Liver disease, bacterial and amebic abscesses, and cirrhosis of the
advertisement

MINISTRY OF HELTHCARE OF THE REPUBLIC OF UZBEKISTAN
TASKENT MEDICAL ACADEMY
APPROVED
Vice-rector for studying process
Senior Prof.
Teshaev O.R.
«_________» __________2011y
Lecture
For students of VII course of treatment faculty
By theme
LIVER DISEASES
Written on basis of tutorial
Tashkent 2011
2
APPROVED
On conference in department of surgical diseases for general practitioners
Head of department___________________senior prof Teshaev O.R.
Text of lecture accepted by CMC for GP of Tashkent Medical Academy
Report №___________from____________2011 y
Moderator senior professor Rustamova M.T.
3
The Liver
LIVER ENLARGEMENT
Physical signs
The infant's liver is normally palpable two sms below the right costal margin. It is also felt in thin
adults, particularly on deep inspiration. The enlarged liver forms a mass which extends downwards
below the right costal margin and may fill the subcostal angle or extend beneath the left costal margin in gross hepatomegaly. The mass moves with respiration, is dull to percussion and is continuous
with the liver dullness, which may itself extend above the normal upper level of the fifth right interspace.
Causes
1. Congenital
a) Riedel's lobe
b) polycystic disease
2 Inflammatory
a) infective hepatitis
b) portal pyaemia
c) leptospirosis (Well's disease)
d) actinomycosis
3 Parasitic
a) amoebic hepatitis and abscess
b) hydatid
4 Neoplastic
a) primary tumour
b) secondary deposits
5 Cirrhosis
a) portal
b) biliary
c) cardiac
d) haemochromatosis
6 Haemopoetic diseases and reticuloses
a) Hodgkln's
b) non-Hodgkin's lymphoma
c) leukaemia
d) polycythaemia
7 Metabolic diseases
a) amyloid
b) Gaucher's disease
Whenever the liver is felt, automatically the patient must be examined to detect any accompanying splenomegaly or lymphadenopathy. If the spleen is palpable in addition to the liver, consider cirrhosis, polycythaemia, leukaemia or amyloid as possible diagnoses. If, in addition, the
lymph nodes are enlarged, the diagnosis is almost certainly a lymphoma.
JAUNDICE
The normal serum bilirubin is below 9 mmol/1. Jaundice becomes clinically detectable
when the serum level rises to over 22 mmol/1.
Jaundice may result from excessive destruction of red cells (pre-hepatic jaundice), liver
damage (hepatic jaundice) or obstruction of the biliary tree (post-hepatic jaundice). Quite frequently
the hepatic and post-hepatic forms coexist; for example, a stone in the common bile duct may produce jaundice partly by obstructing the outflow of bile and partly by secondary damage to the liver
(biliary cirrhosis), and both tumour deposits in the liver and cirrhosis may result in icterus partly by
actual destruction of liver tissue and partly by intrahepatic duct compression.
Classification
Pre-hepatic jaundice:
4
Haemolytic disorders, e.g. spherocytosis, pernicious anaemia, incompatible blood transfusion
Hepatic jaundice:
1 Hepatitis (viral, leptospirosis, glandular fever)
2 Cirrhosis
3 Cholestasis from drugs, e.g. chlorpromazine
4 Liver poisons, e.g. phosphorus, carbon tetrachloride, chloroform, paracetamol overdosage
5 Liver tumours
Post hepatic jaundice:
1 Obstruction within the lumen: gallstones, parasites
2 In the wall:
(a) congenital atresia of common bile duct
(b) traumatic stricture
(c) tumour of bile duct
(d) chronic cholangitis
3 External compression;
(a) tumour of head of pancreas
(b) tumour of ampulla of Vater
(c) pancreatitis
Differential diagnosis of jaundice.
This is based on history, examination and special investigations.
History
A family history of anaemia, splenectomy or gallstones suggests a congenital red cell defect
(acholuric jaundice, etc.). Clay-coloured stools and dark urine accompanying the episodes of jaundice indicate hepatic or post-hepatic causes. Enquire after recent blood transfusions, drugs (chlorpromazine, paracetamol, methyl-dopa, repeated exposure to halothane), injections and alcohol consumption. Has there been contact with cases of virus hepatitis? What is the patient's occupation?
(Farmers and sewer workers are at risk of leptospirosis.)
Usually painless Jaundice of sudden onset with liver tenderness in a young person is viral in
origin. Attacks of severe colic, rigors and intermittency of jaundice suggest stone. Remorselessly
progressive jaundice, often accompanied by continuous pain radiating to the back, is suspicious of
malignant disease.
Examination
The colour of the jaundice is important; a lemon yellow tinge suggests haemolytic jaundice
(due to combined anaemia and mild icterus). Deep jaundice suggests the hepatic or post-hepatic
types.
Look for other signs of cirrhosis: spider naevi, liver palms, gynaecomastia, testlcular atrophy, flapping tremor, encephalopathy, splenomegaly and occasionally finger clubbing. There may
also be ascites and leg oedema, but these may be associated with intra-abdominal malignant disease
as well as cirrhosis.
Examination of the liver itself is helpful; in viral hepatitis the liver Is slightly enlarged and
tender, in cirrhosis the liver edge is firm, although the liver may be shrunken and impalpable. A
grossly enlarged, knobbly liver suggests malignant disease.
If the gallbladder is palpable and distended, it is probable that the cause of the jaundice is
not a stone (Courvoisier's law). The liver is usually smoothly enlarged in post-hepatic obstructive
jaundice.
A pancreatic tumour may be palpable or a primary focus of malignant disease may be obvious, e.g. a melanoma.
Splenomegaly suggests cirrhosis of the liver, blood disease or a lymphoma; in the latter
there may also be obvious lymphadenopathy.
Special investigations
It is easy enough to differentiate the prehepatic causes of jaundice from hepatic and post-hepatic,
5
but that the latter two are often very difficult to differentiate one from the other and, as already stated, are often associated with each other. Laboratory tests are of some help but are by no means diagnostic. Imaging techniques are valuable in visualizing the liver, gallbladder and pancreas, while
endoscopic cannulation of the bile ducts, or transhepatic duct puncture enable the bile duct system
to be outlined. However, it is not unusual for the diagnosis to be established finally only at laparotomy.
Bile pigment metabolism and excretion must be clearly understood if many of the laboratory
investigations in jaundice are to be comprehensible.
Red cells are destroyed in the reticulo-endothellal system. The porphyrin ring of the haemoglobin molecule is disrupted and a bilirubin-iron-globin complex produced. The iron is released and
used for further haemoglobin synthesis in the red marrow. The bilirubin-globin fraction reaches the
liver as a lipid-soluble, water insoluble substance. In the liver the bilirubin is conjugated with glucuronic acid and excreted In the bile as the now water-soluble bilirubin-diglucuronide.
In the bowel lumen, bilirubin is reduced by bacterial action to the colourless urobilinogen,
most of which is excreted in the faeces, in which it becomes converted to urobilin which is pigmented and which, with the other breakdown products of bilirubin, gives the stool Its normal colour.
A small amount of urobilinogen is reabsorbed from the intestine into the portal venous tributaries and passes to the liver, where most of it is excreted once more in the bile back into the gut.
Some, however, reaches the systemic circulation and this is excreted by the kidney into the urine.
When urine is exposed to air, its contained urobilinogen is oxidized to urobilin.
Bilirubin is not excreted by the kidney except in its water-soluble (conjugated) form. It is
therefore absent from the urine in pre-hepatic jaundice (hence the old term 'acholuric jaundice') although present when there Is post-hepatic obstruction.
In pre-hepatic jaundice, large amounts of bilirubin are excreted into the gut, therefore the
urobilinogen in the faeces is raised, the amount absorbed from the bowel increases and there is
therefore greater spillover into the urine.
In hepatic damage the urinary urobilinogen may also be raised because of the inability of the
liver to re-excrete the urobilinogen reabsorbed from the bowel.
In post-hepatic obstruction, very little bile can enter the gut, therefore the urobilinogen must
be low in both the faeces and the urine.
The important laboratory findings in the various types of jaundice can now be summarized.
Urine
The presence of bilirubin indicates obstructive jaundice, either intra- or post-hepatic.
Excess of urobilinogen indicates pre-hepatic jaundice or sometimes liver damage, whereas
an absence of urobilinogen suggests obstructive causes.
Faeces
Absence of bile pigment indicates intra: or post-hepatic causes. The faecal urobilinogen is
raised in pre-hepattc jaundice. The occult blood test may be positive, either on account of oozing
oesophagcal varices secondary to portal hypertension (Indicating cirrhosis), or due to an ampullary
carcinoma which is occluding the orifice of the common bile duct and also bleeding into the duodenum.
Blood
Full haematologlcal investigations (RBC fragility. Coombs' test, retlculocyte count) confirm
haemolytic causes.
The serum bilirubin is Invariably raised. It is rarely higher than 100 mmol/l in pre-hepatic
jaundice, but may be considered higher in obstructive cases. In late malignant disease it may exceed
1000 mmol/1 (50 mg per cent). In pre-hepatic jaundice bilirubin is present in the unconjugated
form. In the pure post-hepatic obstructive jaundice the bilirubin is mainly in the conjugated form,
whereas in hepatic jaundice it is present In the mixed conjugated and unconjugated forms due to a
combination of liver destruction and intra-hepatic duct blockage.
The alkaline phosphatase is normal in pre-hepatic jaundice (90 to 330 mmol/1), raised in
6
hepatic jaundice, and considerably raised (above 600 iu/1) in post-hepatic jaundice and in primary
biliary cirrhosis.
Serum proteins are normal in pre-hepatic jaundice, have a reversed A:G ratio with depressed
albumin in hepatic jaundice and are usually normal In post-hepatic jaundice, unless associated with
liver damage.
Serum tronsaminases are raised in acute viral hepatitis and in the active phase of cirrhosis.
The prothrombin time is normal in pre-hepatic jaundice, prolonged but correctable with Vitamin K in post-hepatic jaundice (where functioning liver tissue is still present) and prolonged but
not correctable in advanced hepatic jaundice, where not only is absorption of fat-soluble Vitamin K
impaired but also the damaged liver is unable to synthesize prothrombin.
Ultrasound and CT scanning
These are extremely useful as well as non-invasive. Gall stones within the gall bladder can
be demonstrated with a high degree of accuracy. Unfortunately, stones within the bile ducts often
fail to visualize. Dilatation of the duct system within the liver is a good indication of duct obstruction, so that if the ducts are not dilated, an obstructive cause for the jaundice is unlikely. Both techniques are valuable in the demonstration of intrahepatic lesions (e.g. tumour deposits. abscess,
cyst), which may then be accurately needled for biopsy material under scan control. A mass in the
pancreas can usually be demonstrated, but differentiation between carcinoma and chronic pancreatitis is difficult.
X-rays.
A plain X-ray of the abdomen may show gallstones (10 per cent are radio opaque). Cholecystography is useless when the patient is jaundiced since the dye is not excreted by the damaged
liver. A barium swallow may confirm the presence of oesophageal varices in jaundice due to cirrhosis, or the subsequent barium meal may reveal a distorted duodenum (suggesting a pancreatic tumour) or the presence of a primary neoplasm of the stomach. In some instances of obstructive jaundice a pre-operative trans-hepatic cholangiogram is performed by direct puncture of a dilated biliary
radicle in order to locate the exact site of the obstruction. This should be undertaken Immediately
prior to surgery since bile leakage is common when the needle is withdrawn in obstructed cases. A
useful investigation is retrograde cholanglography via a catheter introduced into the ampulla of Vater under direct vision via a fibre-optic duodenoscope. A periampullary tumour is also directly visualized at this examination.
Both transhepatic and retrograde cholangiography may be used to introduce dilators and
stents into the biliary duct system.
Liver isotope scanning. A gamma-emitting isotope which is excreted in the bile is injected,
either I131 labelled Rose Bengal, or H1DA, which is taken up by the hepatocytcs and excreted in
the bile, or colloidal technetium, which is incorporated into the macrophage Kupffer cells. Lesions
which do not contain functioning liver tissue, such as tumour deposits, abscesses or cysts, appear as
defects on the scan.
Needle biopsy. If the ultrasound scan reveal no dilatation of the duct system, an obstructive
lesion is unlikely and needle biopsy of the liver will give valuable information regarding hepatic pathology (e.g. hepatitis or cirrhosis). If the ultrasound demonstrates focal lesions in the liver, a biopsy can be obtained under scanning control. Needle biopsy is potentially dangerous in the presence
of jaundice. The prothrombin time, if prolonged, should first be corrected by administration of vitamin K. Should bleeding occur following biopsy, an immediate laparotomy may be necessary.
Laparotomy. Since most causes of post-hepatic obstructive jaundice can be relieved surgically, it may be necessary to submit a doubtful case to laparotomy even though it is suspected that
the aetiology is entirely hepatic, lest an easily remediable condition (e.g. stones in the common bile
duct) is overlooked.
CONGENITAL ABNORMALITIES. Riedel's lobe is a projection downwards from the right
lobe of the liver of normally functioning liver tissue. It may present as a puzzling and symptomless
abdominal mass.
Polycystic liver may reach a very large size but the remaining liver functions normally. It
7
may be associated with polycystic disease of the kidneys and pancreas.
LIVER TRAUMA. This may be due to penetrating wounds (gunshot or stab), or closed
crush injuries, often associated with fractures of the ribs and injuries to other intra-abdominal viscera, especially the spleen. Severe abdominal trauma is becoming increasingly common and accurate pre-operative diagnosis of the source of the haemorrhage may be impossible.
Clinical features
Following injury, the patient complains of abdominal pain. Examination reveals generalized
abdominal tenderness together with the signs of progressive bleeding. CT scanning, if available, can
be very helpful in showing the lesion and differentiation from a ruptured spleen. Occasionally there
is delayed rupture of a subcapsular haematoma, so that abdominal pain and shock may not be in evidence until some hours after the initial injury.
Treatment. If the patient's vital observations are stable, the condition can be managed conservatively with blood transfusion and careful observation. However, bleeding often continues and
there is the risk of overlooking damage to other viscera. In such cases, laparotomy is performed.
Minor liver tears can be sutured. If bleeding continues, the relevant main hepatic arterial branch
should be tied. If this does not control bleeding, major hepatic lobar resection may be necessary.
Temporary packing of the injury with a gauze pack, removed after 48 hours, may be life-saving in
severe trauma when the patient's condition is deteriorating. Antibiotic cover must be given because
of the danger of infection of the devitalized liver. Liver transplantation may be needed to manage
gross trauma to both lobes.
ACUTE INFECTIONS OF THE LIVER
Possible sources of infection are:
1 Arterial, as part of a general septicaemia — this is unusual.
2 Portal, from an area of suppuration drained by the portal vein.
3 Biliary, resulting from an ascending cholangitis.
4 Spread from adjacent infection, e.g. subphrenic abscess or acute cholecystitls.
PORTAL INFECTIONS
Portal pyaemia (pyelophlebitis)
Infection may reach the liver via the portal tributaries from a focus of intra-abdominal sepsis, particularly acute appendicitis or diverticulitls. Multiple abscesses may permeate the liver; in
addition there may be septic thrombi in the intra-hepatic radicles of the portal vein, and infected clot
in the portal vein itself. The condition has become very rare since the advent of antibiotics.
Clinical features
The condition should be suspected in patients who develop rigors, high hectic temperature, a
tender palpable liver and jaundice after any acute infective abdominal condition.
Special investigations
A blood culture should be carried out before treatment is commenced; it is often is positive.
Whenever a space occupying lesion of the liver is suspected, ultrasound or CT scanning
should give confirmation and localization.
Treatment. Comprises antibiotic therapy. Occasionally a large, single abscess may require
drainage. This may be carried out percutaneously under ultrasound control.
Actinomycosis. Actlnomycosis of the liver is a rare variety of portal infection; spread via the
portal blood stream from ilco-caecal actinomycosis.
Amoebic hepatitis. Another special variety of portal infection, secondary to an Entamoeba
histolytica infection of the large intestine. In severe infection the cytolytic enzyme produced by the
amoebae destroys the liver tissue producing an amoebic abscess, which Is sterile, although amoebae
may be found in the abscess wall.
A liver CT scan and ultrasound are the most valuable special investigations.
Treatment. The majority respond to medical treatment with metronidazole, which has replaced emetine as the drug of choice. Ultrasonographlcally directed percutaneous drainage is required infrequently in non-responding cases.
BILIARY INFECTION. Multiple abscesses in the liver may occur in association with se-
8
vere suppurative cholangitis secondary to impaction of gallstones in the common bile duct. Clinically the features are those of Charcot's Intermittent hepatic fever — pyrexia, rigors and jaundice.
Renal failure may occur (the hepato-renal syndrome).
Treatment. Antibiotic therapy is commenced (checked, where possible, against the bacteriology of the bile). Urgent drainage of the bile ducts is performed, either by open operation or, more
usually, by endoscopic sphlncterotomy. Fluid replacement and mannitol given intravenously guard
against renal failure.
HYDATID DISEASE OF THE LIVER.
The liver is the site of 75 per cent of hydatid cysts in man.
Pathology. Dogs are Infected with the ova of Echinococcus granulosis (Taenia echinococcus) as a result of eating sheep offal. The tapeworms develop in the dog's intestine from whence ova
are discharged in the faeces. Man (as well as sheep) ingests the ova from contaminated vegetables,
etc.; the ova penetrate the stomach wall to Invade the portal tributaries and thence pass to the liver.
Hydatid disease is therefore common in sheep rearing communities, e.g. Australia, Iceland, Cyprus,
Southern Europe, Africa and Wales. Public health measures, e.g. destruction of stray dogs, has resulted in a marked drop in Incidence. The cyst consists of:
1 An adventitia: comprising the fibrous coat of the host's reaction.
2 A laminated membrane: white elastic material derived from the cyst itself.
3 Germinal epithelium: upon which brood capsules develop.
4 Cyst fluid: which is clear unless secondarily infected and which contains booklets and
scolices derived from the daughter cysts.
Clinical features. A cyst may present as a symptomless mass. The contents may die and the
walls become calcified so that this inactive structure may be a harmless post-mortem finding.
The active cyst may, however:
1. Rupture into the peritoneal cavity, pleural cavity, alimentary canal or biliary tree.
2. Become infected.
3. Press on intra-hepatic bile ducts and produce obstructive jaundice, although jaundice Is
much more often due to intrabtliary rupture and release of cysts into the bile ducts.
Investigations
1. Plain X-ray of the liver may show a clear zone produced by the cyst, or may show flecks
of calcification in the cyst wall.
2. Ultrasound and CT scan are Invaluable in localizing the cyst.
3. Serological tests depend on the sensitlzation of the patient to hydatid fluid, which contains a specific antigen, leakage of which Induces the production of antibodies. Among the various
test now available, hydatid immuno-electro-phoresis is the one of choice. This depends on the formation of a specific arc of precipitation produced by the interaction of the serum from the hydatid
patient with the antigen as compared to a control.
4. There may be eoslnophilia, which is not specific but should at least arouse clinical suspicion.
Treatment. A calcified cyst should be left alone. Other cysts should be treated to prevent
complications. Treatment with albendazole may result in shrinkage or even disappearance of the
cysts. Failure to respond or the presence of complications are indications for surgery. The cyst is
exposed and aspirated. It is then possible to excise the cyst, working in the plane between the fibrous adventitia and the laminated membrane, taking care not to liberate daughter cysts.
VIRAL HEPATITIS
Aetiology. There are several separate viral agents.
1. The infective hepatitis (type A) virus, which has an incubation period of 2 to 6 weeks and
is spread by nasal droplets and faeces. Children or young adults are usually affected.
2. The serum hepatitis (type B) virus, with an incubation period of 6 weeks to 6 months and
which is transmitted by inoculation with contaminated syringes or a transfusion of blood or plasma
from an Infected patient. The blood in these subjects contains the Australia antigen and is highly infective. Any age may be Infected.
9
3. Type C. Similar in transmission to type B, both of which can lead to chronic infection,
cirrhosis and tumour formation.
Clinical features. There Is a prodromal period of a few days with anorexia, aversion to tobacco, fever, malaise, nausea and vomiting. The patient then becomes jaundiced with dark urine
and clay coloured stools. There may be upper abdominal pain, although this is usually not marked.
The liver is palpable and tender. The great majority recover in up to 4 weeks, treated simply by bed
rest and a low fat diet. Alcohol should be avoided for 12 months; not only is the patient unusually
susceptible to intoxication but the liver is vulnerable to damage by alcohol.
Complications.
1. Hepatic failure, massive necrosis (acute yellow atrophy), with extremely high mortality,
is fortunately rare, about 2 per 1000 cases.
2. Relapse, which may occur a few weeks after the Initial episode.
3. Post-hepatic cirrhosis.
Patients with positive Australia antigenaemia are a risk to nursing, laboratory and medical
staff, especially if multiple venepunctures or surgery are required. All hospital workers should be
protected by vaccination. The danger to unprotected non-immunized staff can be lessened by the
administration of convalescent gamma-globulin given at, or shortly after, the time of exposure.
Great care must be taken in handling blood or in operation on these patients, since the virus can
gain access via minute and unrecognized cuts or pin pricks and probably also through the intact
mucosa of the mouth, genital tract, respiratory tract and conjunctiva.
CIRRHOSIS.
Definition. A group of conditions in which there is chronic hepatic injury; healing occurs
by regeneration and flbrosls. Fibrosis leads to further cell damage and destruction of hepatic architecture progressing to liver failure and portal hypertension.
Aetiology
A convenient classification of the cirrhoses is:
1 Portal:.
(a) alcoholic
(b) nutritional (deficient protein diet)
(c) post-hepatic
(d) idiopathic
2 Biliary:
(a) primary (Hanoi's cirrhosis); an auto-immune disease with raised serum antimitochondrial antibodies
(b) secondary to prolonged biliary obstruction
3 Cardiac: in severe chronic congestive failure
4 Other causes:
(a) chronic active hepatitis. An auto-immune disease
(b) haemochromatosis
(c) hepatolentlcular degeneration (Wllson-Konovalov's disease)
(d) schistosomiasis
In countries with a high consumption of alcohol (France and USA), alcohol is the commonest aetiological factor. In the tropics schistosomiasis heads the list (Egyptian splenomegaly). In
Great Britain 50 per cent of cirrhosis cases are alcoholic.
PORTAL HYPERTENSION
The normal portal pressure Is between 80 and 150 mm of water. In portal hypertension this
pressure may be raised to 500 mm or more.
Aetiology
Portal hypertension results from an obstruction in the portal tree. The causes are classified
according to the site of the block:
1 Pre-hepatic obstruction of the portal venous Inflow Into the liver):
(a) congenital malformation of vessel
10
(b) spreading portal vein thrombosis in the neo-natal period from an umbilical infection
(c) occlusion by tumour or pancreatitis
2 Hepatic (obstruction of the portal flow within the fiver): the cirrhoses.
3 Post-hepatic obstruction of the hepatic veins: Budd-Chiari syndrome:
(a) Idiopathic hepatic venous thrombosis In young adults of both sexes. A possible complication of oral contraceptives in women. In many cases there is an underlying haematological neoplasm for example, polycythemia or mono-clonal gammaglobulinopathy.
(b) congenital obliteration
(c) blockage of hepatic vein by tumour Invasion
By far the commonest cause of portal hypertension is cirrhosis, yet there is no strict relationship between the severity of the liver disease and the extent of portal hypertension, which is not
therefore entirely explained on the basis of mechanical obstruction.
Pathological effects
The 2 important effects of portal hypertension are:
1 The development of a collateral portal-systemic circulation.
2 Splenomegaly.
In course of hepatic insufficiens: ascitis, the manifestations of hepatic failure (in severe cirrhosis).
Collateral channels
Portal obstruction results in the development of collateral channels between the portal and
systemic venous circulations. These are:
1 Between the left gastric vein and the oesophageal veins, forming oesophageal varices; the
largest and clinically the most important connections.
2 Between the superior and inferior rectal veins with development of haemorrhoids, which
are true varices.
3 Along the obliterated umbilical vein to the superior and inferior epigastric veins (caput
medusae).
4 Retroperitoneal and diaphragmatic anastomoses, which present technical hazards to the
surgeon at time of operation.
The oesophageal varices, and to a much lesser extent the haemorrhoids, may result in gastro-intestinal haemorrhage, which is the most serious complication of portal hypertension per se.
Splenomegaly
Progressive splenic enlargement occurs as a result of portal congestion together with some
degree of hypertrophy of the splenic substance itself. This is often associated with the haematologlcal changes of hypersplenism — leucopenia and thrombocytopenia. Anaemia accompanying
Splenomegaly can be accounted for entirely by gastro-intestinal bleeding and is not a result of
splenic enlargement.
Ascitis
This is due to a combination of factors. The raised portal pressure itself increases transudation of fluid into the peritoneal cavity but alone will not produce ascltes, which Is not therefore seen
in the pre-hepatic obstruction. Liver damage results In a low serum albumin, therefore a low plasma
osmotic pressure and consequent deficient reabsorptlon of ascltic fluid. Liver damage is associated
with increased aldosterone activity with sodium retention. Increased lymphatic pressure in the cirrhotic liver results in lymph transudation from the liver surface, and this high lymphatic pressure is
also a feature in the post-hepatic block.
The effects of liver failure
1 Jaundice.
2 CNS effects — mental changes, flapping tremor and hepatic coma. This portal-systemic
encephalopathy is brought about by a shunt of nitrogenous breakdown products from the intestine
via the portal tract into the systemic circulation without the Interposition of the hepatic detoxicating
filter.
11
3 A group of features of, as yet, uncertain aetiological significance — gynaeco-mastia, testlcular atrophy, amenorrhoea, spider naevi, finger clubbing and palmar erythema ('liver palms').
Clinical features
To the surgeon portal hypertension presents as three groups of problems:
1 As a differential diagnosis of jaundice or hepatomegaly.
2 As a cause of gastrolntestinal haemorrhage.
3 As one of the causes of ascltes.
Investigations
In addition to history and examination (which includes a careful search for the stigmata of
liver disease) the following investigations are indicated:
1 Barium swallow to demonstrate the presence of oesophageal varices.
2 Fibreoptic endoscopy will demonstrate varices and differentiate between bleeding from
this source and from a peptic ulcer or multiple gastric erosions, both of which are common in patients with cirrhosis.
3 Liver function tests, together with liver biopsy if necessary.
4 A splenic venogram or the venous phase of a selective superior mesenteric arteriogram to
delineate the exact site of the portal obstruction before elective surgery Is undertaken.
Treatment
The mere demonstration of oesophageal varices on a barium swallow is not an indication for
surgery. Nothing more is required than treatment of the underlying condition on medical lines, e.g.
cirrhosis is managed by a high calorie, well-balanced diet with added protein in malnourished patients (provided liver damage Is not severe), and with avoidance of precipitating factors such as alcohol. Surgical intervention Is only Indicated if haemorrhage occurs.
The management of haemorrhage from oesophageal varices.
This is particularly dangerous, especially in patients with liver damage. In these subjects the
liver is further injured by the hypotension of blood loss, and portal-systemic encephalopathy may be
precipitated due to the absorption of large amounts of nitrogenous breakdown products from the
'meal of blood' within the Intestine. Prognosis is better in the small group of patients with normal
liver function and a prehepatic block.
An attempt must be made to confirm the diagnosis. The presence of established liver disease, an enlarged spleen and proven varices does not necessarily mean that bleeding Is from the varices. Such patients are prone to bleed from gastric erosions and are commonly affected by peptic ulceratlon. Fiberoptic endoscopy should always be performed In order to visualize the bleeding point
and to exclude non-variceal haemorrhage. Bleeding varices are injected directly with sclerosant solution. Active bleeding may, however, prevent a satisfactory view at endoscopy.
The Immediate treatment of haemorrhage is blood replacement by transfusion. Nitrogenous
absorption from the bowel is reduced by emptying as much as possible of the blood from the colon
by means of an enema, giving neomycin by mouth to reduce bacterial decomposition of blood in the
gut, withholding protein from the diet and maintaining nourishment by means of glucose given by
mouth or Intravenously. If bleeding continues, more vigorous methods may be required, but here
careful decision must be taken; if the patient is in advanced hepatic failure with jaundice, ascitis, a
low serum albumin. Impaired clotting, thrombocytopenia and precoma or coma, then It is wise
practice to refrain from further treatment since the prognosis Is hopeless and further procedures
merely add to the discomfort of an already dying patient.
In fitter subjects, the haemorrhage is stemmed either by:
1 Direct pressure on the varices using a Sengstaken tube which is Introduced through the
mouth Into the oesophagus and cardia, then distended, or
2 Intravenous Pitressin (20 units by slow intravenous Injection), Remestipe, sandostatin,
which produces a marked fall In portal venous pressure and temporary cessation of bleeding by
mesenteric arteriolar constriction. Therapeutic doses cause Intestinal colic. The emergency surgical
procedures are: Probe of Blakemore-Sengstaken.
Blakemore-Sengstaken tube. Balloons in the oesophagus and in the cardia compress the
12
bleeding varices; the gastric tube can be used either for aspirating the stomach or for feeding purposes.
1 Trans-thoracic ligation of the varices, which is effective for varices limited to the oesophagus.
2 Porta-caval anastomosis between the portal vein and the inferior vena cava, which shunts
the portal blood directly into the venous systemic circulation and thus lowers the portal, pressure.
3 Injection of the varices via a long needle Introduced through a rigid or fibre-optic oesophagoscope. This technique is analogous to the injection treatment of piles. This procedure can stop
bleeding with minimal trauma to the patient although there are the risks of perforation of the oesophagus and repeated injections may produce ulceration or fibrosis. Control of the bleeding allows
the surgeon to assess the patient as a candidate for liver transplantation. Laparotomy should be
avoided if possible if a subsequent transplant is planned, since the resulting vascular adhesions will
greatly add to the dangers of the transplant operation. If the patient is not a candidate for a transplant, then definitive surgery to prevent further bleeding may be contemplated. This may comprise:
4 Porta-azygos disconnection, in which the varices around the lower end of the oesophagus
and the upper stomach are divided at the cardio-oesophageal junction using the circular stapling
gun, in order to interrupt the communications between the two systems of veins within the wall of
the lower oesophagus.
5 If the portal vein itself is occluded by a thrombus or is congenitally abnormal, porta-caval
anastomosis is impossible. The portal system can be shunted to the systemic system by a variety of
techniques, spleno-renal anastomosis between the splenic vein (after splenectomy) and the left renal
vein is that most often performed.
The types of decompression shunt.
(A) End to side porta-caval shunt, the most straightforward procedure.
(B) Side to side porta-caval shunt, If the venous outflow of the liver is blocked and blood is
leaving the liver from the portal vein.
(C) The end to side spleno-renal shunt with splenectomy.
(D) The mesocaval H- shunt is indicated when a side to side shunt is Impossible, for example, when the portal vein is blocked.
(E) The distal spleno-renal Warren shunt is designed to reduce selectively the blood pressure
in the oesophageal varices, decompression occurs via the short gastric veins and splenic vein into
the renal vein.
6 TIPS – transdermal intrahepatic systemic shunt.
Portal-systemic shunting may be performed in the elective stage when there have been previous episodes of haemorrhage. Such procedures again should only be carried out in patients with
reasonable hepatic function. Jaundice, plasma albumin of less than 25 g/1 and poor general condition are contra-indications to surgery.
Unfortunately, operative procedures in which an anastomosis is made between the portal
and systemic circulations are likely to precipitate portal-systemic encephalopathy and such patients
often have to be maintained indefinitely on a low protein diet. However, liver transplantation is now
a preferable option except in cases of prehepatic obstruction with good liver function.
Treatment of ascites
1 Paracentesis gives immediate relief if discomfort is intense, but It has the disadvantage
that the patient loses protein.
2 Low sodium, high protein diet, Intravenous albumin.
3 Diuretics: chlorothiazide (with potassium supplement) and
4 Peritoneo-venous shunt (LeVeen or Denver): a silicone rubber catheter with a pressureactivated valve, which shunts ascitic fluid from the peritoneal cavity back Into the venous systems
via the internal jugular vein.
5 Surgery: only occasionally Indicated; a few patients may be fit enough for porta-caval
anastomosis which sometimes relieves ascites.
6 Angiography – embolisation of vein according intravessel pressure.
13
LIVER NEOPLASMS
Classification
Benign (rare)
(a) cavernous haemangloma
(b) adenoma
Malignant
1 Primary:
(a) hepatoma
(b) cholangiocarcinoma
2 Secondary (common):
(a) portal spread (from alimentary tract)
(b) systemic blood spread (from lung, breast, testis, melanoma, etc.)
(c) direct spread (from gall bladder, stomach and hepatic flexure of colon)
Hepatoma
About 50 per cent occur in cirrhotics, especially those with nutritional deficiencies, and Is
common in Central Africa (50 per cent of cancer deaths) and the Far East associated with hepatitis
B and C infection.
The tumour forms a large, solitary mass, or there may be multiple foci throughout the liver.
Spread occurs through the liver substance and metastasis outside this organ is late.
Clinically there is massive liver swelling which develops in a cirrhotic. Blood-stained ascites collects and there is a rapid downward course.
Cholangiocarcinoma
Much less common (20 per cent of primary tumours); an adenocarclnoma arising from the
intrahepatic bile duct system which may complicate chronic sclerosing cholangitis. It usually presents with jaundice. Spread occurs directly through the liver substance with a fatal outcome.
Secondaries
The liver is an extremely common site for secondary deposits, which are found in about one
in three post-mortems carried out on patients who have died of advanced malignant disease. Necrosis at the centre of metastases lead to the typical umbillcation of these tumours.
The clinical effects of secondary deposits in the liver are:
1. Hepatomegaly: the liver is large, hard and irregular.
2. Jaundice: due to liver destruction and intrahepatic duct compression.
3. Hepatic failure
4. Portal vein obstruction: producting oesophageal varices and ascites.
5. Inferior vena cava obstruction: producing leg oedema.
Treatment. A primary hepatoma, confined to one lobe, can be treated by hepatic lobectomy.
It may be possible to relieve the jaundice in Cholangiocarcinoma by passing a plastic tube upwards
along the common bile duct through the growth into the dilated radicles above the obstruction or
downwards by a percutaneous intubation. This relieves the jaundice often for months and occasionally for more than a year.
In young people with a primary hepatic tumour confined to the liver, liver transplantation
has proved to be a valuable form of treatment.
Resection of secondary tumours is seldom of value but may be considered when Isolated
deposits are confined to one lobe. Pain may be relieved by ligation of the hepatic artery and occasionally temporary response follows the use of cyto-toxic drugs.
PARASITIC DISEASES OF A LIVER
Actinomycosis.
Actinomycosis of the liver is a rare variety of portal infection; spread via the portal
14
blood stream from ilco-caecal actinomycosis. Treatment is medicamentous (actinolizat) + surgical (resection of liver).
Amoebic hepatitis
Another special variety of portal infection, secondary to an Entamoeba histolytica infection of the large intestine. In severe infection the cytolytic enzyme produced by the amoebae destroys the liver tissue producing an amoebic abscess, which is sterile, although amoebae
may be found in the abscess wall.
A liver CT scan and ultrasound are the most valuable special investigations.
Treatment
The majority respond to medical treatment with metronidazole, which has replaced
emetine as the drug of choice. Ultrasonographlcally directed percutaneous drainage is required
infrequently in non-responding sheaths.
HYDATID DISEASE OF THE LIVER
Tractology
Dogs are infected with the ova of Echinococcus granulosis (Taenia echinococcus) as a
result of eating sheep offal. The tapeworms develop in the dog's intestine from whence ova are
discharged in the faeces. Man (as well as sheep) ingests the ova from contaminated vegetables,
etc.; the ova penetrate the stomach wall to Invade the portal tributaries and thence pass to the
liver. Hydatid disease is therefore common in sheep rearing communities, e.g. Australia, Iceland, Cyprus, Southern Europe, Africa and Wales. Public health measures, e.g. destruction of
stray dogs, has resulted in a marked drop in Incidence. The cyst consists of:
1. An adventitia: comprising the fibrous coat of the host's reaction.
2. A laminated membrane: white elastic material derived from the cyst itself.
3. Germinal epithelium: upon which brood capsules develop.
4. Cyst fluid: which is clear unless secondarily infected and which contains booklets
and scolices derived from the daughter cysts.
The liver is the site of 75 per cent of hydatid cysts in man.
Single-chamber (hydatidous) echinococcus is the heavy parasitic disease concerning to
larval helmintosises. In connection with significant number of patients and existence endemic
areas echinococcosis represents a serious medical and economic problem for many countries
of the world. For the first time the term "echinococcus" is entered into medical practice in
1801 Rudolph. In translation from the Greek language echinococcus means the echinoid or
brushy worm. The given tractology is known from an antiquity. Hyppocrates informed about
water bubbles, which met in internal organs of domestic animals. Galen wrote, that water bubbles were marked in a liver more often. However, only in middle of XIX century the cycle of
development of the parasite causing this disease became known. The tape worm (Echinococcus granulosus Rudolphi) in adult stages lives in a small intestine of the wolf, the jackal or a
dog, and in a stage of larvas parasitizes in organs and tissues of horned livestock and the person.
Besides exists alveolar echinococcosis (Echinococcus multilocularis, alveolans), caus-
15
ing in the person alveococcosis. The final owner of this parasite are foxes and arctic foxes. The
morphology of liver alveococcosis for the first time was described by R.Virhov in middle of
the last century, however was established much later, that hydatidous and alveolar echinococcosis is caused very similar, but with biologically various parasites thus basically differ them
larval stages which named larvocystes.
As a rule, infection of the person single-chamber echinococcus occurs from dogs, and
also after eating the half-baked liver containing elements of echinococcus cyst. Eggs of the
parasite get in an organism of the person in the basic through a digestive tract. Then a current
of blood soaks them up also and lymph carried in one or several organs, and around of oncosphere develops echinococcus cyst, covered chitinous or cuticular membrane. Around of developing cyst the fibrous capsule is formed. Between a fibrous capsule and a chitinous environment there is a space filled with lymph from which the parasite receives nutrients. More often echinococcus cyst develops in a liver. It is caused by that from a digestive tract oncosphera
gets in system of portal vein and settles in a liver. Though echinococcus may be struck any organ. There is also an aerogenic way of infection, and also through a wound at a sting of the
person an animal suffering echinococcosis. In process of growth cyst in a liver there is not only
compressing sites of a liver, but their atrophy. The destruction echinococcus comes at suppuration or a hemorrhage in cyst, perforation or traumas of cyst, and also dying of the parasite from
old age (average life expectancy cyst changes from 10 till 20 years).
The clinical picture of liver echinococcosis depends on a stage of illness, complications
and of some other reasons. In some cases long asymptomatic current is marked. In other situations quickly there comes deterioration of the general condition and clinic is divided on three
stages (period). The first stages proceed from invasion the parasite before occurrence of the
first symptoms. The second stage occupies the period from occurrence of the first complaints
before complications echinococcosis. To the third stage concern displays of complications of
echinococcus cyst (a suppuration, perforation, calcification, break in a cavity or organ).
At development cyst the immune system of the patient suffers first of all. Causeless
weakness begins to disturb patients, apparently, and work capacity is broken. They frequently
suffer catarrheal diseases. Then there are blunt pains, and also feeling of weight, pressure or
constraint in the right hypochondrium. Weakness accrues, appetite is worsened and loss of
weight of a body begins. There may be allergic reactions as nettle-rash, a diarrhea, vomiting.
At compressing by cyst inside or outhepatic bile ducts the jaundice may arise. At suppuration
cyst pains in the right hypochondrium amplify, the body temperature till 40-41°С which carries hectic character. The intoxication accompanying tremendous chills and down-pour then
quickly progresses. Break of an abscess in a pleural cavity, and also in retroperitoneal space is
probable. Sometimes cyst may be emptied in one of the next organs - a stomach, gut, a bronchial tube, gallbladder, intrahepatic bilious ways.
At diagnostics of echinococcosis the liver should take into account, that persons of efficient age (20-50 years) is more often fall ill. More frequently amazed inhabitants of rural areas and endemic regions. At palpation the increase of a liver, as a rule, is marked. It is necessary
to take into account, that pathological process is more often located in the right lobe of a liver.
Taking into account, that the beginning of this disease to establish very difficultly except for
16
detailed acquaintance with clinic echinococcosis. It is necessary to know and use modern diagnostic methods. Survey x-ray allows to establish only indirect attributes of defeat of a liver:
increase in the sizes of a liver, high standing and deformation of a dome of a diaphragm, calcify of cystic walls. Earlier isotope methods were widely used: scintigraphy and scanning of a
liver. Now a wide circulation have received ultrasonic and computer tomography. With the
help of ultrasonic in 90% of cases is diagnosed echinococcus cyst of liver. At the same time
only on the basis of ultrasonic it is sometimes difficult to differentiate echinococcosis with
congenital cysts, abscesses of a liver and others parasitic suppurative cysts. Therefore are applied serologic reactions. The laparoscopy is carried out under indications. In 1912 the Italian
researcher Casoni with the purpose of diagnostics echinococcosis began to use the special test.
He entered to patient's echinococcus allergen and caused allergic reaction. Now are used serologic reactions: latex-agglutinations, double diffusion in gel, indirect hemagglutination, immunofluorescention, etc. At these reactions diagnosticum prepare from native antigene. Test of
Amphilogov: after palpation of lamp eosynophylia enlarge. A combination of ultrasonic, serologic reactions and a computer tomography solve all questions of differential diagnostics. At
echinococcosis, complicated with a mechanical jaundice, it is used endoscopic retrograde pancreatocholangiography. With help of endoscopic retrograde pancreatocholangiography the reason of a jaundice is established. Most frequently last is caused by corking of bile ducts by elements echinococcus or compressing by cyst. Also it is used transdermal transhepatic cholangiography under the control of ultrasonic convex sensor. During time of endoscopic retrograde
pancreatocholangiography it is possible to carry out under indications endoscopic papillosphyncterotomy and to remove from common bile duct an elements of the parasite, having removed thus the reason of an jaundice.
Treatment of liver echinococcosis - only surgical. Till now there are no radical conservative actions in struggle against the implantating parasite. Besides the destruction of echinococcus is not treatment for the patient. As a rule, in this phase there are various complications: a suppuration, perforation or haemorrhages in echinococcus cyst, portal hypertension,
etc. There are some kinds of operative interventions. The choice of a method of intervention
depends on a degree of defeat of a liver and a abdominal cavity, and also from the common
condition of the patient. If the condition of the patient allows, all pathological centers leave
simultaneously. At high operational risk operation can be carried out to two - three stages.
Classification of operative interventions at echinococcosis a liver (O.B.Milonov
(1974)).
1. A lobe or segmentary resection of a liver together with cyst of echinococcus.
2. Echinococcectomy - removal of all elements of the parasite (contents of cyst, germinative and chitinous coats after opening its gleam. Operation is carried out with measures of
strict preventive maintenance semination of elements of the parasite of surrounding bodies and
tissues. For leak-proof evacuation content of cyst and introductions of an antiparasitic preparation it is used special cystotom. Thus the most effective preparation is 80%-s' glycerin with a
10-minute exposition in residual cavities.
3. Ideal echinococcectomy – removal of cyst without damage of a chitinous coats.
4. Pericystectomy. This operation is carried out at partial calcification of a fibrous cap-
17
sule and demands application of precision technics (technical equipment) or clipping according
to an arrangement of vessels and bile ducts. The prevention of formation of purulent fistulas is advantage of pericystectomy in comparison with usual echinococcectomy.
There are some ways of liquidation of a residual cavity after echinococcectomy. Capitonage, or suturing of cavities of a liver, can be complicated because of the expressed dense fibrous capsule. It was applied tamponage of a residual cavity an omentum on a leaving leg,
sticking up by biological glue, marsupialization, etc. Last years began to be applied special
sponge-like films, densely fixed on wound surfaces of a liver.
5. Echinococcotomy - opening of a cavity cyst by a section of coats. This operation was
applied, basically, at complicated cysts.
At the mechanical jaundice caused by stricture of bile ducts, plastic interventions, and
also formation of biliodigestive anastomoses are carried out, is frequent with transhepatic
lrainage. Special difficulties arise at alveococcosis with defeat of a gate of a liver. In these situations various interventions from draining operations up to hemihepatectomy are made. Last
years in connection with development of surgical hepatology operations are successfully carried out at plural widespread of echinococcosis and alveococcosis a liver and other bodies of a
belly cavity.
Clinical features
A cyst may present as a symptomless mass. The contents may die and the walls become calcified so that this inactive structure may be a harmless post-mortem finding.
The active cyst may, however:
1. Rupture into the peritoneal cavity, pleural cavity, alimentary canal or biliary tree.
2. Become infected.
3. Press on intra-hepatic bile ductsand produce obstructive jaundice, although jaundice
Is much more often due to intrabtliary rupture and release of cysts into the bile ducts.
Investigations
1. Plain X-ray of the liver may show a clear zone produced by the cyst, or may show flecks
of calcification in the cyst wall.
2. Ultrasound and CT scan are Invaluable in localizing the cyst.
3. Serological tests depend on the sensitlzation of the patient to hydatid fluid, which
contains a specific antigen, leakage of which Induces the production of antiorgans. Among the
various test now available, hydatid immuno-electro-phoresis is the one of choice. This depends
on the formation of a specific arc of precipitation produced by the interaction of the serum
from the hydatid patient with the antigen as compared to a control.
4. There may be eoslnophilia, which is not specific but should at least arouse clinical
suspicion.
Treatment
A calcified cyst should be left alone. Other cysts should be treated to prevent complications.
Treatment with albendazole may result in shrinkage or even disappearance of the cysts. Failure to
respond or the presence of complications are indications for surgery. The cyst is exposed and aspirated. It is then possible to excise the cyst, working in the plane between the fibrous adventitia and
the laminated membrane, taking care not to liberate daughter cysts.
Ascariasis
18
Ascariasis it is widely distributed on all globe, except for the countries located in a circle of a polar belt. It is connected by that severe conditions of the north are adverse for development of the parasite. Disease was known to doctors and biologists of an extreme antiquity,
its activator is the intestinal parasite - Ascaris lumbricoides.
Crawling of round worms in intrahepatic bile ducts is observed at massive invasion of
ascarides of hepatocholedoch. The parasites who have got in hepatic bile ducts, the drilling
movements result to rough patomorphologic changes in gentle parenchima of organ, and a
plenty of tractogenic microflora on skin-muscular sheath of a worm promotes formation of set
abscess-forming cavities in a liver. Thus, most severe and dangerous complication of intestinal
ascariasis is mass helminthic invasion a liver. Ascariasis invasion intrahepatic ducts results to
cholangioectasia, cholangitis, pericholangitis abscesses, it is frequent completely incapsulated
and losing communication with bile ducts.
Ascariasis of liver in some countries meets enough frequently and after amebiasis the
second place on frequency genesis of hepatic abscesses, and in Vietnam even the first takes. At
the same time, Ascariasis of a liver not always results in formation of abscesses.
Recognition of ascariasis bilious ways and liver represents significant difficulties as
this disease is characterized by the attributes similar to other tractological conditions. In diagnostics ascariasis of bilious ways and liver the big attention should be given anamnestic data,
namely revealing of round worms in emetic or faecal weights which specify on helminthic
genesis and migration of intestinal parasites in organs of abdominal cavity. Characteristic clinical attributes to which concern first of all original strong, drilling, colic pains reaching significant intensity come to light. Pains are located in epigastral areas and the right hypochondrium.
Probably, that painful reaction is caused by passage of worms through major duodenal papilla,
and further pains arise in connection with infringement normal passage of bile. It is possible,
that intensity of painful reaction at this suffering depends on active behaviour of ascarides in
bilious ways.
The jaundice is observed at obstruction of distal part of choledoch by helminthic nodes.
However the jaundice is not a characteristic attribute of helminthic invasion hepatocholedoch
as ascarides with the mobility operate as a drainage, accelerating passage of bile in duodenum.
At a narrow end part of choledoch even one ascaride may result in its blockade of distal department. Subicteriosity and icteriosity of scleres and skin are observed at massive helminthic
invasion of outside and intrahepatic bile ducts, as result of development of parasitic cholangitis
and infringements of functional ability of a liver. Thus are frequent temperature reaction and
tremendous chills.
In some supervision ascariasis of liver it is accompanied by increase of the sizes of a
liver that is connected to a complex patomorphologic changes, namely stagnation of bile and a
progressing of infection.
In diagnostics of helminthic invasion of liver and bilious ways changed peripheral
blood. At this tractology are frequent eosinophilia (13-15 %), and at presence of inflammatory
process in parenchima of liver which is accompanied by purulent cholangitis or abscessing, are
marked by high leucocytosis with shift to the left, and also accelerated ESR.
Important value in diagnostics of ascariasis of a liver has definition in faeces eggs of
19
this parasite. For their revealing research is necessary to carry out repeatedly. However the importance of this test grows at the account of clinical attributes of abdominal ascariasis.
The valuable diagnostic method in recognition ascariasis of liver and bilious ways is
carefully carried out duodenal intubation. At this research in portions B and C a plenty of leukocytes and eggs ascarides is defined, that renders the big service to the clinical physician at
definition of character of tractological process in a liver and bilious ways. Ascariasis of liver
which quite often is complicated plural abscessing, may result to embolism of hearts, pulmonary arteries and its branchings. In these sheaths embol is ascaride, carried away a current of
blood from destroyed purulently-necrotic process of venous barriers of a liver in inferior cava
vein, then in the right auricle, ventricle of hearts, pulmonary artery and further in its branchings. This rare and heavy complication always comes to death.
Treatment always begins with a medicamentous course of antihelmintisation (levamisol, mebendasol, vermox). At absence of effect it is unique correct and saving action duly operative treatment is. The basic condition at operation concerning ascariasis a liver is careful
audit of bilious ways and a liver, especially left lobe as in it parasitic nestes are quite often
formed.
At presence ascarides in hepatocholedoch carry out supraduodenal choledochotomy with the
subsequent removal of parasites and obligatory drayning of hepatocholedoch. Simultaneously make
cholecystectomy. The drainage of bile ducts promotes outcrawling of parasites (if they were not
removed) and is effective means in struggle with cholangitis; besides on it is possible to enter directly into intestines antihelmints means. Cholecystectomy at ascariasisе of liver and bilious ways
carry out and at absence of macroscopical changes on the part of a gallbladder with a view of preventive maintenance of cholelithiasis for at parasitic defeat in a bubble quite often appear eggs ascarides which are the nucleus for formated of stones contain.
Duly operation concerning ascariasis of bilious ways and a liver is preventive maintenance parasitic abscessing of liver. Ascariasis abscesses of a liver settle down on a surface of a
liver more often, sheaths of break thinning walls of an abscess in a free abdominal cavity with
the subsequent therefore are frequent development of a peritonitis.
The best preventive maintenance of relapse ascariasis outside of and intrahepatic bile
ducts after removal from them intestinal parasites is well carried out repeated dehelmintisation
at repeating control of excrements on eggs of worms.
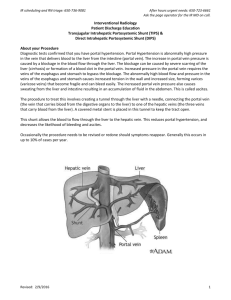
Portal Vein
Portal vein is formed by the union of splenic vein & superior mesenteric vein behind the neck
of pancreas. It is 8 cms long. It is a system of veins which starts in the cappilaries & ends in
cappilaries. Portal vein collects blood from a ) abdominal part of alimentary tract b) pancreas
c) gall bladder
d) spleen & conveys the blood to the liver.
Tributaries of Portal vein :
1. Splenic vein 2. Superior mesenteric vein 3.left gastric vein 4. Right gastric vein 5. Superior
pancreatoduodenal vein 6. Cystic vein 7. Para-umbillical vein.
Branches of Portal vein :
1. Right branch is shorter & narrower. It enters the right lobe of liver.
20
2.
1.
2.
3.
4.
5.
6.
Left branch is longer & getting the blood from para-umbillical vein ,itentrs the left lobe of liver
through porta hepatis.
Porta-Caval Anastomosis: These are collateral blood circulation path which start working
during portal vein obstruction.
Umbilicus : portal vein anastomosis with veins of anterior abdominal wall ( Systemic ) through
para-umbillical veins.
Anal canal : superior rectal vein (PV ) anastomosis with middle & inferior rectal vein (Systemic ).
Bare area of liver : hepatic venules (PV ) anastomosis with Intercostal veins & phrenic veins
(Systemic ).
Posterior abdominal wall : splenic vein ( PV ) anastomosis with renal vein & azygous vein
(Systemic ).
Liver : Left branches of portal vein (PV ) anastomosis with inferior vena cava ( Systemic ).
Lower oesophageous :through oesophageal tributaries of left gastric vein (PV ) with accessory
hemiazygous vein ( Systemic ).
PORTAL HYPERTENSION
Various diseases of a liver, a number of extrahepatic processes, and also direct pathological changes in portal vein result in significant infringements of a portal blood flow. These
diseases create obstacles to a blood flow of on separate sites of system portal veins and result
to symptom-complex of portal hypertension.
Portal hypertension (PH) is a syndrome of the various pathological processes developing owing to infringements of outflow of blood from system of portal vein. Sharp increase of
pressure in a combination to delay of a blood flow in system portal drives veins to varicose expansion of veins of a esophagus and cardia with frequent bleedings from them, and also to expansion of veins of anterior abdominal wall, splenomegaly, ascites and a number of other
changes of an organism.
In spite of the fact that this disease in the certain degree it was allocated as independent
discipline, it lies on a joint of many specialities: hepatology, gastroenterology, phlebology, infectious and surgical diseases, hematology, etc. Achievements of these sciences and occurrence of qualitatively new equipment have allowed improving diagnostics considerably various forms of PH. However treatment of PH till now remains insufficiently solved problem.
First of all complexity and diversity of a problem speaks that is more often PH is caused by a
cirrhosis of a liver. The term "a portal hypertension" for the first time in medical practice was
entered by the French researchers A.Zhilber and M.Villare in 1901. They have registered the
increased pressure in portal vein at the patients suffering by ascites.
Depending on localization of the pathological process caused infringement of portal
blood circulation, distinguish suprahepatic, intrahepatic, extrahepatic and mixed forms of PH.
Some authors, instead of the term "extrahepatic", use the term "subhepatic" PH. Most frequently meets intrahepatic PH. Basically it is caused by the cirrhosis of a liver developing as a result
of infectious processes (Botkin's disease) or toxic defeats of a liver (alcoholism, etc.). Less often its reason there are tumours of a liver, a chronic hepatites, a fatty dystrophy of a liver, sarcoidosis, malaria. In the special literature there are messages on cases intrahepatic PH which
develops owing to an obliteration of intrahepatic branchings of portal system connected to reception of massive dozes of cytostatics. Extrahepatic (subhepatic) PH is consequence of independent pathologic processes of the main vessels of portal system. The origin of this form PH
is caused by anomalies of development portal veins or its main inflows. In other cases extrahepatic PH is caused by a thrombosis portal veins (pylephlebitis) or its main inflows. Pylephlebitis develops owing to complications of purulent diseases of organs of abdominal cavity (appendicitis, cholecystitis, etc.). This form PH can be caused in newborns a thrombosis of an
21
umbilical vein with distribution of process on portal vein. Extrahepatic PH arises also at various diseases when vessels of portal system are exposed extravasal compression (compression
from the outside). It can be a tumour or cyst, starting with the adjacent organs (a stomach, a
pancreas, etc.). When the reason of extrahepatic PH there are independent diseases of vessels
of portal system (atresia portal veins or it cavernous transformation, etc.), that it allocate in the
separate form and name primary extrahepatic PH. Thus primacy of a pathology portal veins in
occurrence PH is emphasized. At the same time extrahepatic PH, arising owing to a compression portal veins at various somatic diseases, has received the name secondary extrahepatic
PH. This division primary extrahepatic PH as diseases of portal veins, and secondary - as syndrome, conveniently for practical purposes. The diagnosis of extrahepatic primary PH dictates
necessity of a choice of rational surgical tactics as imposing vascular porto-caval shunt. At
secondary extrahepatic PH it is necessary to diagnose disease which causes development of
this syndrome. Depending on a site of the block in the main inflows portal veins primary and
secondary extrahepatic PH it is supplemented with terms "total" and "segmentary". So, for example, at pancreonecrosis when occurs compression and thrombosis of splenic veins, developing further PH refers to secondary segmentary extrahepatic PH.
By principal causes of suprahepatic forms PH happen disease of Chiari, and also BuddChiari syndrome. At Chiari disease it is marked obliterating endophlebitis or thrombosis of hepatic veins. At Budd-Chiari syndrome there is a thrombosis of hepatic veins with distribution
on vena cava inferior or there is a stenosis vena cava inferior at a level of a confluence of hepatic veins. The stenosis vena cava inferior can be caused by primary vascular tumours (leiomyoma, leiomyosarcoma) or neoplasms of the various organs squeezing vena cava inferior or
hepatic veins (hypernephroid cancer, hepatoma, etc.). Substantial increase of pressure in vena
cava inferior is possible at the expressed cordial insufficiency and constrictive pericarditis.
Thus, irrespective of the reasons creating the block in various departments of system of
portal vein, all of them result to uniform symptom-complex a portal hypertension.
There are some variants of formation portal veins. The portal vein more often is formed
by merge of splenic and upper mesentery veins. At a confluence of a liver it forms portal sine
from which the right and left branches originate, and also cross-section branch for caudate lobe
of a liver. Occurs about five-seven branchings portal veins before the most thin interlobular
veins will turn in paralobular (septal) veins, which refer to as terminal capillaries. The last pass
in sinusoid capillaries (sinusoids) which are the common for arterial and venous blood. Sinusoid capillaries open in the central vein. From the central veins located in the center of lobules,
begins the drainage of system of hepatic veins. From them depart inserted and sublobulars collective veins and finally three main hepatic veins are formed: right, average and left. In the
field of posterior diaphragmatic surfaces of a liver all three hepatic veins run in vena cava inferior. On a place of their confluence are available sphincters. Thus, in sinusoid capillaries wide
communication between branches of portal veins and a hepatic artery is carried out. Thus, in
hepatocytes mixed blood. Neurohumoral and hemodynamic regulation of portal blood circulation is carried out through a network of sphincters, located on a course of a portal channel and
regulating inflow and outflow of blood. The difference of pressure in portal system is one of
the most important conditions of portal blood circulation. In portal vein pressure in norm
makes 5-10 mm Hg. An item, and in hepatic veins - 0-5 mm of a Hg.
Many questions of pathogeny PH at cirrhosis of a liver remain unexplored and disputable. At the same time PH the basic is or, at least, the important reason of some secondary functional frustration of a liver at a cirrhosis. Therefore pathogenetic factors PH are complex,
many-sided and to explain them only blockade of system of portal veins is impossible. Cirrhoses of a liver are characterized superfluous proliferation of connective tissue elements on
periphery and in the center of hepatic cells. As a result of growth of a connecting tissue comes
compression of portal venules, sinusoides or hepatic (central) venules, and sometimes both
those, and others. It conducts to essential increase of resistance to a blood flow in venous vessels of a liver and to difficulty of outflow of blood from portal veins. At the expressed cirrhosis
22
of a liver only 15% of blood of portal system reach sinusoides. Intrahepatic blood circulation
with development of arterio-venous fistulas is completely reconstructed. Some researchers
consider, that PH is caused by infringements of outflow of blood through hepatic (central)
veins. Thus most the great value is given to the postsine mechanism of blocking of a blood
flow. It is shown, that compression an intrahepatic venous blood flow is caused also by units
of regenerating hepatocytes. It matters perisinuidal fibrosis and arterio-venous anastomoses in
intralobular connective tissue septs, and also portal infitration. Some authors consider, that
acute increase of intrasinusoidal pressure is the reason of hepatic insufficiency and ascites.
Thus, intrahepatic blockade conducts to increase of pressure in system portal veins. In
norm pressure in portal vein makes from 50 up to 115 mm of waters. At PH pressure can rise
up to 600 mm of waters. It results to expansion of portocaval anastomoses and activization of
collateral blood circulations. Especially a lot of blood flows on portocaval anastomoses
through veins of cardial parts of a stomach and a esophagus, is less - on veins of anterior abdominal wall, hepatoduodenal ligature (vein of Sappey), rectum, pararenal and retroperitoneal
cellular, diaphragms, etc. It is necessary to note, that varicose veins of an esophagus and cardia, an abdominal wall arises only at PH. Thus the most vulnerable is esofagocardial zone
which is a acidce of fatal bleedings. Veins of an esophagus are influenced with two factors:
high portal pressure and an inconsistency of anastomoses veins of an esophagus with veins of
upper полой veins. Veins of esophagus, having the main type of a structure and weak friable
submucouse layer, extend easily, extended, becoming twisting and knotty. Veins bulged in a
gleam of a esophagus as 3-4 trunks, incorporating among themselves fine venous textures. Basically they are on a site in the extent about 4 sm in distal part of an esophagus and 3-5 sm in
cardial part of stomach. The expanded veins with atrophied elastic skeleton cannot resist high
and frequently varying intravascular pressure and even more extend. Esophagus mucous in this
parts gets blue-crimson color for the account bulging veins. On mucous of esophagus quite often there are erosion which frequently bleed.
In pathogenesis of bleedings from varicose veins a number of factors from which as
leaders are considered, a portal crisis (a hypertonic crisis in system portal veins), peptic factor
and infringements in coagulating system of blood matters. Portal pressure raises at a deep
breath, cough, defecation, physical tension, movements of a diaphragm, during dream, after
plentiful reception of food, etc. At PH the size of pressure depends on a degree of blockade of
system portal veins. Sharp fluctuations and high portal pressure can result in break decompensated varicose veins. Not casually bleedings develop after plentiful reception of food or during
dream when inflow of blood to organs of digestion considerably increases. Therefore many researchers consider, what exactly the hypertonic crisis is the starting mechanism of occurrence
of a bleeding from veins which walls pathologically are changed, and a mucous membrane of
an esophagus above them is sharp thinning. As we stated above, is frequent acidces of bleedings at PH erosion and ulcerations of mucous membrane of an esophagus are. A reflux in an
esophagus of acid gastric contents counts the reason of development erosive esophagitis. It is
marked, that varicose veins can be damaged by firm food. From this corresponding recommendations for hygiene of a feed follow at PH. It is necessary to take into account a role of
gross infringements in coagulating to system of the blood, being one of the reasons of heavy
bleedings at PH. It is necessary to note, that each subsequent bleeding aggravates hypoxia of
liver and worsens its functional condition.
Ascites, developing at intrahepatic forms PH, depend on the deep exchange infringements connected to diseases of a liver. They are caused by infringements of an albuminous and
water-salt exchange, reduction of the albumin contents, delay of allocation of sodium and
changes of flow of lympha in a liver. Ascites is characteristic for intrahepatic PH, and also for
syndrome Budd-Chiari at which it develops very quickly. At the same time ascites is very seldom marked at patients with extrahepatic PH and is especial at persons with primary extrahepatic PH. It speaks that function of a liver at them is not broken almost.
23
In reply to the block in portal system there is a stagnation in a spleen and splenomegaly
develops. The increase in inflow and reduction of outflow of blood from a spleen conducts to
amplification of its function and hyperplasia. Thus the spleen can contain up to 500 ml of
blood. Sometimes it becomes huge, as aneurysm, occupying thus half of abdomen. Than closer
to a spleen the block of a portal blood flow is located, especially expressed splenomegaly. At
extrahepatic PH splenomegaly long time can be unique clinical sign. Amplification of function
of a spleen can result in an anemia, лейкопении and a thrombocytopenia (hypersplenism). The
fact of that after bleedings a spleen is sharply reduced, testifies that stagnation in it is the leading mechanism of occurrence splenomegaly at PH.
Blood at PH, passing a liver, through porto-caval anastomoses enters in the big circle
of blood circulation. At a terminal stage of cirrhosis from portal blood circulation are switched
off from 60 up to 80% of branchings portal veins. This blood contains harmful nitrogenous
products which cause brain intoxication. At cirrhoses of a liver and without that there are sharp
infringements desintoxication functions of a liver. The massive ammoniac intoxication conducts to development of an encephalopathy. These infringements of metabolisms I.P.Pavlov
named "meat intoxication".
At intrahepatic PH all organs and systems suffer. As a result of stagnation and high capillary pressure there is a hypostasis of a mucous membrane of small bowels. Therefore in it
process absorbing is broken. Amplified allocation rich fiber of a liquid through an intestinal
wall that carries the name exudation enteropatia begins. Also the cardiovascular system also
suffers. Than the changes in a liver are deeper, is heavier defeat of a myocardium.
Clinical picture. At expressed PH its various forms, basically have similar clinical semiology. Basic symptoms PH are: expansion of veins of a esophagus and a stomach, and also
veins on anterior abdominal wall and hemorrhoidal veins, splenomegaly and signs of hypersplenism, hemorrhagic signs (bleedings from gastroesophageal veins, a mucous membrane of a
nose, gums, and also hemorrhoidal and uterine bleedings), ascites. Clinical distinctions between forms PH are shown in terms of their occurrence and a degree of expressiveness of separate attributes. Features of clinic can be caused also by weight of pathological process in a
liver and the hepatic insufficiency connected to it. So, at patients with extrahepatic PH ascites,
as a rule, it does not happen, and if it arises, in late stages. Quite often started diseases at them
is connected to casual detection of the increased spleen. At the same time at diseases Chiari
and Budd-Chiari the initial stage can be shown by sudden occurrence ascites and sharply increased, painful liver. The increase of spleen at them is marked later. It is necessary to emphasize once again, that varicose veins, is especial in cardioesophageal areas are characteristic only for PH and meet at all its forms. And, repeating, we shall notice, that bleedings from these
veins are one of the main reasons of death at PH.
Most frequently there is intrahepatic form PH. As it was mentioned, the main reason of
it is the cirrhosis of a liver. Except appropriate for PH attributes, it can be marked and other
semiology carrying the common character. At diffuse defeats of a liver the clinical signs connected to hepatic insufficiency are marked. Allocate dispeptic and astenovegetative syndromes. For the first are characteristic bad appetite, feeling of dryness and bitterness in a
mouth, thirst, a distortion of taste, intolerance of fat food and alcohol, etc. There can be disgust
for smoking. Attributes of the astenovegetative syndrome there is a weakness, decrease in
work capacity, a sleeplessness, the suppressed mood, irritability, etc.
At women may be infringement of the menstrual cycle, and at men - an impotence.
There are nasal bleedings and increased gingival hemorrhage. Bad sight in darkness is quite often marked. The nausea, weight in epigastrium, an eructation and constipation frequently disturb. Typically persistent abdominal distension (meteorism) which is frequent precedes occurrence of ascites. Frequently patients complain of feeling of weight, pressure and pains in the
right under the ribs. But these pains not intensive, whining character. They are caused by a
stretching of glisson capsules. Pains can amplify at inclinations forward and sharp movements.
24
The jaundice or icteric discolouration of the scleras is possible. At times patients are
disturbed with an itch, is especial in interfinger plications, axillary areas, shins or forearms.
The itch amplifies in warm or at night. The skin can have an earty colour. On the face, neck
and hands (zone "decollete") there can be vascular "asterisks". As a rule, it is the soft formation slightly raised above a surface of skin and quite often pulsing arteriola, with radial capillaries departing from it or circular zones of skin hyperemia. It is possible hyperemia tips of
fingers and palms that carries the name "palmar erythema". Bright red painting of lips and
tongue ("cardinal`s tongue") is sometimes observed. Fingers can be as drum-type sticks, and
nails - in the form of watch-glasses. Quite often arises Dupuytren`s contraction. It is marked
poor pilosis on pubis, axillary cavity. Also take place an atrophy testicles and gynecomastia.
Frequently increase parotides. At the most part of patients the cirrhosis of a liver marks loss of
weight. The clinic of cerebral insufficiency can be moderate. At times it is brightly expressed
as sharp excitation, delirium or depression, drowsiness and down to coma.
Ascites is a characteristic attribute of intrahepatic form PH and Chiari diseases. It can
sometimes be undistinguished and easily gives in to conservative therapy. Quite often, especially at decompensated cirrhoses, ascites becomes resistant and results in an exhaustion of patients, and also increase hepatic, renal and cardiovascular insufficiency. At survey the sharp
increase of abdomen with tense, thinning, a smooth skin of anterior abdominal wall and bulging of umbilicus is observed. On the abdominal wall there are expanded hypodermic veins
(symptom Cruvelier-Baumgarten). They can remind a kind "heads of medusae" around umbilicus, or be distributed in the direction of thorax or superpubic areas. At times above them
"noise of humming-top" is listened specific. Expansion of veins of an abdominal wall is caused
by development of portocaval anastomoses, as a rule, as a result of functioning umbilical vein.
It is necessary to note, that at Chiari disease the expanded veins are located not on anterior abdominal wall, and on lateral walls of abdomen, and also on a back and the bottom extremities
is more often.
The most dangerous and heavy complication is bleedings from veins of the cardioesophageal zones. These bleedings frequently recur and quite often come to death of the patient.
Especially high remains lethality from bleedings at intrahepatic form PH. This is promoted also by the progressing hepatic insufficiency developing in result of blood loss.
It is necessary to note, that already from the first bleeding expired about 20% of patients. Lethality at relapsing bleedings makes 45-60%. Quite often after massive bleeding at
patients with a cirrhosis of a liver for the first time arises ascites and process in a liver becomes
more active. Lethality from bleedings at extrahepatic PH is much lower.
The clinic of a bleeding is shown first of all by bloody vomitting (hematemesis). Thus
bloody vomitting is more often plentiful, and together with emetic weights of color of "a coffee grounds" scarlet blood that testifies about heavy blood loss is allocated. The black chair
(melena) and the general attributes of acute blood loss is marked also: weakness, dizziness,
falling of arterial pressure, a tachycardia, pallor of integuments.
At all forms PH there is an increase in a spleen. However the sizes of this increase are
various. Especially typically expressed increase in a spleen at extrahepatic PH. Quite often patients mark feeling of weight and a pain in left under the ribs, that is caused adhesions spleens
with surrounding organs and tissues, and sometimes - heart attacks of a spleen. As a rule, at
bleedings the spleen is reduced. Further it again increases till the former sizes. Splenomegaly
is accompanied by hypersplenism, that is shown by reduction of thrombocytes up to 8000030000, and leukocytes up to 3000-1500. The constant moderate anemia which even outside of
a bleeding becomes significant is marked and hardly gives in to treatment.
Diagnostics PH in typical cases is not difficult, however variability and atypical currents of separate forms demand application of special additional methods of research. Nevertheless, careful studying the anamnesis of disease first of all is necessary. The infectious hepatites transferred in the past and the subsequent development of cirrhosis of a liver is typical of
intrahepatic form PH. Thus the men quite often suffering alcoholism are ill more often. Prima-
25
ry extrahepatic forms PH, as a rule, develop at children's age. Indications on the umbilical sepsis transferred in the childhood are possible. Chiari disease concerns to rare diseases. In 20%
of cases it proceeds as the acute form. Suddenly arise abdominal pains accompanying with fast
increase of a liver and rough increase ascites which badly give in therapies. At the chronic
form of Chiari disease the gradual increase in the sizes of a liver, various intensity of a pain in
abdomen and resistant ascites are observed. The forecast at disease Chiari happens adverse is
more often.
Diagnostics of various forms PH consists first of all in diagnostics of a cirrhosis of a
liver. Thus function of a liver with the help of laboratory, isotope, ultrasonic and other methods of research is studied. In diagnostics of structural changes of a liver ultrasonic, a computer
tomography, a nuclear magnetic resonance are widely applied. Are applied laparoscopic researches with biopsy a liver. Now it is widely used transdermal biopsy a liver under the control
of an ultrasonic beam with convex gauge. The spectrum of the laboratory researches describing function of a liver, is extremely wide - from definition of protein and its fractions, and also
transaminase up to the most complex immunologic researches.
In a wide network of medical institutions the ultrasonic equipment enables to orient
precisely in a pathology of a liver. X-ray research of a esophagus and a stomach allows to diagnose varicose veins of cardioesophageal zones and to plan of the further inspection. In diagnostics of varicose veins fibroesophagogastroscopy (FEGDS) has crucial importance. Task of
FEGDS includes definition of localization and type of varicose veins: trunk or network. Also is
solved the problem on a degree dilatation of an esophagus, a functional condition cardia and
expressivenesses of the reflux-esophagitis. The stomach and duodenum are investigated for revealing of possible accompanying diseases (a stomach ulcer, a cancer, erosion, etc.). Endoscopically the probability of development of a bleeding from varicose veins is predicted, tactics of treatment is planned. Thus allocate 3 degrees varicose veins: I degree - 2-3 mm, II - 3-4
mm and III – 5 mm and more. Results of researches have shown, that at I degrees probability
of occurrence of a bleeding minimal, at II - the probability of a bleeding within one year makes
about 40%, and at III-93,2%. Proceeding from this, indications to operative intervention are established. Now more and more a wide circulation has received endoscopic sclerotherapy of
varicose veins.
Earlier it was widely applied splenoportography and splenomanometry. For the first
time splenoportography is executed S.Abeatichi and L.Kampi in 1951. For carrying out of this
research in the ninth intercostal space at the left on a back axillary line punctured a spleen.
Then portal pressure is measured and entered water-soluble X-ray contrast substance which
acts in portal vein and its intrahepatic branchings. It is applied coeliacography with selective
hepatic arteriography. Narrowing of hepatic artery is typical for liver cirrhoses with pauperization of intrahepatic vascular figure. Also it is carried out selective contrasting of the upper
mesentery arteries. Arteriomesentericography enables diagnostics extrahepatic forms PH. Thus
in a venous phase contrasting expansion upper mesentery veins and pathological changes (a
stenosis, amputation, etc.) is defined splenic or portal veins. For diagnostics of Budd-Chiari
syndrome is carried out cavagraphy. Punctured the femoral vein on Seldinger and through it
catheter is carried out in vena cava inferior, and then entered X-ray contrasting preparation. It
is sometimes carried out portohepatography through a umbilical vein. For this purpose by a
small section above umbilicus on a white line is dissected aponeurosis. Then the umbilical vein
through which the system portal veins is contrasted is allocated and dilate with a bougie.
Concluding section of diagnostics, we mark, that hospital network is equipped enough
endoscopic and ultrasonic equipment. On the basis of clinic and results of these inspections diagnostics of syndrome PH is possible. Carrying out complex, including intravasal researches,
with the purpose of diagnostics of various forms PH, it is carried out in large, and also the specialized clinical establishments.
Surgical treatment. First of all it is necessary to emphasize, that a basis of all operations
at intrahepatic form PH (except for transplantation of a liver) preventive maintenance or a stop
26
of a bleeding from varicose veins of cardioesophageal zones. Only at primary extrahepatic PH
when the structure and function of a liver are kept, after imposing vascular porto-caval anastomosis it is possible to expect for recovery.
In 1877 the Russian surgeon and physiologist N.V.Ekk has developed in experiment
operation vascular porto-caval anastomosis. He cut distal part of portal veins and connected it
with upper cava vein the end to side. He has proved, that switching-off of a liver from portal
blood circulation does not conduct to it necrosis, but there come heavy general infringements
of metabolism character. I.P.Pavlov in 1892 has altered a technique of operation of N.V.Ekk
and imposed this anastomosis side-to-side without crossing of portal veins. Researches have
shown, that at experimental animals after this operation also there come infringements of a metabolism with frustration of function of the central nervous system. It has been connected to an
intoxication nitrogenous slags. For the first time in clinical practice in 1903 M.Vidal has executed porto-caval anastomosis to the patient with a cirrhosis of a liver with ascites. The patient
was died from hepatic insufficiency. In connection with high lethality and complexity of performance portocaval anastomoses operations counting upon formation of collateral between
systems of portal and cava veins began to be applied. With this purpose filed an omentum to
anterior surface parietal mesentery (D.Drummond, R.Morison, 1896; S.Talma, 1898).
G.Schiassi (1901) carried out an omentum in retroperitoneal cellular, W.Мауо (1924) - in a
vagina of a direct muscle of abdomen, and A.Narath (1905) - in hypodermic fat. Also used an
omentum for creation of adhesions with the organs having outflow in system of cava vein. For
this purpose moved testicle to a abdominal cavity and shrouded in its omentum. Carried out
decapsulating of kidneys and closed its omentum. It was used omentohepatopexia and a number of other similar operations. However effect of them was unstable and by present time as
independent operations at PH they are not used. A.Whipple, A.Blakemore, I.Lord began to apply operation splenorenal anastomosis. Thus the spleen and the left kidney left, and their vessels incorporated the end in the end. R.Linton, A.Blalock (1947) at performance splenorenal
anastomosis a kidney did not delete, and the end splenic arteries sewed to side of the left renal
arteries. V.Satinsky (1948) for imposing splenorenal anastomosis began to use thoracoadominal access. The first successful operation of imposing direct porto-caval anastomosis in
Russia belongs to F.G.Uglov (1952).
As it was mentioned above, main principle of all operations at intrahepatic and mixed
forms PH is preventive maintenance or a stop of a bleeding from varicose veins. With this purpose it was applied about 200 various operative interventions only on gastroesophageal zone
(gastrectomy, esofagocardial resection, Taner operation, etc.). Basically all these operations by
present time are left. In emergency situations probe-obturator of Blakemore is widely applied
to stop of a bleeding from varicose veins. This probe has two pneumatic cylinders and three
gleams. Through one gleam aspirated gastric contents, and through others two - are inflated
gastric and esophageal cylinders. Inflated by air, both cylinders squeeze varicose veins and
carry out a mechanical stop of a bleeding. In this condition the probe - obturator is left at 48-72
o'clock. Periodically cuff is dismissed and checked reliability of a hemostasis. Also intensive
conservative hemostatic therapy is carried out. If with the help of these actions it is not possible to stop a bleeding operative intervention is shown. Basically it is applied gastrotomy and
suturing of bleeding varicose veins. Tanner operation consists that the stomach is cut from a
esophagus is sometimes used, spill varicose veins, and then the stomach again is sewed with a
esophagus. Now all these operations at height of a bleeding are practically left, for lethality at
them remains to the highest. So, at decompensated cirrhosis of a liver at height of a bleeding
any operative intervention including suturing varicose veins, it is accompanied lethality up to
90% and is higher. Therefore use of a probe-obturator and carrying out of intensive conservative therapy serves in such situations as a method of a choice. Except for infusion and transfusion therapy directed on a stop of a bleeding and compensation of blood loss, the preparations
reducing inflow of blood in portal system are entered. To these preparations concern pituitrin,
27
oxytocin, sandostatin, octreotid, remestip, etc. At FEGDS the various manipulations directed
on realization of a hemostasis are carried out (ligation or sclerotherapy of the veins).
In the scheduled order basically four kinds of operations are applied: direct interventions on veins of esophagus and stomach, vascular porto-caval anastomoses, эндоскопическое
sclerosing of veins and transplantation of a liver. Indications to portocaval anastomoses at intrahepatic PH now are limited. At primary extrahepatic PH duly performance porto-caval anastomosis is operation of a choice as in essence results in recovery of patients. In our country in
these situations the preference is given mesentericocaval anastomosis. The new problem is
TIPS - transdermal interhepatic system shunt.
Serious problem there is a treatment of proof ascites. The basic surgical methods of
treatment proof ascites are: adominal paracentesis, peritoneo-venous shunting, transjugular intrahepatic portosystem shunt and transplantation of a liver. The combination concerns to a new
method of treatment ascites by paracentesis with intravenous introduction of ascites liquids
and parallel application of diuretics. Introduction of ascites liquid with the help of hemialisator
allows to avoid possible complications. The essence of operation of imposing peritoneojugular shunt will be, that in a abdominal cavity is established conduit with valve Le Veen
from which departs catheter. Last is carried out hypodermically and entered through jugular
vein in the right auricle. Thus unloading of abdominal cavity from a liquid and the further removing by its natural way is carried out. Apply operation of imposing lymphovenouse anastomosis between a thoracic lymphatic channel and jugular vein.
Duly diagnostics and the qualified help can improve results of treatment and considerably prolong a life of patients PH. The further finding-out of complex pathogenetic mechanisms, development of preventive actions, creation of new pharmacological means will give an
opportunity of better treatment PH. Wider introduction of transplantation of a liver will rescue
a life of many doomed patients.
Cirrhosis of the liver
It is a condition characterized by chronic hepatic cells damage, disruption of hepatic
architecture, regeneration and overgrowth of fibrous tissue, fibrosis and proliferation of remaining cells with the features of progressive hepatocellular failure&portal hypertension.
Classification of a cirrhosis of a liver
(the World association on studying a liver, Acapulco, 1974;
WHO - 1978)
1. On morphology.
1.1. Macronodular.
1.2. Micronodular.
1.3. Mixed macro - and micronodular (incomplete septal).
1.4. Primary biliary.
2. On etiology.
2.1. Virus (a virus of a hepatites B, C, D).
2.2. Alcoholic.
2.3. Toxic (medicines and chemical substances).
2.4. Connected to congenital infringements of a metabolism.
2.4.1. Galactozemia.
2.4.2. Diseases of accumulation of glicogen.
2.4.3. Thirozinozis.
2.4.4. Congenital intolerance of fructose.
28
2.4.5. Deficiency an alpha - 1 - antitripsinum.
2.4.6. Talassemia.
2.4.7. Hypermethioninemia.
2.4.8. Konovalov-Wilson's disease.
2.4.9. Overload iron (hemochromatosis).
Activity? Compensation? Russian scientists necessarily estimate these two parameters:
active, inactive, compensated, decompensated.
Clinical classification.
1. Portal
2. Biliary
3. Cardiac (in severe chronic congestive failure)
4. Haemochromatosis
5. Hepatolentlcular degeneration (Wllson-Konovalov's disease)
6. Schistosomiasis (Egyptian splenomegaly)
1. Portal
a) alcoholic
b) nutritional (deficient protein diet)
c) post-necrotic
d) idiopathic
The main difference from chronic hepatitis – development of portal hypertension.
Clinical features.
1. Hepatomegaly – is common but as the disease progresses, due to the destruction of
hepatocytes&proliferation processes, the liver reduces in the size, becomes painless, hard and
irregular.
2. Jaundice - is usually mild and is due to failure of transportation of bilirubin by the
hepatocytes.
Unconjugated bilirubin level is high because damaged hepatocytes can not conjugate it.
Conjugate bilirubin level is high as due to inflammation of hepatic cells and biliary canal, some part of bilirubin which is conjugated by the remaining hepatocytes,can not pass in to
the bile.
3. Ascites – is due to inadequate sodium and water balance and excretion. Since due to
hepatic failure in cirrhosis, synthesis of proteins is impaired resulting in hypoproteinaemia
which cause decrease in blood oncotic pressure. As a result of which fluid accumulates in the
extracellular space, resulting in ascites and oedema.
4. Circulatory changes: teleangioectasia, palmar erythema.
5. Endocrine changes: due to loss of detoxification of oestrogen in the liver: in males:
testicular atrophy, gynaecomastia, hair loss, impotence; in women: breast atrophy, irregular
menses, amenorrhoea.
6. Haemorrhagic tendency: easy bruising (hematomas) – bleeding from teeth gums due
to defect in coagulation system.
7. Portal hypertension: splenomegaly (difference from hypersplenism: low erytrocytes,
29
leucocytes, thrombocytes count), collateral blood circulation: bleeding varices (hematemesis &
melena), hemorrhoid.
8. Hepatic encephalopathy: due to hepatic damage and shunting of blood, undetoxified
blood reaches the brain (usually nitrogenous substances like ammonia). I.P.Pavlov writes this
syndrome after portocaval anastomosis.
9. Asteno- vegetative syndrome: nausea, vomiting,anorexia.
INVESTIGATIONS
1.
Blood test:
a) bilirubin level is high (both unconjugated & conjugated bilirubin level is high);
b) high level of aminotransferase (ALT&ACT);
c) high level of alkaline phosphatase;
d) low level of serum proteins - since the synthesis is impaired;
e) albumin / globulin level is altered — as albumin synthesis is impaired;
f) prothrombin index is decreased – coagulation time is increased.
2. Ascite test:
a) transudative in character (protein level less than 2.5 gm per liter);
b) straw coloured.
3. Ultrasound – may reveal:
a) ascites;
b) increase in a liver and spleen
4. Ba-oesophagogram - reveals filling defects due to variceal formation.
5. Esophagoscopy (expansion of esophageal veins, esophagitis, sclerotherapy).
5. Splenoportography: expansion of veins of portal system, symptom of "the dried out
tree": there is a trunk, and leaves and fine branches have dried out.
6. Arteriography (embolization of splenic and gastric arterues); coeliacography with selective hepatic arteriography. Narrowing of hepatic artery is typical for cirrhoses of a liver with
pauperization of intrahepatic vascular figure. Also it is carried out selective contrasting of upper mesenteru arteries. Arteriomesentericography enables diagnostics of outhepatic forms of
portal hypertension.
7. Intracutaneous intrahepatic cholangiography - shows undilated bile ducts.
COMPLICATIONS
1. Portal hypertension: hematemesis and melena, variceal bleeding, splenomegaly.
2. Hepatic encephalopathy.
3. Hepatorenal failure.
4. Ascites.
5. Hepatic carcinoma (adenoma, the short anamnesis is characteristic.
6. Bacterial infection (tuberculosis)
7. Hypersplenism - low erytrocytes, leucocytes, thrombocytes count count.
TREATMENT
1.
Diet: nutritious with high carbohydrates and moderate protein level.
2.
Diuretics: Furosemide 20 mg with potassium solutions (KCL 1%-100,0) I.V.
3.
Treatment of anaemia (usually anaemia is posthemorrhagic, hypochromic), during
low Hb level - blood transfusion.
30
4.
Slow drainage of ascitic fluid.
5.
I.V - protein solutions like aminocrovin.
6.
Antibiotics.
7.
Preliminary possibilities bleeding from varices - I.V.- Sol. Vicasoli 1% - 4,0; Vasopressin – 20 units.
PORTAL HYPERTENSION
The normal portal pressure is between 80 and 150 mm of water. In portal hypertension
this pressure may be raised to 500 mm or more.
Aetiology. Portal hypertension results from an obstruction in the portal tree. The causes
are classified according to the site of the block.
1. Pre-hepatic obstruction of the portal venous inflow into the liver
a) congenital malformation of vessel
b) spreading portal vein thrombosis in the neo-natal period from an umbilical infection
c) occlusion by tumour or pancreatitis
2. Hepatic (obstruction of the portal flow within the liver): the cirrhoses.
3. Post-hepatic obstruction of the hepatic veins: Budd-Chiari syndrome
a) Idiopathic hepatic venous thrombosis in young adults of both sexes. A possible complication of oral contraceptives in women. In many cases there is an underlying haematological neoplasm for example, polycythemia or monoclonal gammaglobulinopathy.
b) congenital obliteration
c) blockage of hepatic vein by tumour invasion
The 2 important effects of portal hypertension are:
1 The development of a collateral portal-systemic circulation.
2 Splenomegaly.
In course of hepatic insufficiens: ascites, the manifestations of hepatic failure (in severe
cirrhosis).
Collateral channels
Portal obstruction results in the development of collateral channels between the portal
and systemic venous circulations. These are:
1. Between the left gastric vein and the oesophageal veins, forming oesophageal varices; the largest and clinically the most important connections.
2. Between the superior and inferior rectal veins with development of haemorrhoids,
which are true varices.
3. Along the obliterated umbilical vein to the superior and inferior epigastric veins (caput medusae).
4. Retroperitoneal and diaphragmatic anastomoses, which present technical hazards to
the surgeon at time of operation.
The management of haemorrhage from oesophageal varices.
The factors of the prognosis: augmentation of a liver and lien, ascites, icterus, system
of Child, Pugh.
This is particularly dangerous, especially in patients with liver damage. In these subjects the liver is further injured by the hypotension of blood loss, and portal-systemic encephalopathy may be precipitated due to the absorption of large amounts of nitrogenous breakdown
31
products from the 'meal of blood' within the Intestine. Prognosis is better in the small group of
patients with normal liver function and a prehepatic block.
An attempt must be made to confirm the diagnosis. The presence of established liver
disease, an enlarged spleen and proven varices does not necessarily mean that bleeding is from
the varices. Such patients are prone to bleed from gastric erosions and are commonly affected
by peptic ulceratlon. Fiberoptic endoscopy should always be performed in order to visualize
the bleeding point and to exclude non-variceal haemorrhage. Bleeding varices are injected directly with sclerosant solution. Active bleeding may, however, prevent a satisfactory view at
endoscopy.
The immediate treatment of haemorrhage is blood replacement by transfusion. Nitrogenous absorption from the bowel is reduced by emptying as much as possible of the blood
from the colon by means of an enema, giving neomycin by mouth to reduce bacterial decomposition of blood in the gut, withholding protein from the diet and maintaining nourishment by
means of glucose given by mouth or intravenously. If bleeding continues, more vigorous
methods may be required, but here careful decision must be taken; if the patient is in advanced
hepatic failure with jaundice, ascites, a low serum albumin. Impaired clotting, thrombocytopenia and precoma or coma, then it is wise practice to refrain from further treatment since the
prognosis Is hopeless and further procedures merely add to the discomfort of an already dying
patient.
In fitter subjects, the haemorrhage is stemmed either by:
1. Direct pressure on the varices using a Sengstaken tube which is introduced through
the mouth into the oesophagus and cardia, then distended, or
2. Intravenous pitressin (20 units by slow intravenous injection), remestipe, sandostatin, octreotide, which produces a marked fall in portal venous pressure and temporary
cessation of bleeding by mesenteric arteriolar constriction. Therapeutic doses cause intestinal
colic. The emergency surgical procedures are: probe of Blakemore-Sengstaken.
Blakemore-Sengstaken tube. Balloons in the oesophagus and in the cardia compress the
bleeding varices; the gastric tube can be used either for aspirating the stomach or for feeding
purposes.
1. Trans-thoracic ligation of the varices, which is effective for varices limited to the oesophagus.
2. Porta-caval anastomosis between the portal vein and the inferior vena cava, which
shunts the portal blood directly into the venous systemic circulation and thus lowers the portal,
pressure.
3. Injection of the varices via a long needle Introduced through an esophagoscope (polydocanol). This technique is analogous to the injection treatment of piles. This procedure can
stop bleeding with minimal trauma to the patient although there are the risks of perforation of
the oesophagus and repeated injections may produce ulceration or fibrosis. Control of the
bleeding allows the surgeon to assess the patient as a candidate for liver transplantation. Laparotomy should be avoided if possible if a subsequent transplant is planned, since the resulting
vascular adhesions will greatly add to the dangers of the transplant operation. If the patient is
not a candidate for a transplant, then definitive surgery to prevent further bleeding may be con-
32
templated. This may comprise.
4. Porta-azygos disconnection, in which the varices around the lower end of the oesophagus and the upper stomach are divided at the cardio-oesophageal junction using the circular stapling gun, in order to interrupt the communications between the two systems of veins
within the wall of the lower oesophagus.
5. If the portal vein itself is occluded by a thrombus or is congenitally abnormal, portacaval anastomosis is impossible. The portal system can be shunted to the systemic system by a
variety of techniques, spleno-renal anastomosis between the splenic vein (after splenectomy)
and the left renal vein is that most often performed.
The types of decompression shunt.
A. End to side porta-caval shunt, the most straightforward procedure.
B. Side to side porta-caval shunt, if the venous outflow of the liver is blocked and
blood is leaving the liver from the portal vein.
C. The end to side spleno-renal shunt with splenectomy.
D. The mesocaval H-shunt is indicated when a side to side shunt is impossible, for example, when the portal vein is blocked.
E. The distal spleno-renal Warren shunt is designed to reduce selectively the blood
pressure in the oesophageal varices, decompression occurs via the short gastric veins and
splenic vein into the renal vein.
6. TIPS – transdermal intrahepatic systemic shunt. Portal-systemic shunting may be
performed in the elective stage when there have been previous episodes of haemorrhage. Such
procedures again should only be carried out in patients with reasonable hepatic function. Jaundice, plasma albumin of less than 25 g/1 and poor general condition are contra-indications to
surgery.
Unfortunately, operative procedures in which an anastomosis is made between the portal
and systemic circulations are likely to precipitate portal-systemic encephalopathy and such patients
often have to be maintained indefinitely on a low protein diet. The further from a liver an anastomosis, the less often encephalopathy.
However, liver transplantation is now a preferable option except in cases of prehepatic
obstruction with good liver function.
Treatment of ascites
1. Paracentesis gives immediate relief if discomfort is intense, but it has the disadvantage that the patient loses protein.
2. Low sodium, high protein diet, Intravenous albumin.
3. Diuretics: chlorothiazide (with potassium supplement) and
4. Peritoneo-venous shunt (LeVeen or Denver): a silicone rubber catheter with a pressure-activated valve, which shunts ascitic fluid from the peritoneal cavity back into the venous
systems via the internal jugular vein.
5. Surgery: only occasionally indicated; a few patients may be fit enough for portacaval anastomosis which sometimes relieves ascites.
6. Angiography – embolisation of vein according intravessel pressure.
2. Biliary cirrhosis (primary biliary cirrhosis – PBC). Over 90% of patients are female 40 to
60 years of age. The most common symptom is pruritus, being present in over two thirds of the
33
patients. The typical pattern is an extremely high alkaline phosphatase with a disproportionately low, and often normal, bilirubin. There is often a striking elevation of the serum IgM. The
serum cholesterol level may be increased, and there may be other evidence of hyperlipidemia.
There is clearly some heterogeneity in antimitochondrial antibodies; nine types (designated anti-M1-M9). The main microscopic sign – lymphoid infiltrates around bile ducts. These patients
are often seen first by a dermatologist because of their intense pruritus; some 30% of them
have cutaneous xanthelasmas.
For patients with terminal stage PBC the problem is solved carrying out of transplantation of a liver. At earlier stages of disease the indication to transplantation of a liver can be a
painful, not stoped skin itch.
a) primary (Hanoi's cirrhosis)
b) secondary to prolonged biliary obstruction
c) an autoimmune disease with raised serum anti-mitochondrial antibodies: PRIMARY
SCLEROSING CHOLANGITIS – PSC. The typical patient with PSC is a man under 45 years
of age; the sexual predominance seen in PBC is not quite so striking, but some 60-70% of PSC
patients are male. The alkaline phosphatase is usually fourfold or greater increased, often with
a normal bilirubin level. Ulcerative colitis will be found in over 70% of patients with PSC; uncommonly the underlying inflammatory bowel disease will prove to be Crohn's disease. Ordinarily PSC appears in a patient with known ulcerative colitis; the ulcerative colitis often appears particularly quiescent in these patients. There is a combination to other diseases: thyroiditis, Sjogren syndrome, coeliacia, sarcoidosis, a chronic pancreatitis, rheumatoid arthritis, autoimmune hepatites, a system sclerosis and system red lupus. Cholangiogram, usually obtained
via RCPG, remains the gold standard for the diagnosis of PSC. When specimens of the large
bile ducts are available, multifocal areas of acute and chronic inflammation are present; there
is usually a striking lymphocytic predominance, and lymphoid aggregates are commonly
prominent.
To specific complications PSC concern bacterial cholangitis, strictures of bile ducts,
cholelithiasis and cholangiocarcinoma.
When are formed strictures, it is carried out endoscopic or transdermal ballon dilatation. At
unsuccess or impossibility endoscopic corrections carry out reconstructive operations on bilious ways. For treatment of patients with final stage ПСХ unique effective means of treatment
remains liver transplantation.
About other versions of a cirrhosis of a liver to you will tell on corresponding faculties.
It is.
3. Cardiac (in severe chronic congestive failure).
4. Haemochromatosis.
5. Hepatolentlcular degeneration (Wllson-Konovalov's disease).
6. Schistosomiasis (Egyptian splenomegaly).