2 of 3 - Iowa Psychiatric Society
advertisement

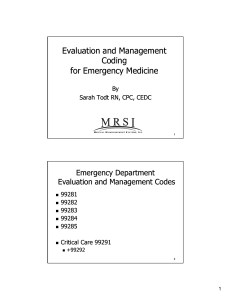
Session 2: Evaluation and Management (E/M) Coding for Mental Health Alison C. Lynch MD Robert E. Smith MD November 30, 2012 Outline of this session • Length of time = 90 minutes • Break down E/M coding into components • Go over criteria for assessment and documentation of these components • Practice using charts (hand outs) to determine what elements need to be obtained and documented Evaluation and management codes— Overview • Medical providers use Evaluation and Management (E/M) codes when billing general office or facility-based visits. • These codes have replaced 90862 and can be used when an E/M service is done in addition to psychotherapy. • The Centers for Medicare and Medicaid Services have established guidelines for selecting the appropriate E/M code. • Codes are divided by new and established patients, site of service, and level of complexity or amount of work required. • The amount of work required is driven by the nature of the presenting problem. • If counseling and coordination of care accounts for 50% or more of the patient encounter, you can select the E/M code on the basis of time EXCEPT when done in conjunction with a psychotherapy visit. (More on this later….) Overview • Billing for an E/M service requires the selection of a Current Procedural Terminology (CPT) code that best represents: – Patient type – Setting of service – Level of E/M service performed – Medical necessity E/M coding should • Reflect the work that was done • Be supported by the documentation – Content, not volume • Reflect care that is reasonable and necessary, that is compliant with the standards of good medical practice • Medical necessity is the over-arching determinant of what code is used Who can use E/M codes? • • • • • Physicians Nurse practitioners* Clinical nurse specialists Certified nurse midwives Physician assistants *NP’s Medicare benefit must permit billing of E/M services, and services must be furnished within the scope of practice in the state in which the NP practices in order to receive payment from Medicare. What are the codes? • • • • • 99201 99202 99203 99204 99205 • • • • • • 99211 99212 99213 99214 99215 et. al. • So how do you know what code to use??? Patient type The first question to ask yourself about a visit is whether the patient is new …. New vs. Established Patient • New: A patient who has not received any professional services from the physician or another physician/nonphysician practitioner of the same specialty who belongs to the same group practice, within the past three years. • Established: A patient who has been seen within the past three years. New: > 3 years • Multisite practices are considered a single group practice for coding New vs. Established Why does it matter? • For new patients, must document all three key coding components (history, exam and medical decision-making) – For established patients, 2 of the 3 components will do • Earn more RVUs for new patients, at all levels of coding – Get credit (and reimbursed) for the work you are doing What about consultations? • Same codes apply to new and established patients for consultations • So no distinction is necessary Determine Setting • • • • Office or other outpatient setting Hospital inpatient Emergency department Nursing facility Determine level of care • This is the most complicated component…. • In general, the more complex the visit, the higher level of code used, (and the higher reimbursement rate) Level of care—3 components • History • Examination • Medical decision making • Exception• Time is the key factor in determining level of care if the visit consists predominantly (>50%) of counseling or coordination of care (More about this later…) History types (4) • • • • Problem focused Expanded problem focused Detailed Comprehensive History Components • • • • Chief complaint History of Present Illness Review of Systems Past, Family, and/or Social History Criteria for history type History components—CC • Chief Complaint – Required for all levels of E/M services – A concise statement that describes the symptom, problem, conditions, diagnosis, or reason for the patient encounter. – Frequently stated in the patient’s own words. History Components—HPI • History of Present Illness elements – – – – – – – Location (e.g. low mood) Quality (e.g. hopeless, emptiness) Severity (e.g. 7 on a scale of 1 to 10) Duration (e.g. for the past 2 weeks) Timing (e.g. constant, especially at night) Context (e.g. when alone) Modifying factors (e.g. felt better after going to church) – Associated signs and symptoms (e.g. crying, insomnia) HPI—2 types • Brief HPI – Includes 1-3 elements – Example: • CC: anxiety • Brief HPI: Avoiding leaving home for past week • Extended HPI – 4+ elements, related to present HPI or associated comorbidities, or status of at least 3 chronic or inactive conditions – Example: • CC: anxiety • Extended HPI: Patient has been avoiding leaving home for past week. This is the 1 year anniversary of her daughter’s accident. She is having some flashbacks about it, the worst she’s ever had. She’s sleeping about 4 hours/night. She has missed 3 days of work. History Components—ROS ROS Elements • • • • • • • Constitutional Eyes Ears, Nose, Mouth, Throat Cardiovascular Respiratory Gastrointestinal Genitourinary • Musculoskeletal • Integumentary (skin +/breast • Neurological • Psychiatric • Endocrine • Hematologic/Lymphatic • Allergic/Immunologic ROS • • • • • • • Constitutional (e.g. fatigue) Eyes (e.g. blurry vision) Ears, Nose, Mouth, Throat (e.g. dry mouth) Cardiovascular (e.g. palpitations) Respiratory (e.g. cough) Gastrointestinal (e.g. constipation) Genitourinary (e.g. decreased libido) ROS • • • • • • • Musculoskeletal (e.g. tremor) Integumentary (skin +/- breast) (e.g. itching) Neurological (e.g. weakness) Psychiatric Endocrine (e.g. polydipsia) Hematologic/Lymphatic (e.g. bruising) Allergic/Immunologic (e.g. hives, NKDA) ROS—3 types • Problem pertinent ROS – Inquires about the system directly related to CC • Extended ROS – Inquires about the system directly related to CC, plus 2-9 additional systems • Complete ROS – Inquires about the system directly related to CC, plus 10+ additional systems – All positives and pertinent negatives must be individually documented. Notation that all remaining systems are negative is permissible. Past, Family, and/or Social History • PMH, PPH, illnesses, operations, injuries, treatments, medications, allergy • FH: medical events, diseases, hereditary conditions that may place patient at risk • SH: age appropriate review of past and current activities PFSH—2 types • Pertinent PFSH: – At least one item from any of the three areas is documented. • Complete PFSH: – At least one specific item from 2 of the 3 history areas are documented (established pt). – At least one specific item from all 3 of the 3 history areas are documented (new pt). Other notes on the history • ROS and/or PFSH obtained during earlier encounter does not need to be re-recorded if clinician reviews and updates previous info. • ROS and/or PFSH may be recorded by ancillary staff or on a form completed by the patient. Clinician must note review and confirmation of info recorded by others. • If clinician unable to get history from pt or other source, record should describe the patient’s condition which precludes obtaining a history. Examination—4 types • • • • Problem focused Expanded problem focused Detailed Comprehensive • The type and extent of the examination is based upon clinical judgment, patient’s history, and nature of presenting problem(s). Psychiatry-specific exam • Can be used for examination of patient with a mental health presenting problem, in place of a general multi-system examination Exam types • Problem focused exam – Perform and document exam of 1-5 elements • Expanded problem focused exam – Perform and document exam of 6-8 elements • Detailed exam – Perform and document exam of 9-13 elements • Comprehensive exam – Perform and document exam of 14-15 elements Exam elements Constitutional Musculoskeletal • 3 of 7 vital signs • Muscle strength, tone, atrophy, abnormal movements • Examination of gait and station – – – – – – – Sitting/standing BP Supine BP Pulse rate, regularity Respiration Temperature Height Weight • General appearance Exam elements—Mental Status • • • • Speech Thought processes Associations Abnormal or psychotic thoughts • Judgment and insight • Orientation to time, place, person • Recent and remote memory • Attention span, concentration • Language • Fund of knowledge • Mood and affect MS Exam Details • Thought processes: rate of thoughts, content of thoughts, abstract reasoning, computation • Associations: loose, tangential, circumstantial, intact • Abnormal or psychotic thoughts: hallucinations, delusions, homicidal or suicidal ideation, obsessions, preoccupation with violence MS Exam Details • Speech: rate, volume, articulation, coherence, spontaneity, perseveration, paucity of language • Language: naming objects, repeating phrases Other notes on the examination • Specific abnormal and relevant negative findings of the examination of the affected or symptomatic area/system should be documented. • Abnormal or unexpected findings of the examination of any asymptomatic area/system should be described. • A brief statement indicating “negative” or “normal” is sufficient to document normal findings related to unaffected area/system. Medical Decision Making • Refers to the complexity of establishing a diagnosis and/or selecting a management option • Determined by – Number of possible diagnoses – Number of management options – Amount/complexity of medical records, diagnostic tests, other info that must be obtained, reviewed, analyzed – Risk of significant complications, morbidity, mortality, and comorbidities, associated with CC, diagnostic procedures, and possible management options MDM—4 types • • • • Straightforward Low complexity Moderate complexity High complexity Number of diagnoses or management options • Minimal – 1 established diagnosis – Problem(s) improved – 1 or 2 management options • Limited – 1 established diagnosis and 1 rule-out or differential – Stable or resolving problem(s) – 2 or 3 management options Number of diagnoses or management options • Multiple – 2 rule-out or differential diagnoses – Unstable or failing to change problem(s) – 3 changes in treatment plan • Extensive – More than 2 rule-out or differential diagnoses – Worsening or marked change in problem(s) – 4 or more changes in treatment plan Amount and/or complexity of data to be reviewed • None or minimal – 1 source of medical data – 2 diagnostic tests – Confirmatory review of results • Limited – 2 sources of medical data – 3 diagnostic tests – Confirmation of results with another physician Amount and/or complexity of data to be reviewed • Moderate – 3 sources of medical data – 4 diagnostic tests – Results discussed with physician performing tests • Extensive – 4+ sources of medical data – >4 diagnostic tests – Unexpected results, contradictory reviews, requires additional reviews Risks of significant complications, morbidity, or mortality • Minimal – One self-limited problem (e.g. medication side effect) – Diagnostic testing: laboratory tests requiring venipuncture, urinalysis – Management: reassurance Risks of significant complications, morbidity, or mortality • Low – 2 or more self-limited or minor problems, or 1 stable, chronic illness (e.g. well-controlled depression), or acute uncomplicated illness (e.g. exacerbation of anxiety disorder) – Diagnostic testing: psychological testing, skull film – Management: psychotherapy, environmental intervention (e.g. agency, school/vocational placement), referral for consultation Risks of significant complications, morbidity, or mortality • Moderate – 1 or more chronic illness with mild exacerbation, progression, or side effects of treatment; or 2 or more stable chronic illnesses; or undiagnosed new problem with uncertain prognosis (e.g. psychosis) – Diagnostic testing: EEG, neuropsychological testing – Management: Prescription drug management, open door seclusion, ECT (no co-morbid medical conditions) Risks of significant complications, morbidity, or mortality • High – 1 or more chronic illnesses with severe exacerbation, progression, or side effect of treatment (e.g. schizophrenia) or acute illness with threat to life (e.g. suicidal or homicidal ideation) – Diagnostic testing: lumbar puncture, suicide risk assessment – Management: drug therapy requiring intensive monitoring (e.g. benzo taper for pt in withdrawal), closed-door seclusion, suicide observation, ECT (with co-morbid medical condition), rapid IM neuroleptic administration, pharmacological restraint Other notes on MDM • Clinically, there is a close relationship between the nature of the presenting problem and the complexity of medical decision making – Patient comes in for a prescription refill: straightforward decision making – Patient comes in with suicidal ideation: decision making of high complexity Medical Decision Making Putting It All Together Need Two of Three to Qualify for Level Overall MDM Problem Points Data Points Level of Risk Straightforward Complexity (992x2) 1 1 Minimal Low Complexity (992x3) 2 2 Low Moderate Complexity (992x4) 3 3 Moderate High Complexity (992x5) 4 4 High Medical Decision Making: Diagnosis/Management Options Problem Points Problem Points Self limited or minor (maximum of 2) 1 each Established problem, stable or improving 1 each Established problem, worsening 2 each New problem, no additional work up planned (maximum of 1) 3 New problem, with additional work up planned 4 Examples of Straightforward Medical Decision-Making • Weekly weight check on patient with anorexia • Prescription refill with no examination • Routine (e.g. weekly) CBC with diff for patient taking clozapine • Advice to patient Examples of Low Complexity Medical Decision-Making • Major depression, mild (PHQ=10), with recommendation for psychotherapy • Dry mouth as a side effect to treatment with nortriptyline, patient agrees to monitor symptoms (no med adjustment) and will try to drink more water and chew sugarless gum • Stable anxiety without complications or comorbidities, continue CBT • OTC sleep aid (e.g. melatonin) for insomnia Examples of Moderate Complexity Medical Decision-Making • Patient with worsening depression. • Patient with bipolar disorder, developed mild rash with lamotrigine, which has been stopped. The rash is resolved. Pt. needs an alternative mood stabilizer. • Patient with alcohol dependence in partial remission who would like to try naltrexone. Examples of High Complexity Medical Decision-Making • Patient with suicidal ideation, new or worsening. • Patient with first psychotic break. • A patient with anorexia nervosa who is now below 85% ideal body weight. Ways to Document Complexity • • • • • • • Barriers obtaining history, additional sources Old records reviewed Labs/EKG reviewed or ordered Treatments or medications ordered Differential diagnoses Co-morbidities or underlying diseases Patient instructions given • (This is not interactive complexity code, 90785.) Putting it all together What are the codes? • 9920x (1-5), new patient, outpatient visit • 9921x (1-5), established patient, outpatient visit Office or other outpatient services: new patient • 99201 (all 3 required) – Problem-focused history (1-3 HPI elements) – Problem-focused exam (1-5 elements) – Straightforward medical decision making – CC: self-limited or minor – Typical time: 10 minutes face-to-face with patient and/or family Office or other outpatient services: new patient • 99202 (all 3 required) – Expanded problem-focused history (1-3 HPI, 1 ROS) – Expanded problem-focused exam (6-8) – Straightforward medical decision making – CC: low to moderate severity – Typical time: 20 minutes face-to-face with patient and/or family Office or other outpatient services: new patient • 99203 (all 3 required) – Detailed history (4+ HPI, 1 PFSH, 2-9 ROS) – Detailed exam (9-13) – Medical decision making of low complexity – CC: moderate severity – Typical time: 30 minutes face-to-face with patient and/or family Office or other outpatient services: new patient • 99204 (all 3 required) – Comprehensive history (4+ HPI, 3 PFSH, 10+ ROS) – Comprehensive exam (14-15) – Medical decision making of moderate complexity – CC: moderate to high severity – Typical time: 45 minutes face-to-face with patient and/or family Office or other outpatient services: new patient • 99205 (all 3 required) – Comprehensive history (4+ HPI, 3 PFSH, 10+ ROS) – Comprehensive exam (14-15) – Medical decision making of high complexity – CC: moderate to high severity – Typical time: 60 minutes face-to-face with patient and/or family Office or other outpatient services: established patient • 99211—this code is used for a service that may not require the presence of a physician/prescriber. Presenting problems are minimal, and 5 minutes is the typical time that would be spent performing or supervising these services. Office or other outpatient services: established patient • 99212 (2 of 3 required) – Problem-focused history (1-3 HPI) – Problem-focused exam (1-5 elements) – Straightforward medical decision making – CC: self-limited or minor – Typical time: 10 minutes face-to-face with patient and/or family Office or other outpatient services: established patient • 99213 (2 of 3 required) – Expanded problem-focused history (1-3 HPI, 1 ROS) – Expanded problem-focused exam (6-8) – Medical decision making of low complexity – CC: low to moderate severity – Typical time: 15 minutes face-to-face with patient and/or family Office or other outpatient services: established patient • 99214 (2 of 3 required) – Detailed history (4+ HPI, 1 PFSH, 2-9 ROS) – Detailed exam (9-13) – Medical decision making of moderate complexity – CC: moderate to high severity – Typical time: 25 minutes face-to-face with patient and/or family Office or other outpatient services: established patient • 99215 (2 of 3 required) – Comprehensive history (4+ HPI, 2 PFSH, 10+ ROS) – Comprehensive exam (14-15) – Medical decision making of high complexity – CC: moderate to high severity – Typical time: 40 minutes face-to-face with patient and/or family Documentation Requirements for Established Patient Visits 99211 99212 99213 99214 99215 CC N/A Required Required Required Required HPI N/A 1-3 1-3 4+ 4+ ROS N/A N/A Pertinent 2-9 10+ PMSF N/A N/A N/A 1 2 Exam N/A 1-5 6-8 9-13 14-15 Medical DecisionMaking N/A Straightforward Low Moderate High Time 5 min 10 min 15 min 25 min 40 min Documentation Requirements for New Patient Visits 99201 99202 99203 99204 99205 CC Required Required Required Required Required HPI 1-3 1-3 4+ 4+ 4+ ROS N/A Pertinent 2-9 10+ 10+ PMSF N/A N/A 1 3 3 Exam 1-5 6-8 9-13 14-15 14-15 Medical DecisionMaking Straightforward Straightforward Low Moderate High Time 10 min 20 min 30 min 45 min 60 min Notes about “typical time” • The specific times expressed in the visit code descriptors are averages, and therefore represent a range of times which may be higher or lower depending on actual clinical circumstances. • Face-to-face for office and outpatient • Unit/floor for hospital and inpatient • Time is not a criteria for level of service. Examples of different levels 99211 (5 min) • • • • • BP check by nurse Weight check for metabolic syndrome Lab draw Picking up prescription refill Picking up return to work or school certificate. (If mail or call in, no CPT code allowed) • May not require physician presence 99212 (10 min) • One self limited problem • 1-3 HPI elements – (no ROS) • Focused exam (1-5 elements) • Example: 1 month follow up after stopping a medication, to confirm patient is still doing well 99213 (15 min) Decision Making (low) • 2 or more self limited problems • one stable chronic illness • acute uncomplicated illness (social anxiety) History • 1-3 HPI elements • Pertinent ROS Physical • 6+ elements 99214 (25 min) Decision Making (moderate) • 1+ chronic illness with mild exacerbation • 2+ or more stable chronic illnesses • Undiagnosed new problem with uncertain diagnosis • Acute illness with systemic symptoms • Acute complicated injury History • 4 HPI elements • 2-9 ROS • 1 of 3 PFSH Physical • Detailed (affected area and related organ system) Time vs. Complexity • The PTSD exacerbation that requires two hours of office time • The patient who takes 30 minutes just to review problems, adjust medications, counsel and coordinate care – but doesn’t require an exam or complex medical decision-making Billing for time • Sometimes you can use the length of time spent face-to-face with a patient instead of using history, exam, and MDM criteria in E/M coding. Coding Based On Time • When you’ve spent the time, but the points just don’t add up • If clinician spends more than 50% of face-to-face visit counseling or coordinating patient’s care, can code based on time spent – even if hx, exam or medical decision-making elements lacking • Documentation may refer to prognosis, diff dx, risks, benefits of tx, instructions, compliance, risk reduction, or discussion with another health provider. How to do it • Documentation must state total time spent face-toface or coordinating care, what the content of that counseling or coordination was, and that more than 50% of the total time was spent in counseling or care coordination. – “20 minutes of 25 minutes face-to-face time spent counseling/coordinating care re: importance of medication compliance with mood stabilizer for bipolar disorder” – “45 minutes spent meeting with pt and Case Manager discussing plan of care for complex patient with depression and fibromyalgia” Time vs. Code Typical time New patient codes 5 min 10 min 99211 99201 15 min 20 min 99212 99213 99202 25 min 30 min Established patient codes 99214 99203 40 min 99215 45 min 99204 60 min 99205 Physician Work RVU’s (2013) New Patients 99201 - 99205 Established Patients 99211 - 99215 Level I 0.48 0.18 Level II 0.93 0.48 Level III 1.42 0.97 Level IV 2.43 1.5 Level V 3.17 2.11 Suggestions for clinicians • Assess appropriate level of care in first 5 minutes of encounter – Helps to organize the gathering of information • Organize documentation to identify the elements that support the E/M code level – CC, HPI, ROS, P/F/S Hx – Exam – Medical Decision Making/Plan Categorical Note Outline • Chief Complaint • History of Present Illness • Past Medical, Psychiatric, Family & Social History • Review of Systems • Examination • Diagnosis • Formulation/Plan of Care Review: 99213 • • • • 2+ or more self-limited or minor problems 1 stable chronic illness Acute uncomplicated illness Typically 15 minutes face-to-face with pt/family Review: 99214 • 1+ chronic illness with exacerbation • 2+ or more stable chronic illnesses • Undiagnosed new problem with uncertain diagnosis • Acute illness with systemic symptoms • Acute complicated injury • Typically 25 minutes face-to-face with pt/family What is often missing? • Most frequent deficiencies identified in audits of mental health records ① Failure to provide and record the required number of elements in the ROS for the level of history designated ② Failure to provide and record the required number of constitutional elements (including vital signs) Don’t Forget… • Submit question cards • We will answer some after lunch • Others will be answered via online support through IPS after the course. Thank you! References • Evaluation and Management Services Guide, US Department of Health and Human Services, December 2010. • Procedure Coding—Handbook for Psychiatrists, 4th Ed., C. W. Schmidt et al., APA Publishing, 2011. • American Academy of Child and Adolescent Psychiatry (AACAP) website resources www.aacap.org (useful!!)