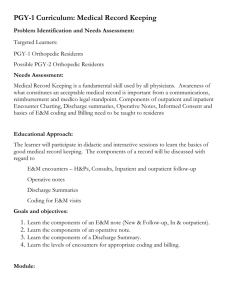
New patient history
advertisement

New Condition Form Name: ________________________________________________ □ Right handed □ Left handed What is the reason for the visit? □ Ambidextrous □ injury □ pain Where is the location of the symptoms? □ Right Date: _____/_____/_________ Occupation: ___________________________________________ □ numbness □ Left DOB: _____/_____/________ □ mass □ other: ______________________________________ Area of body: _________________________________________________ When did the problem begin? _____________________________________________________________________________________ How did the problem start? □ no specific injury □ car accident □ sports □ fall □ work related □ other _________________________ My pain is: □ sharp □ dull □ stabbing □ burning □ throbbing □ aching □ other _______________________________________ My symptoms also include: □ locking □ weakness □ catching How severe are the symptoms? □ swelling □ clicking □ mild □ stiffness □ numbness/tingling □ other __________________________________ □ moderate □ severe □ disabling My symptoms are made better with: □ rest □ heat □ ice □ therapy □ medications My symptoms are made worse when: □ on uneven surfaces □ gripping/grasping □ sitting □ therapy □ working □ instability □ standing □ walking □ overhead activities □ splint □ bending □ reaching □ other_________________________ □ twisting/turning □ throwing □ lifting □ squatting □ typing □ other______________________________ How often do the symptoms occur? □ minimal □ intermittent □ constant □ when sleeping at night □ other____________________ Since the symptoms started, it is □ getting better □ getting worse □ unchanged Which treatments have you tried? □ rest □ heat □ ice □ therapy □ medications □ injection □ splint □ surgery □ other________________________ Patient signature: _______________________________ _________________________________________________________________________________________________________________ Office Use Only Examination: (□ = Normal) □ Constitutional (3) P: R: Ht: Wt: □ General appearance (development, nutrition, body habitus, deformities, grooming) □ Cardiovascular (Peripheral pulse) □ Lymphatic (Palpation of lymph nodes) Neurological/Psychological □ Coordination □ Reflexes □ Sensation □ Orientation □ Mood/affect Musculoskeletal □ Gait - Inspection/palpation (alignment, tenderness, crepitus, swelling) - Stability (laxity, subluxation, or dislocation) Head/neck Right UE Spine/ribs/pelvis Left UE Head/neck Right UE Spine/ribs/pelvis Left UE Right LE Left LE - ROM (with or without pain) Head/neck Right UE Spine/ribs/pelvis Left UE Right LE Left LE - Strength (tone, weakness, atrophy) Right LE Left LE Head/neck Right UE Spine/ribs/pelvis Left UE Right LE Left LE Skin -Inspection/palpation (scars, rashes, lesions) Head/neck Right UE Spine/ribs/pelvis Left UE Right LE Left LE X-ray: □ see report Impression: Plan: Level (3 of 3) History (CC +) Exam Decision Time counseling 1 1 HPI 1 Element SF 10 minutes 2 1 HPI + 1 ROS 6 Elements SF 20 minutes 3 4 HPI, 2-9 ROS 1 PFSH 12 Elements Low 30 minutes M.D. signature: _______________________________________ 4 4 HPI, 10+ ROS 3 PFSH All (29 Elements) Moderate 45 minutes 5 4 HPI, 10+ ROS 3 PFSH All (29 Elements) High 60 minutes Date: ___________________