Peripheral vasculature - James Mitchell's Home Page

C 4. The peripheral vascular system a. Describe the distribution of blood volume in the various regional circulations and explain the factors that result in redistribution of blood in health and disease.
Distribution of blood volume:
Pulmonary circulation
Heart
Arteries
Arterioles
Capillaries
Veins
9%
7%
13%
2%
5%
64%
The distribution of cardiac output to various tissues is determined largely by local factors affecting arteriolar tone and to a lesser extent by sympathetic and parasympathetic nervous activity. For laminar flow, Q= Δ P/R where R is resistance in the vessel, equal to 8 η l/ π r 4
Thus:
.
Q =
π Pr
8 η l
4
(Poiseuille’s Law)
Laminar flow occurs in situations where Reynold’s number is less than 200 and turbulent flow at over 2000, with turbulent flow at branching points and other irregularities at values between 200 and 2000. Reynold’s number = vd ρ / η where ρ is density and η viscosity.
Blood flow distribution at rest:
Tissue %CO ml/min ml/min/100g
Brain
Heart
Bronchi
Kidneys
Adrenal
Liver
Muscle
Bone
Skin
0.5
27
15
5
6
14
4
2
22
700
200
100
1100
25
1350
750
250
300
50
70
25
360
300
95
4
3
3
(75% portal)
Local control of blood flow in the short term is determined by tissue metabolism.
Flow rises slower than a rise in metabolism as extraction of oxygen and nutrients is not maximal at rest. The exact mechanism of local vasodilatation is not known. Candidates as local vasodilators include adenosine (and its phosphates), CO
H +
2
, lactate, histamine, K + and
. It is also theorized that oxygen lack causes vasodilatation by relaxing precapillary sphincters.
These mechanisms operate from minute to minute to regulate local flow in most tissues. They also operate over a longer period after an episode of nutrient or oxygen lack, causing reactive hyperaemia after release of a tourniquet or active hyperaemia in a muscle after exercise. The net effect is a constant perfusion of most tissues at rest over a wide range of arterial pressure.
Specialized mechanism operate to regulate local flow in the renal, cerebral and coronary circulations. In the kidney, the juxtaglomerular apparatus adjusts constriction of afferent and efferent arterioles to maintain GFR. In the brain, CO
2
and H + ions act as potent vasodilators.
Arteriolar flow responds to local demands as a result of the release of nitric oxide
(NO). Increased flow through an arteriole causes increased shearing of endothelial cells and results in the release of NO, dilating the arteriole. Many other noxious stimuli also cause
Peripheral vasculature 1.C.4.1
James Mitchell (December 24, 2003)
the release of NO.
In the longer term, hypoxia is a stimulus for the development of new vessels in most tissues over the course of weeks and months.
b. Explain the factors which determine systemic blood pressure and its regulation.
The physiological determinant of systemic blood pressure are cardiac output and total peripheral resistance. The physical determinants are arterial blood volume and arterial compliance. Systemic blood pressure varies between systolic and diastolic pressures, the mean arterial pressure is the average pressure over time.
In physical terms the mean arterial pressure equals arterial volume divided by arterial compliance. Arterial volume (V arterial system (Q h a
) is determined by the cardiac output entering the
) and the peripheral flow leaving it (Q r h
- Q
).
dV a
/dt = Q r
Peripheral resistance is defined as pressure drop divided by flow:
R = (P a
- P ra
) / Q r
Compliance of the large vessels is determined by their physical composition. In the smaller arteries and arterioles, smooth muscle in the vessel walls plays a large role in determining compliance and resistance. It is defined as change in volume per unit change in pressure:
C a
= dV a
/ dP a
It is more useful in physiological terms to describe mean arterial pressure in terms of
. cardiac output and peripheral resistance. P a
will approach equilibrium for a given R and Q h
The rate of approach will depend on arterial compliance: dP a
/dt = (Q h
- R · (P a
- P ra
)) / C
is small compared with P a
In normal circumstances, P proportional to C a ra time gives an exponential equation for P a
approaching Q h a
. Integrating with respect to
· R with a time constant
. So a non-compliant system will show rapid pressure changes in response to changes in cardiac output or peripheral resistance.
The difference between diastolic and systolic pressures is pulse pressure . It is determined by stroke volume and arterial compliance. As cardiac output is the product of stroke volume and heart rate, an increase in stroke volume at a fixed heart rate will increase both mean and pulse pressures. With age and atherosclerosis, arterial compliance falls, resulting in greater pulse pressure without necessarily changing mean pressure. This places greater strain on the heart as it is more efficient at volume work than pressure work.
Control in Cardiac control (1.C.5) c. Describe total peripheral vascular resistance and the factors that affect it.
Resistance in fluid flow is defined as pressure drop per unit flow. Total peripheral resistance (R) can therefore be determined as (P a
- P ra
) / Q r
. In the systemic circulation the majority of resistance is in the arterioles. This is because of the relationship of radius to resistance in vessels:
R = k/r 4 (k = 8
η l/
π
)
Although the arterioles have a greater total cross sectional area than the large vessels, their smaller average radius more than outweighs this. In capillaries, the situation is reversed, mean radius being far smaller again, but the total number of vessels in parallel making it a low resistance section of the circulation.
Peripheral resistance is maintained largely by sympathetic tone maintaining a basal level of vasoconstriction in vascular beds in skeletal muscle and skin. Skeletal muscle constitutes the largest single vascular bed and the major determinant of total peripheral resistance. Resistance in other circulations is also partly controlled by neural factors but also by local control (especially in the brain and myocardium).
α
The main effect of increased sympathetic tone is vasoconstriction of the arterioles via
-receptors. Circulating adrenaline may oppose this effect by causing skeletal muscle vasodilation via ß
2
-receptors at low concentrations.
Peripheral vasculature 1.C.4.2
James Mitchell (December 24, 2003)
Many local metabolites and transmitters affect vascular tone at a local level, vasodilators including adenosine, H + , CO
2
, lactate, K + and phosphate, and some acting via
EDRF (NO): bradykinin, histamine and leukotrienes. In anaphylaxis, sepsis or severe metabolic acidosis, circulating levels of these mediators can result in generalized vasodilation and hypotension (shock).
d. Describe the general mechanisms involved in local vascular control.
Local vasodilation results from increased metabolism via a number of mediators. The products of metabolism H + , CO
2
, lactate, adenosine, K + and phosphate all act as vasodilators, adenosine playing a key role. Oxygen may play a role as a vasoconstrictor.
These factors combine to provide a negative-feedback mechanism to match blood flow and oxygen supply to tissue requirements. In the pulmonary circulation, the situation is reversed, oxygen acting as a vasodilator and CO
2
as a vasoconstrictor.
Mechanical factors play a role in local perfusion in muscle tissue. Blood flow is severely limited during contraction in both myocardial and skeletal muscle due to extrinsic compression of vessels. This effect is opposed by the myogenic mechanism in which vascular smooth muscle contracts in response to an increase in transluminal pressure.
Endothelium-mediated tone results in vasodilation in response to an increase in longitudinal pressure gradient through release of NO, allowing flow to increase with driving pressure.
e. Describe the essential features of microcirculation in relation to its structure, fluid exchange and control mechanisms present in the pre- and post-capillary sphincters.
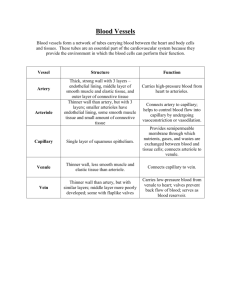
The systemic microcirculation consists of arterioles, metarterioles, capillaries and venules. Arterioles range from 5 µm to 100 µm in diameter and have a media containing smooth muscle. They give rise to capillaries and metarterioles (10-20 µm). Capillaries are around 5 µm in diameter and 0.5-1 mm long forming an interconnecting network. They rejoin to form venules.
Blood flow in the capillary network is regulated at the arteriolar-capillary junction
(precapillary sphincter) and is intermittent in any one capillary, varying from zero to several mm/s. The amount of capillary flow is regulated upstream by arteriolar tone and downstream by venous pressure. Arteriolar tone responds to local factors (myogenic mechanism, EDRF, metabolites and vasodilators) and also to systemic control via sympathetic tone and circulating vasoactive mediators.
The major locally acting vasodilators are EDRF (NO) which acts via cGMP and is released in response to many agents as well as longitudinal pressure gradient and possibly
PGI
2
, released in response to shear stress and acting via cAMP. Metabolites which act as direct vasodilators in adenosine, CO
2
, H + and K + .
Capillary blood has a lower haematocrit (around 15%) than arteriolar blood (more than 30%) because the obligatory cell-free boundary layer of plasma at the endothelial surface represents a significant proportion of the volume of a capillary ( Fabraeus Effect ).
There is also less red cell flow into side-opening capillaries than end-opening ones with regard to arteriolar flow.
The wall of capillaries consists of a single layer of endothelial cells bounded by a basement membrane. The junctions of the endothelial cells include some pores of about
4 nm which are more permeable than the rest of the lining. Some capillaries in the liver, kidney and gut have fenestrations which are large discontinuities in the endothelium covered by membrane. Pinocytotic vesicles are prominent in the endothelial cells.
The capillary wall is permeable as the function of capillaries is the transport of mediators, substrates and metabolic products to and from the periphery. Diffusion is the major transport mechanism across the capillary wall. The rate of diffusion of a substance
(J) is described:
J = -PS · (C o
- C i
)
Peripheral vasculature 1.C.4.3
James Mitchell (December 24, 2003)
Where P is the capillary permeability, S the surface area and C o
- C i
the concentration gradient. For small molecules and ions and highly lipid-soluble molecules, the capillary permeability is very high and their transport across the membrane is flow-limited.
For lipid insoluble molecules, permeability falls rapidly with molecular size to almost zero at 60 kd. Thus albumin, being polar and over 60kd, shows negligible diffusion.
The equilibration of ions and molecules across the membrane is complicated somewhat by the presence of non-diffusible charged molecules such as albumin because of the Gibbs-Donnan effect.
Though most of the water movement across the capillary membrane is a result of diffusion, the net water flow is determined by capillary filtration. Water filtration or absorption across the membrane depends on the net pressure across the membrane. The components of the net pressure are hydrostatic pressure and oncotic pressure. Hydrostatic pressure within the capillary ranges from around 32 mmHg at the arterial end to 15 mmHg at the venous end. Tissue hydrostatic pressure is between –1 and –7 mmHg.
The oncotic pressure ( π ) depends on the concentration of non-diffusible solute (mainly albumin) and its reflection coefficient (
σ
, close to 1 for albumin) and absolute temperature: o
) π =
σ
RT · (C i
- C (R = gas constant)
The net water flow by filtration depends on the total pressure gradient and the filtration constant for water across the membrane (k): flow = k · [(P c
+ π i
) - (P i
+ π p
)]
Total flow is also proportional to the area of membrane and inversely proportional to the viscosity of water and thickness of the membrane.
In most tissues, the net flow of water out of capillaries is small, as the hydrostatic gradient from the arterial to venous end of the capillaries ensures that the rate of water loss at the arterial end is almost balanced by the water absorption at the venous end. In the glomerulus, a high hydrostatic pressure ensures filtration over the whole capillary length whereas in the intestinal mucosa, a high plasma oncotic pressure results in absorption over the entire length.
This mechanism also acts to compensate for blood loss. A fall in both arterial and venous pressure results in a lower hydrostatic pressure over the whole capillary length and consequent absorption of water from the interstitial compartment into the circulation.
Similarly, a rise in venous and arterial pressures, though initially partly compensated for by increased arteriolar tone, results in extravasation of fluid: oedema. Net loss of fluid and albumin is dealt with by the lymphatics which ultimately return them to the circulation.
The last mechanism by which molecules are transferred across the capillary membrane is by pinocytosis. Small amounts of large molecules which are otherwise nondiffusible can be transferred in these vesicles.
Peripheral vasculature 1.C.4.4
James Mitchell (December 24, 2003)