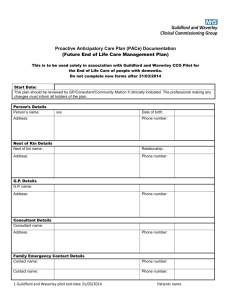
Advanced Care Planning – Clinical Treatment Plan
advertisement

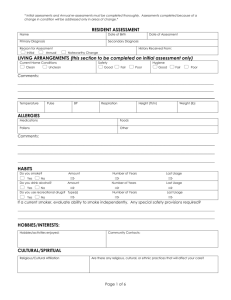
Dorset adapted Proactive Elderly Advanced CarE (PEACE) Suggested anticipatory care plan for care home residents approaching end of life. Based on PEACE from GSTT. This form is advisory only and may not be applicable if the resident’s wishes or clinical condition changes or a situation arises which is not anticipated. If concerns please contact the named Physician or GP for further advice Resident’s name DOB Hosp Number Care Home Physician Tel no Nurse Tel no Discharging Hospital / Ward Date: Summary of medical problems. Resident’s views Does the resident have mental capacity to decide about the actions in the event of progression of their illness? Yes / No If yes, has this Suggested Action Plan been discussed and agreed with the resident? Yes / No Does this person have an: LPA? ADRT? Court Deputy? Possible Developments specific to the resident 1 Lower respiratory tract infection/UTI 2 Fall and limb pain 3 Poor oral intake 4 Signs of possible stroke or coma 5 Person has no signs of life 6 Unexpected acute medical problem/deterioration Action Category Yes / No Yes / No Yes / No details: Comments Please also see supplementary notes for care home staff (attached) Proactive Elderly Advanced CarE (PEACE) SUGGESTED ACTION on PROGRESSION of ILLNESS Resident’s name DOB Hosp Number Care Home Physician Date: Nurse Discharging Hospital / Ward Summary of suggested action categories: Intensive : Transfer to hospital for treatment if appropriate. Critical care, intubation and ventilation should be considered. Hospital : Transfer to hospital for treatment if appropriate but not for critical care, intubation and ventilation. Home : Treatment medication and comfort measures within care home with support from GP. Admission to hospital to be avoided unless comfort measures fail. Comfort : Palliative Medication by subcutaneous, oral or per rectal route, positioning, wound care and other measures to relieve suffering. Implementation of Liverpool care pathway if appropriate. Admission to hospital to be avoided unless comfort measures fail. Views of significant others The patient’s next of kin or advocate have / have not been consulted about this advice? Summary of discussion / views of significant others including if there are differing opinions (which may be relevant to future best interest decisions.) Names Relationship Agree with above? Yes/ No/ Not involved To be contacted? Phone Yes/ No/ Not involved Yes/ No/ Not involved Spiritual needs of the patient at the end of life: Any other Comments This form has been given to: (Please circle) Patient Relative Care Home Suggested review date: GP / OOHS / ED Proactive Elderly Advanced CarE : Guidance for care home staff If your patient deteriorates and has a suggested action of ‘intensive’ or ‘hospital’ treatment, then the appropriate action is to ring the GP/OOHS and if necessary arrange admission to hospital. If your patient deteriorates and has a suggested action of ‘comfort’ or ‘home’, you may find the following grids helpful. In order to carry them out, you may need to ask the GP to come to see the patient and to prescribe as appropriate, and involve PICS or the palliative care service. Please contact the patient’s significant others as stated on the front of this form. Home Oral food as tolerated (eg pureed). If required involve community SALT Oral fluid as tolerated. If required follow SALT advice. Where possible / appropriate you may use sub-cutaneous fluids in the care home. Contact GP for diagnosis and treatment with antibiotics if required. If new pain GP may need to consider the diagnosis, and treat accordingly Feeding Hydration Infection Pain Breathlessness Agitation Nausea/vomiting Diarrhoea Drowsiness/ confusion Fall GP will need to consider cause of breathlessness and what treatment medications are appropriate Ensure no urinary retention/ constipation/ pain or other unmet need If necessary call GP to prescribe sub cut midazolam Check no constipation / urinary infection and treat accordingly + antiemetics Check not overflow constipation (PR). Stool samples for c.diff and treatment if positive. Encourage fluids. Loperamide only if continues for more than 3 days and risk of skin breakdown Check no constipation / urinary infection / dehydration. Consider medications which could be causing this. The GP may need to do blood tests to guide therapy. Examine for injury. If fracture suspected may require admission to hospital for adequate palliative management. Give analgesia prior to transfer. If no injury, consider cause of fall. Consider need for crash mats, low bed, increased supervision and assistance with toileting and transfers. Medications Pressure care area Pressure area care is based on risk assessment and is fully documented. Patient repositioning should be maintained ensuring that pain issues are also addressed. Pressure sores managed at home with review by TVN and GP Comfort Oral fluids or food as tolerated Oral fluids or food as tolerated and as often as tolerated. Low intake is very likely Treat symptoms as required. Fan therapy for temperatures. Call GP/Palliative care to consider medication – oromorph or sub-cut morphine may be required Call GP/Palliative care to consider medication – eg oromorph or sub-cut morphine. Consider oxygen, normal saline nebulisers Ensure no urinary retention/ constipation/ pain or other unmet need If necessary call GP to prescribe sub cut midazolam Check no constipation. GP will need to prescribe anti-emetics, eg cyclizine oral or s/c Check not overflow constipation (PR). Stool samples for c.diff and treatment if positive. Encourage fluids. Loperamide only if continues for more than 3 days and risk of skin breakdown Check no constipation / urinary infection / dehydration. Consider medications which could be causing this. Examine for injury. If fracture suspected may require admission to hospital for adequate palliative management. Give analgesia prior to transfer. If no injury, consider cause of fall. Consider need for crash mats, low bed. Ask GP/Palliative care to review medications – especially to stop unnecessary medications. Pressure area care is based on risk assessment and is fully documented. Patient repositioning should be maintained ensuring that pain issues are also addressed. Pressure sores managed at home with review by TVN and GP In addition, pressure care, mouth care, management of continence issues, and spiritual wellbeing will all be important.