryption methods; (b) Prevent display of passwords while being entered; (c) Prevent storage/transmission of unencrypted passwords in Clear Text ; (d) Provide Login restrictions (days, time and workstation, hardwired and dial- up); (e) Provide application menu selection restrictions; (f) Restrict menu or application element display based on user profile; (g) Support for database and field level security; and (h) Input validation prior to committing data to the back end. “Electronic Signature” shall have the ability to: (a) Use digital/electronic signatures in records and documents within the system and with external partners; (b) Utilize Public Key Infrastructure (PKI) technology for digital signatures; (c) Accept external electronic signature from other systems; and (d) Provide for integrity of information delivered over the Internet. EDI (Electronic Data Interface) Requirements: 1. “EDI” shall have the ability to: (a) Accept and transmits information in the following standard formats: i. ASC X12N 270 / 271 Eligibility; ii. ASC X12N 276-277 Claim Status; iii. ASC X12N 275 Patient Information / Claims Attachment; iv. ASC X12N 278 Health Care Services Review; Exhibit C – RFP No. 901004 Page 56 A (b) (c) (d) (e) (f) (g) (h) B C D E F Comments v. ASC X12N 834 Benefit / Enrollment / Maintenance; vi. ASC X12N 835 Health Care Claim Payment / Advice; vii. ASC X12N 837 Health Care Claim; viii. ASC X12N 997/999 Functional Acknowledgment; ix. TA1 Interchange Acknowledgement; x. NCPDP Telecommunication Standard v 5.1; xi. NCPDP Batch Standard v 1.1; xii. NCPDP SCRIPT Standard 8.1; xiii. NCPDP Formulary and Benefit Standard 1.0; and xiv. Additional formats as needed. Software will be updated to meet current data exchange standards; Electronically transmit EDI claims to Medi-Cal, Medicare and other major insurance carriers using industry standard formats; Transmit EDI claims status to providers, including: i. Errors requiring resubmission; ii. Resubmission validation; iii. Ability to reject claims received electronically due to missing required fields; iv. Ability to transmit electronic statements to thirdparty processing agents; v. Ability to customize EDI components including the addition or removal of elements; and vi. Provides data compression for transmitted transactions. Provide data validation based on: i. Data type; ii. Data integrity checks; iii. Comparison edits (e.g., comparison against a table of acceptable values); and iv. User defined rules. Report all preprocessor errors in an inbound batch at one time; Include error processing mechanism for import process reconciliation; Accept electronic imports and exports of the following information and reference files: i. DSM IV; ii. ICD-9; iii. ICD-10; Exhibit C – RFP No. 901004 Page 57 A B C D E F Comments iv. CPT; v. HCPCS; vi. REV Codes (revenue); vii. Taxonomy Codes; viii. NDC codes; ix. Provider data; x. National Provider Identifier (NPI); xi. Mode of Treatment Codes; xii. Service Function Codes; xiii. Member data; xiv. Pricing and fee tables; xv. Client Identification Number (CIN); xvi. USPS Data File (zip code); and xvii. Other. (i) Retain historical code history (date ranges, time stamped); (j) View status of EDI file transfers; (k) Resend EDI file; (l) Support the development of: i. Error checking routines; and ii. Flagging via error reports. 14. Ease of Use Requirements: 1. “User Customization Options” shall have the ability to: (a) Customize existing application components such as: i. Field Labels; ii. User Defined Fields; iii. Validations; iv. Screens; and v. Default Values (based on screen or table). (b) Provide security controlled access to the customization or definition of tables; (c) Establish table edits or validations within user-defined fields; (d) Flag custom programming and prevents overwrite during upgrades; (e) Flag custom help text and prevents overwrite during upgrades; (f) Provide for user-defined screen literals (field label) associated with the data field; (g) Provide for user-defined screen literals not associated with Exhibit C – RFP No. 901004 Page 58 A 2. 3. 4. B C D E F Comments the data field; (h) Provide scripting tools to respond to user and system generated events (ex Java Script, VBA); (i) Define the edit rules for a user-defined data element; (j) Provide automatic data formatting as appropriate (e.g., phone number, dates); (k) Allow for System Administrators to modify and customize existing screen data elements and layout; (l) Support ability to save work in progress; (m) Provide visual cues for user to easily see where they are in their workflow (ie registration or admission); (n) Provide workflow tools to prompt user to continue on to next logical step in business process; (o) Provide "save" and "continue" prompts for user throughout application; (p) Provide a standard user interface throughout all modules for the following actions: i. Searches; ii. Adding / updating data; iii. Report generation; and iv. Navigation through the system. “On-line Help” shall have the ability to: (a) Provide on-line context sensitive definitions for menu-screen selections; (b) Customize help text; (c) Add internal policies and procedures to help text; (d) Provide updates to on-line documentation with each software update; and (e) Provide release notes for every minor or major releases. “User Documentation” shall have the ability to: (a) Include a complete on-line copy of the user documentation; (b) Include on-line user documentation and help files which are searchable based on a topic and/or keyword; and (c) Incorporate wiki-based user support. “Technical Documentation” shall have the ability to: (a) Include a complete on-line copy of the technical documentation (system administration, configuration workbook, system architecture, application architecture, etc.); (b) Provide technical documentation, within each screen that includes source of all data (i.e., data element name and table Exhibit C – RFP No. 901004 Page 59 A (c) B C D E F Comments or calculation); and Include documentation that explains system error or performance messages to users and administrators, with the actions required. 15. System Reliability: 1. “Backups” shall have the ability to: (a) Provide for fully automated backups of data, security credentials, log and audit files; (b) System restore results in a fully operational and secure state, including application data, security credentials, log and audit files; (c) Do selective restore, such as a table or single client record; and (d) Perform complete backups of a running system in production use without shut down or suspension of operations. 2. “Availability” shall have the ability to: (a) Provide user system availability twenty-four (24) hours per day, seven (7) days per week; (b) Include utilities to help monitor and tune performance; and (c) Include standard and remote alerting capabilities. 3. “Business Continuity” shall have the ability to: (a) Create synchronized instances of the system at primary and recovery data center sites; (b) Provide high availability capabilities to the recovery data center for users in the event of a system failure; (c) Provide auto-save function for all user updates, based on system settings; and (d) Generate a backup copy of the application data, security credentials, and log/audit files. 16. Production Scheduling and Control Requirements: 1. “Production Scheduling and Control” shall have the ability to: (a) Establish and support job queues, assign priorities and classes; (b) Provide job scheduling capabilities; (c) Provide event triggered job scheduling; (d) Provide job batch scheduling of multiple processes; Exhibit C – RFP No. 901004 Page 60 A (e) (f) (g) (h) (i) 17. B C D E F Comments Provide system notification to the operator of exceptions including: any communications failure; abnormal job completion; and performance degradation; Print the system log; Interface with third party job scheduling systems; Provide inbound/outbound interface messaging queue management capabilities; Provide data extraction and import scheduling: i. Real-time; ii. Daily; iii. Monthly; and iv. Other. Other Environments Requirements: 1. “Testing, Training, and Development Environments” shall have the ability to: (a) Create separate multiple environments, including: i. Production; ii. Test; iii. Development; iv. Training; v. Disaster Recovery; vi. Staging; and vii. Others. (b) Include test transactions, with input, that have been defined and are available for validating the functionality of the system; (c) Use subset copies of the production database for testing, development or training (i.e., database structure intact with a subset of the real data); (d) Provide testing of configuration changes; (e) Provide testing of control file changes; (f) Create a testing environment that includes all functional components of the production environment; (g) Preserve user profiles when loading a new release to any environment; (h) Comply to standard Data Warehouse extraction and import standards; (i) Copy entire production database into a test environment; Exhibit C – RFP No. 901004 Page 61 A (j) B C D E F Comments and Copy entire production database into an alternate environment with de-identified data. 18. Systems Standards Requirements: 1. “Systems Standards” shall have the ability to: (a) Comply with the security and privacy of health data provisions of the HIPAA Final Security Rules; (b) Comply with State of California and Federal security requirements; (c) Use XML and EDI format; (d) Provide data transmission using current HL7 protocol; (e) Electronically send and receive Continuing Care Documents via HL7 CCD format; (f) Electronically send and receive Clinical Documentation via current HL7 release; (g) Provide data transmission using ASC X12N; (h) Interface with current and commonly used Internet Browsers on Windows and other operating systems; (i) Utilize its own HL7 Parser; (j) Interface with Microsoft Software Management System (SMS); (k) Be compatible with standard networking products; (l) Support Pointsec 2.0 encryption protocol for secure remote laptop access; (m) Support SMTP email messaging protocol; (n) Support for SMS text messaging and SMPP; and (o) Support for IVR voice services. 19. Interfaces Requirements: 1. “Interfaces” shall have the ability to: (a) Interface with OCR, scanning applications and intelligent character recognition software; (b) Interface with translation software (interface engine) for the transmission of electronic claims; (c) Interface with standard voice recognition software; (d) Interface with pen/touch screen devices; (e) Provide data extracts from the EHR database or reporting Exhibit C – RFP No. 901004 Page 62 A (q) repository to feed an external enterprise data warehouse; Interface with (import/export) Netalytics MethaSoft Product (all-inclusive system for Narcotics Treatment Program); Provide an interface engine to create customized interfaces; Use a third party interface engine to create customized interfaces with connectivity support for: i. Oracle RDBMS; ii. MS SQL Server; iii. MS Access; iv. Text Files; v. XML Files; vi. SFTP; and vii. HL7. Notify a third party system in the event a client EHR record is created/modified/deleted; Support a real-time interface to the Medi-Cal Eligibility database; Support a real-time interface to third party health insurance providers (such as Kaiser and Blue Cross); Interface with California Outcome Monitoring System (CalOMS); Interface with internal and/or external third party lab systems for orders and results; Interface with one or more clinical evidence-based practice libraries (e.g., McKesson, Interqual, Milliman Care Guidelines); Interface with the California Performance Outcome System (POS) for surveys; Interface with third party report writers such as Crystal Reports, MS Access, R&R, SQL Reporting Services Report Writer, etc.; Support secure FTP batch interfaces; (r) Interface with standard Document Management Systems; (s) Interface with external Electronic Health Records system to import or export clinical data including Treatment Plans and Progress Notes on a "request" basis; Be compatible with standard Speech Recognition software; (f) (g) (h) (i) (j) (k) (l) (m) (n) (o) (p) (t) B C D E F Comments Exhibit C – RFP No. 901004 Page 63 A (u) Be compatible with standard Screen Reader software; (v) Support for Medical Device Interfaces such as Barcode readers, labelers, etc.; Support distributive data processing interfaces with external services; Import laboratory data - specimen results (Currently using San Diego Reference Lab, Redwood Lab, Terra Firma Lab); and Staff table supports interface with credentialing system and contains necessary fields. (w) (x) (y) B C D E F Comments Exhibit C – RFP No. 901004 Page 64