History - mlcoleman
advertisement

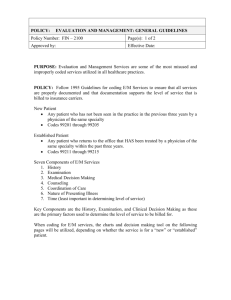
Evaluation & Management Services 1 What is documentation and why is it important? Medical record documentation is required for reporting pertinent findings, facts and observations about a patients health history. The medical record documents patient care showing the chronology of treatment, communication between physicians, quality of care, and collection of data. 2 General principles of documentation Medical record should be complete and legible. Documentation should include: Chief complaint Exam and Diagnostic Test results Assessment Plan 3 E/M Coding Key Components History Physical Examination Medical Decision Making Contributory Factors Nature of the presenting problem • Medical Necessity drives code selection Extent of counseling Coordination of care Time 4 E/M Guidelines Medicare and Commercial Insurance CMS 1995 and 1997 E/M guidelines • Use either set • 1997 approved by AMA Medicaid Does not use ‘95 or ‘97 guidelines Uses AMA guidelines found in the CPT book • E/M Service Guidelines section list “Instructions for selecting a Level of E/M Service” 5 Medical Necessity A service that is reasonable and necessary for the diagnosis and treatment of illness or injury, or to improve the functioning of a malformed body member. Government definition 6 STEP ONE - HISTORY 7 Definitions History Chief complaint (CC) • Reason for the visit History of present illness (HPI) • chronological description of the development of the patient’s illness from the 1st sign and/or symptom to the present. Review of systems (ROS) • is an inventory of body systems obtained through a series of questions asked by the physician seeking to identify signs and/or symptoms that the patient may be experiencing or has experienced Past, Family, Social, History (PFSH) 8 History Definitions - Cont Past, Family, Social, History (PFSH) The PFSH consists of a review of one or more of the following three areas of the patient’s history: • Past History (P) • Family History (F) • Social History (S) The PFSH is considered to be interval history for subsequent inpatient visits. • Interval history - any new history information obtained since the last “physician-patient” encounter 9 History Problem Focused Chief Complaint Brief HPI (1-3) No ROS No PFSH Expanded Problem Focused Chief Complaint Brief HPI (1-3) Problem pertinent ROS (1) No PFSH ALL 3 elements must be met: HPI,ROS,PFSH, FOR A NEW PATIENT. Detailed Chief Complaint Extended HPI (4 or status of 3 chronic/inactive) Extended ROS (2-9) Pertinent PFSH (1) Comprehensive Chief Complaint Extended HPI (4 or status of 3 chronic/inactive) Complete ROS (10) Complete PFSH (2 or 3 based on category of E/M) 10 CPT History Guidelines (Medicaid) Problem focused: CC; brief HPI Expanded problem focused: CC; brief HPI, problem pertinent ROS Detailed: CC; extended HPI, problem pertinent ROS extended to include a review of limited number of additional systems; pertinent PFSH directly related to the patient’s problems Comprehensive: CC; extended HPI, ROS which is directly related to the problem(s) identified in the HPI plus a review of all additional body systems; complete PFSH 11 Elements of History HPI Location Quality Severity Duration Timing Context Modifying factors Associated signs and symptoms 12 Elements of History - HPI Location – place, whereabouts, site, position. Where on the body is the patient experiencing signs or symptoms? (e.g., pain in groin) Quality – A description, characteristics, or statement to identify the type of sign or symptom. (e.g., burning pain in groin) Severity – Degree, intensity, ability to endure. (e.g., History of mild burning pain in groin that has become more intense) 13 Elements of History - HPI Duration – Length of time. How long has patient been experiencing the signs or symptoms? (e.g., History of intermittent mild burning pain in groin that has become more intense and frequent for the last two weeks) Timing – Regulation of occurrence. A description of when the patient experiences signs or symptoms (e.g., history of intermittent mild burning in groin that has become more intense and frequent for the last two weeks). 14 Elements of History - HPI Context – Circumstances, cause, precursor, outside factors. A description of where the patient is or what the patient does when the signs or symptoms are experienced (e.g., history of intermitted mild burning pain in groin that has become more intense and frequent for the last two weeks since the patient bent down to pick up son and continues to feel intense pain when bending). 15 Elements of History - HPI Modifying Factors – Elements that change, alter or have some effect on the complaint or symptoms (e.g., history of intermittent mild burning pain in the groin that has become more intense and frequent for last two weeks since the patient bent down to pick up son; continues to feel intense pain when bending. Patient currently on Motrin 800 mg BID for past 3 weeks without relief) Associated Signs and Symptoms – Factors or symptoms that accompany the main symptoms. What other factors does patient experience in addition to this discomfort/pain? (e.g., Shortness of breath, lightheadedness, nausea/vomiting) 16 Elements of History - ROS Constitutional (e.g., fever, weight loss/gain, lack of appetite) Eyes Ears, nose, throat, mouth Respiratory Gastrointestinal Genitourinary Musculoskeletal Integumentary (skin and/or breast) Neurological Psychiatric Endocrine Hematologic/Lymphatic Allergic/Immunologic 17 Documentation Example of ROS Patient denies loss of consciousness. He has not had any bowel or bladder problems. All other systems are negative. 18 Evaluation of Sample ROS Patient denies loss of consciousness or bowel/bladder problem. All other systems are negative. Neurological = loss of consciousness Gastrointestinal = no bowel Program Genitourinary = no bladder problems All other neg 19 Element of History - Past/Family/Social History - (PFSH) Past History: the patient’s history of illnesses, operations, injuries, treatments, medications. Family History: a review of medical events in the patient’s family, including diseases which may be hereditary or place the patient at risk.” Social History: Contains marital status and/or living arrangements; current employment; occupational history; use of drugs, alcohol and tobacco; level of education, sexual history; or other relevant social factors. 20 Body Areas vs. Organ Systems The exam components are divided up between body areas and organ systems. These can be combined when counting elements for exam. BODY AREAS Head, incl. Face Neck Chest, incl. Breasts & axillae Abdomen Genitalia, groin, buttocks Back, incl. Spine Each extremity ORGAN SYSTEMS Constitutional (vitals & general appearance) Eyes ENT, mouth Cardiovascular Respiratory Gastrointestinal Genitourinary Musculoskeletal Skin Neurologic Psychiatric Hematologic/Lymphatic/Immunologic 21 History CASE STUDY New patient is complaining of a white vaginal discharge for the past 2 days with a heavier flow in the morning. There is no change with Monistat. Patient denies itching burning with urination or fever. Patient has had 2 sexual partners in the past 60 days 22 History CASE STUDY What is the patient’s CC ? Vaginal Discharge What are the patient’s Elements of HPI? 1. 2. 3. 4. Location - vaginal Duration - past 2 days Timing - a heavier flow in the morning Modifying factor - There is no change with Monistat What is the Level of HPI? Ans: Detailed CASE STUDY New patient is complaining of a white vaginal discharge for the past 2 days with a heavier flow in the morning. There is no change with Monistat. Patient denies itching burning with urination or fever. Patient has had 2 sexual partners in the past 60 days 23 History CASE STUDY What is/are the ROS? Integumentary - itching Genitourinary - burning with urination Constitutional - fever What is the Level of ROS? Ans: Detailed What is/are the patient’s PFSH PH (past history) – N/A FH (family History) - N/A SH – (social history) - Patient has had 2 sexual partners in the past 60 days What is the Level of PFSH? Ans: Detailed CASE STUDY New patient is complaining of a white vaginal discharge for the past 2 days with a heavier flow in the morning. There is no change with Monistat. Patient denies itching burning with urination or fever. Patient has had 2 sexual partners in the past 60 days 24 History CASE STUDY ANSWER/EXPLANATION History Level = Detailed (3 of 3) CC HPI = Extended (4+ elements) ROS = Extended (3 elements) PFSH = Pertinent (1 element) EXAMPLE CC - Vaginal discharge HPI - New patient is complaining of a white vaginal (location) discharge for the past 2 days (duration) with a heavier flow in the morning (timing). There is no change with Monistat (modifying factor). ROS - Patient denies itching (integumentary), burning with urination (genitourinary) or fever (constitutional). 25 PFSH - Patient has had 2 sexual partners in the past 60 days (social) STEP TWO – EXAMINATION Performed by Physician 26 Physical Exam Problem Focused (95)<1 body area/ organ system (97) 1-5 elements Expanded Problem Focused (95) 2-4 body areas/ organ systems (97) 6 - 11 elements Detailed (95) 5-7 body areas/organ systems (97) 12 elements in 2+areas/systems Comprehensive (95) 8 organ systems (97) General exam: Perform all elements document at least 2 elements in each of 9 areas/systems 27 CPT Physical Exam Guidelines (Medicaid) Problem focused: limited exam of the affected body area or organ system Expanded problem focused: limited exam of the affected body area or organ system and other symptomatic or related organ system(s) Detailed: extended exam of the affected body area(s) and other symptomatic or related organ system(s) Comprehensive: general multi-system exam or a complete exam of a single organ system 28 Physical Exam Example Vaginal Discharge Exam Constitutional • BP, temp, pulse Genitourinary • Examination of external genitalia • Examination of cervix What is the Level of the Physical Exam? ANS: Problem Focused = (At least two body areas/organ systems) CASE STUDY New patient is complaining of a white vaginal discharge for the past 2 days with a heavier flow in the morning. There is no change with Monistat. Patient denies itching burning with urination or fever. Patient has had 2 sexual partners in the past 60 days 29 STEP THREE MEDICAL DECISION-MAKING 30 MEDICAL DECISION-MAKING MDM refers to the complexity of establishing a diagnosis and/or selecting a management option. MDM is the function of 3 variables 1. Number of diagnoses and/or management options 2. Amount &/or complexity of data that must be obtained, reviewed &/or analyzed 3. Risk of significant complications, morbidity &/or mortality 31 Number of Diagnosis and/or Management Options Self Limited or Minor; stable, improving, worsening x1 Established Problem*; stable, improved x1 Established Problem*; worsening X2 New Problem*; no workup planned X3 New Problem*; addl. workup planned x4 Total Diagnosis or management options 32 Amount and/or Complexity of Data Documentation should include: Diagnostic service: • Ordered, planned, scheduled or performed Review of tests results • Simple notation or initialing & dating Decision to obtain old records or additional History Relevant findings from review of old records Discussion of results with performing physician Direct visualization and interpretation 33 Risk of Complications, Morbidity and/or Mortality Refers to patient’s level of risk at the visit Sources of risk Presenting problem Diagnostic procedures ordered Management options selected Illustrated by clinical examples in “Table of Risk” 34 Documented Example of MDM A/P (assessment/plan): By history, suspect possible herniated disk. Patient will be referred for MRI scan. Prescribe Motrin 800 mg, tid with food, Vicodin for pain. 35 Evaluation of MDM A/P: By history, suspect possible herniated disk. Patient will be referred for MRI scan. Prescribe Motrin 800 mg, tid with food, Vicodin for pain. Number of dx/tx options = new problem with addl workup Amt/complexity of data = ordered MRI Risk = prescription management 36 Decision Making Straightforward #Diagnostic/treatment options (0 -1) Amt./complexity of data Moderate Complexity (0 -1) Risk (minimal) Low Complexity #Diagnostic/treatment options (2) Amt./complexity of data #Diagnostic/treatment options (3) Amt./complexity of data (3) Risk (moderate) High Complexity #Diagnoses/mgmt options (4) Amt./complexity of data (4) Risk (high) (2) Risk (low) 37 Decision Making Straightforward minimal number of diagnoses or management options considered. little, if any, amount or complexity of data reviewed. minimal risk of complications or morbidity or mortality (expectation of full recovery without functional impairment). Low Complexity limited number of diagnoses or management options considered. limited amount and complexity of data reviewed. low risk of complications or morbidity or mortality (uncertain outcome or increased probability of prolonged functional impairment. 38 Decision Making Moderate Complexity multiple number of diagnoses or management options considered. moderate amount and complexity of data reviewed. moderate risk of complications or morbidity or mortality (uncertain outcome or increased probability of prolonged functional impairment or high probability of severe prolonged functional impairment). High Complexity extensive number of diagnoses or management options considered extensive amount and complexity of data reviewed high risk of complications or morbidity or mortality (uncertain outcome or increased probability of prolonged functional impairment or high probability of severe prolonged functional impairment) . 39 CPT MDM Guidelines (Medicaid) Complexity measured by: # of possible diagnoses and/or the number of management options that must be considered. Amount/complexity of records, tests, other information that must be obtained, reviewed, and analyzed. Risk of significant complications, morbidity, mortality, as well as co-morbidities, associated with the patient’s presenting problem(s), the diagnostic procedure(s) and/or the possible management options. 40 Table of Risk Examples Presenting Problem Minimal – One self-limited or minor problem. Low – Two or more minor problems, one stable chronic illness, acute uncomplicated illness. Moderate – Chronic illness with exacerbation, two of more stable chronic illnesses, undiagnosed new problem with uncertain prognosis, acute illness with systemic pneumonitis, acute complicated injury High – Chronic illness with severe exacerbation, acute or chronic illness that poses threat to life, abrupt change in neurologic status. 41 Decision Making Example Vaginal Discharge Exam New problem, additional workup planned • Lab is ordered (4) Review/order tests in 8xxxx series (1) What is the Level of Medical Decision Making? ANS: Moderate (2 0f 3) Moderate decision making • Undiagnosed new problem with uncertain prognosis • Prescription drug management – Prescription written Extensive # Diagnosis/treatment options Minimal amount of data to be reviewed Table of Risk - Moderate 42 Level Assignment EXAMPLE/CASE STUDY CPT BOOK History = Detailed Physical Exam = Problem Focused Decision Making = Moderate What is the code for a New & Established Patient? ANSWER Level = 99203, new patient If Established Patient = 99214 43 Contributing Factors Presenting Problem Minimal Self-Limited/Minor Low Severity Moderate Severity High Severity Time FACE-TO-FACE Time is a key factor ONLY when: • Counseling or coordination of care takes up OVER 50% of the total visit time 44 Consultation Code Selection 45 Definition of Consultation “A type of service provided by a physician whose opinion or advice regarding evaluation and/or management of a specific problem is requested by another physician or other appropriate source.” Payment for consultation is often significantly higher than other E/M service 46 Consultation vs. Referral Consultation: Requires a physician request for an opinion or advice. Request and reason for consult must be documented. Evidence of opinion and/or advice communicated back to requesting physician. Referral: Is a transfer of care for treatment of a specified problem. Is for a known problem. Physician plans to manage the patient’s care and treatment. No report to referring physician is required. UPIN is required. 47 Four Elements That Distinguish A Consultation 1. 2. A type of service provided by a physician whose opinion or advice regarding evaluation and/or management of an unknown or uncertain problem is requested by another physician or appropriate source. The written or verbal request for a consultation must be documented in the medical record. 3. The consulting physician may initiate diagnostic or therapeutic services at the consultation or subsequent visit. 4. The consulting physician’s opinion and any services ordered or performed must be: a) Documented in the medical record; and b) Communicated by written report to the requesting physician or other appropriate source. 48 Types of Inpatient Consultations Initial Inpatient No difference in new or established Follow-up Inpatient Used to complete an initial consultation Reported one time during hospital stay • Complete initial consult, initiated by consulting physician Requires 3 of 3 key components be documented • Subsequent consult, initiated by attending physician Requires 2 of 3 key components be documented 49 Counseling/Coordination of Care Main factor determining code when takes up MORE than 50% of the total visit time Documentation: • Total visit time • Time spent in Counseling/Coordination of Care – Face to face • Subject/ content Code level is based on the total visit time not just the time spent in counseling 50 Counseling Examples Established patient, 20 minute visit to followup on oral contraceptive use NP 99213 RN 99211 (MA 99213) 15 minutes of a 20 minute visit spent counseling the patient on alcohol and cigarette use during pregnancy NP 99213 RN 99211 (MA 99213) 51 Definitions New Patient Has not received face-to-face services from • ANY provider in the agency • Within past 3 years (AMA) Established Patient Has received face-to-face services from • ANY provider in the agency • Within past 3 years (AMA) 52 Selecting a Level of E/M Identify Place of service (POS) = where (office) Type of service (TOS) = what (Problem/Preventive) Status of Patient = who (New/Established) Determine the extent of history - physical exam - decision making - counseling Must consider all factors, and make sure adequate DOCUMENTATION in chart to justify code. 53 Office 99201-99215 Report Problem visit (vs. Preventive visit) 99201-99205, 99212-99215 performed by MD, NP, PA,CNS 99211 - Ancillary staff i.e. RN, LPN, CNA MD/NP must be in the clinic Report only 1 E/M per day Report diagnostic tests, studies, procedures separately 54 Office 99201-99215 (Medicaid) 99201-99205, 99212-99215 may be performed by any staff of a “certified family planning clinic”. Staff may be MD, NP, PA, RN, CMA or unlicensed personnel acting in a coordinated manner to provide the service(s). Other reporting requirements are the same as other providers 55 Preventive Medicine Services 56 Preventive Medicine 99381-99397 Routine management of patients without presenting problems, i.e. annual, routine, well child exams Performed by (MD,NP,PA,CNS) Includes other clinic staff if Medicaid Codes New/established patients Age Not used for scheduled follow-up visits for specified problems 57 CASE STUDY Susan Johnson was referred to Dr. Jones’ office for her opinion of Susan’s chronic low back pain radiating to the leg. Dr. Jones took a detail history, performed a detailed examination, and medical decision making was of low complexity. 99243 58 CASE STUDY Michael, age 38, scheduled an annual physical exam with Dr. Graves. He has been Dr. Graves’ patient for 15 years and had his last annual physical 2 years ago. First - Identify Place of service (POS) = where (office) Type of service (TOS) = what (Problem/Preventive) Status of Patient = who (New/Established) Determine the extent of history - physical exam - decision making counseling 99395 59 CASE STUDY A 2-year-old boy with bacterial pneumonia is hospitalized and has had 5 days of antibiotic therapy. Today the child developed a fever of 101.1 F with a mild rash on his torso. In a subsequent hospital visit, the attending physician performed a problem-focused history and examination. The MDM complexity was low. 99231 60