Assessment of the Peripheral Vascular System
advertisement

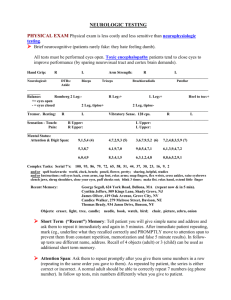
Peripheral Vascular System 1 ALLENTOWN COLLEGE OF ST. FRANCIS DE SALES DEPARTMENT OF NURSING AND HEALTH Nursing 201 Nursing Skills Laboratory Procedure: Assessment of the Peripheral Vascular System ACTION Inspect the arms, from the shoulders to the fingertips, by observing the client’s arms from all angles NORMAL FINDINGS Symmetry in size Skin similar in color to the rest of the body Skin thin, smooth, firm, and even Nail surfaces normal thickness and unridged Presence of a flat, barely visible venous pattern Absence of edema Symmetry Generalized warmth Return of normal color to the nail bed in 1-2 seconds when compression on the nail bed is released Symmetry Normal rate (60-100 Palpate the arms, wrists, and hands for temperature, by 1) placing the dorsal (back) surface of your fingers and hands against the client’s fingers, and 2) moving the dorsal (back) surface of your fingers and hands up the skin of the client’s fingers toward his/her shoulders Test capillary refill of the fingernail beds of the right hand, by 1) squeezing each of the client’s nail beds of his/her fingers between the pads of the thumb and index finger of your right hand for 5 seconds, 2) observing the color of each of the client’s nail beds of his/her fingers, 3) releasing the pressure on each of the client’s nail beds of his/her fingers by the pads of the thumb and index finger of your right hand, and 4) noting the time it takes for the color of the nail beds of the client’s fingers to return to normal (Reverse to test capillary refill of the fingernail beds of the left hand) Palpate the radial pulse of the right arm, by 1) placing the pads of your index and middle fingers on the flexor surface of the client’s right wrist laterally, and 2) ABNORMAL FINDINGS Bilateral or unilateral swelling or atrophy Skin pale upon elevation Skin dusky red (rubor) or cyanosic upon dependency Skin very thin, shiny, atrophic Nail surfaces thickened and ridged Presence of varicosities Presence of edema Asymmetry Generalized coolness Localized areas of warmth or coolness Delay ( 2 seconds) or absence of return of normal color to the nail bed when compression on the nail bed is released Asymmetry Bradycardia ( 60 Peripheral Vascular System 2 pressing the pads of your index and middle fingers lightly on the flexor surface of the client’s right wrist laterally (Reverse to palpate the radial pulse of the left arm) beats per minute) Regular rhythm Elastic arterial wall Normal (2+) force (amplitude) Palpate the ulnar pulse of the right arm, by 1) placing the pads of your index and middle fingers on the flexor surface of the client’s right wrist medially, and 2) pressing the pads of your index and middle fingers lightly on the flexor surface of the client’s right wrist medially (Reverse to palpate the ulnar pulse of the left arm) Symmetry Normal rate (60-100 beats per minute) Regular rhythm Elastic arterial wall Normal (2+) force (amplitude) Palpate the brachial pulse of the right arm, by 1) standing directly in front of the client, 2) placing the pads of your index and middle fingers just medial to the biceps tendon in the client’s right antecubital space, and 3) pressing the pads of your index and middle fingers just medial to the biceps tendon in the client’s right antecubital space (Reverse to palpate the brachial pulse of the left arm) Symmetry Normal rate (60-100 beats per minute) Regular rhythm Elastic arterial wall Normal (2+) force (amplitude) Perform the Allen test on the right arm, by 1) having the client rest his/her right hand in his/her lap with the palm up, 2) placing the pad of the thumb of your left Immediate return of normal color to the beats per minute Tachycardia ( 100 beats per minute Irregular rhythm Thickened, hard, rigid, beaded arterial wall Absent (O), thready or weak (1+), increased (3+), or bounding (4+) force (amplitude) Asymmetry Bradycardia ( 60 beats per minute) Tachycardia ( 100 beats per minute) Irregular rhythm Thickened, hard, rigid, beaded arterial wall Absent (0), thready or weak (1+), increased (3+), or bounding (4+) force (amplitude) Asymmetry Bradycardia ( 60 beats per minute) Tachycardia ( 100 beats per minute) Irregular rhythm Thickened, hard, rigid, beaded arterial wall Absent (0), thready or weak (1+), increased (3+), or bounding (4+) force (amplitude) Delay or absence of return of normal color Peripheral Vascular System 3 hand lightly over the radial artery of the client’s right hand, 3) placing the pad of the thumb of your right hand lightly over the ulnar artery of the client’s right hand, 4) asking the client to clench his/her right fist tightly, 5) firmly compressing the radial artery of the client’s right hand with the pad of the thumb of your left hand, 6) firmly compressing the ulnar artery of the client’s right hand with the pad of the thumb of your right hand, 7) asking the client to open the fist of his/her right hand into a relaxed, partly flexed position, 8) observing the color of the client’s right palm (should be pale), 9) releasing the pressure of the pad of the thumb of your right hand from the ulnar artery of the client’s right hand, and 10) observing the color of the client’s right palm (should be pink) (Reverse to perform the Allen test on the left arm) Palpate the epitrochlear node of the right arm, by 1) asking the client to shake your right hand with his/her right hand, 2) reaching around under the elbow of the client’s right arm, and 3) placing the pads of the index and middle fingers of your right hand lightly in the groove between the biceps and triceps muscles of the client’s right arm about 3 centimeters (1 1/4 inches) above the medial epicondyle of his/her right arm (Reverse to palpate the epitrochlear node of the left arm) Inspect both legs, from the buttocks to the feet, by observing the client’s legs from all angles palm when compression on the ulnar artery is released Usually nonpalpable If palpable: small ( 1 centimeter) with regular borders, round, discrete, mobile, soft, nontender Symmetry in size Skin similar in color to the rest of the body Skin thin, smooth, firm, and even Nail surfaces normal thickness and unridged Even distribution of hair over the lower legs, feet, ankles, and toes Absence of lesions, ulcers Presence of a flat, barely visible venous pattern Absence of edema to the palm when compression on the ulnar artery is released Enlarged ( 1 centimeter) with irregular borders Confluent Immobile Hard, firm Tenderness Bilateral or unilateral swelling or atrophy Skin pale upon elevation Skin dusky red (rubor) or cyanosic upon dependency Presence of brown pigmentation around the ankle Skin very thin, shiny, atrophic Nail surfaces thickened and ridged Loss of hair over the lower legs, feet, ankles, and toes Presence of ulcers Peripheral Vascular System 4 Palpate the legs, ankles, and feet for temperature, by 1) having the client lie down on an examining table, 2) placing the dorsal (back) surface of your fingers and hands against the client’s toes, and 3) moving the dorsal (back) surface of your fingers and hands up from the client’s toes toward his/her hips Test capillary refill of the toenail beds of the right foot, by 1) having the client lie down on an examining table, 2) squeezing each of the client’s nail beds of his/her toes between the pads of the thumb and index finger of your right hand for 5 seconds, 3) observing the color of each of the client’s nail beds of his/her toes, 4) releasing the pressure on each of the client’s nail beds of his/her toes by the pads of the thumb and index finger of your right hand, and 5) noting the time it takes for the color of the nail beds of the client’s toes to return to normal (Reverse to test capillary refill of the toenail beds of the left foot) Palpate the superficial horizontal inguinal lymph nodes of the right leg, by 1) having the client lie down on an examining table, 2) placing the pads of your index and middle fingers over the client’s anterior superior iliac spine of his/her right leg, and 3) moving the pads of your index and middle fingers from the client’s anterior superior iliac spine across to his/her symphysis pubis (Reverse to palpate the superficial horizontal inquinal lymph nodes of the left leg) Symmetry Generalized warmth Return of normal color to the nail bed in 1-2 seconds when compression on the nail bed is released Usually nonpalpable If palpable: small ( 1 centimeter) with regular borders, round, discrete, mobile, soft, nontender Palpate the superficial vertical inquinal lymph nodes of the right leg, by 1) having the client lie down on an examining table, 2) placing the pads of your index and middle fingers over the client’s symphysis pubis, and 3) moving the pads of your index and middle fingers from the client’s symphysis pubis down his/her inner thigh (Reverse to palpate the superficial vertical inquinal lymph nodes of the left leg) Palpate the femoral pulse of the right leg, by 1) having the client lie down on an examining table, 2) placing the pads of the index and middle fingers of your right Usually nonpalpable If palpable: small ( 1 centimeter) with regular borders, round, discrete, mobile, soft, nontender Symmetry Normal rate (60-100 over the tips of the toes, metatarsal heads, lateral malleoli, points of trauma, medial malleoli Presence of varicosities Presence of edema Asymmetry Generalized coolness Localized areas of warmth or coolness Delay ( 2 seconds) or absence of return of normal color to the nail bed when compression on the nail bed is released Enlarged ( 1 centimeter) with irregular borders Confluent Immobile Hard, firm Tenderness Enlarged ( 1 centimeter with irregular borders Confluent Immobile Hard, firm Tenderness Asymmetry Bradycardia ( 60 Peripheral Vascular System 5 hand over the client’s inquinal ligament about midway between the anterior superior iliac spine and the symphysis pubis, and 3) pressing the pads of the index and middle fingers of your right hand deeply below the inquinal ligament about midway between the anterior superior iliac spine and the symphysis pubis (Reverse to palpate the femoral pulse of the left leg) beats per minute) Regular rhythm Elastic arterial wall Normal (2+) force (amplitude) Palpate the popliteal pulse of the right leg, by 1) having the client lie down on an examining table, 2) asking the client to relax his/her right leg, 3) flexing the client’s right leg 90° at his/her right knee, 4) placing the pads of the fingertips of both your hands behind the client’s right knee so that they just meet in the midline of the popliteal space behind the client’s right knee, and 5) pressing the pads of the fingertips of both your hands deeply into the popliteal space behind the client’s right knee (Reverse to palpate the popliteal pulse of the left leg) Symmetry Normal rate (60-100 beats per minute) Regular rhythm Elastic arterial wall Normal (2+) force (amplitude) Palpate the dorsalis pedis pulse of the right leg, by 1) having the client lie down on an examining table, 2) placing the pads of the index and middle fingers of your right hand over the dorsum of the client’s right foot just lateral to the extensor tendon of the client’s right great toe, and 3) pressing the pads of the index and middle fingers of your right hand lightly over the dorsum of the client’s right foot just lateral to the extensor tendon of the client’s right great toe (Reverse to palpate the dorsalis pedis pulse of the left leg) Symmetry Normal rate (60-100 beats per minute) Regular rhythm Elastic arterial wall Normal (2+) force (amplitude) Palpate the posterior tibial pulse of the right leg, by 1) having the client lie down on an examining table, 2) placing the pads of the index and middle fingers of your Symmetry Normal rate (60-100 beats per minute) Tachycardia ( 100 beats per minute) Irregular rhythm Thickened, hard, rigid, beaded arterial wall Absent (0), thready or weak (1+), increased (3+), or bounding (4+) force (amplitude) Asymmetry Bradycardia ( 60 beats per minute) Tachycardia ( 100 beats per minute Irregular rhythm Thickened, hard, rigid, beaded arterial wall Absent (0), thready or weak (1+), increased (3+), or bounding (4+) force (amplitude) Asymmetry Bradycardia ( 60 beats per minute) Tachycardia ( 100 beats per minute) Irregular rhythm Thickened, hard, rigid, beaded arterial wall Absent (0), thready or weak (1+), increased (3+), or bounding (4+) force (amplitude) Asymmetry Bradycardia ( 60 Peripheral Vascular System 6 right hand just behind and slightly below the medial malleolus of the client’s right ankle, and 3) pressing the pads of the index and middle fingers of your right hand lightly just behind and slightly below the medial malleolus of the client’s right ankle (Reverse to palpate the posterior tibial pulse of the left leg) beats per minute) Regular rhythm Elastic arterial wall Normal (2+) force (amplitude) beats per minute) Tachycardia ( 100 beats per minute) Irregular rhythm Thickened, hard, rigid, beaded arterial wall Absent (0), thready or weak (1+), increased (3+), or bounding (4+) force (amplitude) Mild (1+), moderate (2+), deep (3+), very deep (4+) pitting edema Palpate for pitting edema of the right foot, ankle, and leg, by 1) having the client lie down on an examining table, 2) pressing the thumb of your right hand firmly for 5 seconds behind the medial malleolus of the client’s right ankle, over the dorsum of the client’s right foot, and over the client’s right shin, 3) removing the thumb of your right hand from over the dorsum of the client’s right foot, behind the medial malleolus of the client’s right ankle, and over the client’s right shin, and 4) observing for an indentation left in the skin over the dorsum of the client’s right foot, behind the medial malleolus of the client’s right ankle, and over the client’s right shin (Reverse to test for pitting edema of the left foot, ankle, and leg) Test for Homan’s sign of the right calf, by 1) having the client lie down on an examining table, 2) cupping the client’s heel and resting the sole of his/her foot on your forearm, and 3) pressing up on the ball of the client’s right foot with your forearm (Reverse to test for Homan’s sign of the left calf) Palpate the right calf for signs/symptoms of deep phlebitis, by 1) having the client lie down on an examining table, 2) asking the client to relax his/her right leg, 3) flexing the client’s right leg 90 at his/her right knee, and 4) compressing the client’s right calf muscles against his/her tibia with the pads of the fingertips of your right hand (Reverse to palpate the left calf) Inspect the saphenous system for varicosities, by 1) having the client stand, and observing the clients legs from all angles Absence of edema Absence of pain elicited upon dorsiflexion of the foot Presence of pain elicited upon dorsiflexion of the foot Nontender Soft Absence of tension in the calf muscles Tenderness Firm Presence of tension in the calf muscles Perform the manual compression test, by 1) having the client stand, 2) placing your left hand over the lower part of the client’s varicose vein in his/her leg, 3) placing your right hand over the upper part (about 15-20 centimeters above the lower part) of the client’s varicose vein in his/her leg, 4) firmly compressing the upper part of the client’s varicose vein in his/her leg with your right hand, and 5) Presence of a flat, barely visible venous pattern Absence of a palpated pulsation transmitted beneath your lower fingers Presence of dilated, tortuous veins with thickened walls Presence of a palpated pulsation transmitted beneath your lower fingers Peripheral Vascular System 7 palpating the lower part of the client’s varicose vein with your left hand for a pulsation Perform the retrograde filling (Trendelenburg) test of the right leg, by 1) having the client to lie down on an examining table, 2) asking the client to elevate his/her right leg at a 90 angle until the venous blood has drained from the great saphenous vein in his/her right leg, 3) placing a tourniquet around the upper thigh of the client’s right leg tightly enough to occlude the great saphenous vein but not the femoral artery, 4) assisting the client to a standing position, 5) inspecting venous filling of the client’s right leg, 6) releasing the tourniquet around the upper thigh of the client’s right leg, and 7) inspecting venous filling of the client’s right leg (Reverse to perform the retrograde filling (Trendelenburg) test of the left leg) Perform Buerger’s test, by 1) having the client lie down on an examining table, 2) elevating both of the clients legs, ankles, and feet 30 centimeters (1 foot) above the level of his/her heart for 60 seconds, 3) observing the skin color of the client’s legs, ankles, and feet when elevated, 4) having the client sit up and dangle his/her legs, ankles, and feet over the edge of the examining table, and 5) noting the time it takes for the color of the client’s legs, ankles, and feet to return to normal Slow filling (30-35 seconds) from below of the superficial veins while the tourniquet is applied Absence of sudden additional filling of the superficial veins after the tourniquet is released Pallor on elevation Return of preelevation skin color in 10 seconds after the legs, ankles, and feet are dangled Filling of the veins of legs, feet, and ankles in 15 seconds after the legs, ankles, and feet are dangled GRADING PULSE FORCE (AMPLITUDE) GRADE O 1+ DESCRIPTION Absent; not discernible Thready or weak; difficult to feel Rapid filling ( 30-35 seconds) from below of the superficial veins while the tourniquet is applied Presence of sudden additional filling from above of the superficial veins after the tourniquet is released Marked pallor on elevation Return of preelevation skin color in 10 seconds after the legs, ankles, and feet are dangled Filling of the veins of the legs, feet, and ankles in 15 seconds after the legs, ankles, and feet are dangled Dusky red (rubor) or cyanosis of the feet after the legs, ankles and feet are dangled Peripheral Vascular System 8 2+ 3+ 4+ Normal; detected readily, obliterated by strong pressure Increased Bounding; difficult to obliterate GRADING PITTING EDEMA GRADE 1+ 2+ 3+ 4+ DESCRIPTION Mild; 2 millimeter indentation, no perceptible swelling of the leg Moderate; 4 millimeter indentation that subsides rapidly Deep; 6 millimeter indentation that remains for a short time, leg looks swollen Very deep; 8 millimeter indentation that lasts for a long time, leg looks very swollen CHRONIC INSUFFICIENCY OF ARTERIES AND VEINS Pain CHRONIC ARTERIAL INSUFFICIENCY Intermittent claudication Cramping Worsens with elevation Aggravated by walking CHRONIC VENOUS INSUFFICIENCY Slow onset Aching pain Exercise improves pain Better with elevation Peripheral Vascular System 9 Pulses Color Decreased or absent Pale (especially upon elevation) Dusky red (rubor) or cyanosis upon dependency Temperature Edema Skin Changes Cool Absent or mild Absence of hair over the lower legs, feet, ankles, and toes Very thin, shiny, atrophic skin Nails thickened and ridged Ulceration Tips of the toes Metatarsal heads Lateral malleoli Points of trauma May develop Reduced, tissue atrophy Gangrene Muscle Mass NAME OF PULSE Normal Absent CHARACTERISTICS Regular, even in intensity No palpable pulse, no waveform Nocturnal cramping Pruritis Paresthesias Heaviness in the legs at the end of the day Normal, through may be difficult to feel through edema Normal Dusky red (rubor) or cyanosis upon dependency Often brown pigmentation around the ankles Normal Present, often marked Often brown pigmentation around the ankles Stasis dermatitis Possible thickening of the skin Possible narrowing of the leg as scarring develops Medial malleoli Does not develop Unaffected ARTERIAL WAVEFORM PATTERN CONTRIBUTING CONDITIONS Normal Cardiac Arrest Arterial line disconnected Peripheral Vascular System 10 Weak/thready Force (amplitude) is 1+ Difficult to palpate Need to search for it May wax and wane Force (amplitude) is 4+ Very easy to observe in arterial locations near the surface of the skin Very easy to palpate Difficult to obliterate with pressure from the fingertips Has two strong systolic peaks with a dip in between Best detected in the carotid artery Pulsus alternans Alternating strong and weak pulses Equal interval between each pulse Pulsus bigeminus Alternating strong and weak pulses Weak pulse (premature beat) comes in early after the strong pulse (normal beat) Force of premature beat is decreased due to shortened cardiac filling time Pulse beats have weaker amplitude with inspiration and a stronger amplitude with expiration Bounding Biferiens Pulsus parodoxus Water-Hammer, Corrigan’s pulse Shock Severe peripheral vascular disease Hyperdynamic states such as seen with hyperthyroidism, exercise, anxiety, vasodilation seen in high cardiac output syndromes May be due to normal aging secondary to arterial wall stiffening Aortic regurgitation Combination of aortic regurgitation and stenosis Hypertrophic obstructive cardiomyopathy Aortic regurgitation Terminal left ventricular heart failure Systemic hypertension Regular bigeminal dysrhythmias such as PVCs and PACs Pulse beats have greater than normal force then collapses suddenly Rapid systolic upstroke and no dicrotic notch secondary to rapid Cardiac tamponade Acute pulmonary embolus Pericarditis May be present in clients with chronic lung disease Hypovolemic shock Pregnancy Aortic regurgitation Peripheral Vascular System 11 Unequal Difference in the force (amplitude) between right and left pulses ========================== Dissecting aneurysm (location of aneurysm determines where the difference in amplitude is felt