PBS Paper-Final Version - Australian Medical Association
advertisement

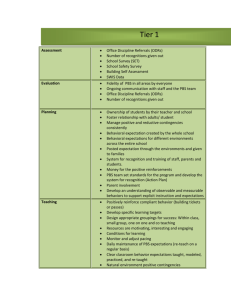
PBS DISCUSSION PAPER with AMA Federal Council Resolutions Prepared by: Dr Jennifer Thomson Acting Director, Health Services Mr Roger Kilham Consultant Economist Federal Secretariat Australian Medical Association 42 Macquarie Street BARTON ACT 2600 Tel: 02 6270 5400 Fax: 02 6270 5499 March 2002 AMA - PBS Discussion paper prepared by Jennifer Thomson & Roger Kilham Feb 2002 1 AMA - PHARMACEUTICAL BENEFITS SCHEME (PBS) DISCUSSION PAPER Introduction The Pharmaceutical Benefits Scheme (PBS) is an important plank of health care in Australia. It has been in existence for 50 years during which time it has evolved from a scheme for the provision of drugs for life threatening conditions to a scheme for the provision of timely, reliable and affordable access to necessary and cost effective medicines1. The scheme is now looming as a large target for the attention of central expenditure control Departments (Treasury and Finance) due to both its size and the rate of growth of spending. The PBS cost $1 billion in 1987 and reached $4 billion in 2000/01.2 The trend rate of growth of spending under the PBS has been of the order of 10 to 11% per annum (nominal), which equates to about 6 to 7% in real per capita terms. However, in the year 2000-01, spending grew by about 19%, significantly boosted above the trend rate by Ministerial decisions to list two new drugs (Celebrex for arthritis, Zyban for anti-smoking). In the absence of listing of these new drugs, it is likely that PBS spending would still increase in real per capita terms. PBS growth Many factors have been contributing to the rapid growth of PBS spending. These include: Community expectations, including expectations of access to new and sometimes very expensive drugs; Expansion in effective drug treatments (which relates to community expectations, prescribing patterns and listing of new drugs); The ageing of the population; Increasing costs of drugs, due both the changes in the composition of drugs prescribed and to a movement towards world parity pricing; The growth of the concessional schemes (which relates to increasing income inequality in Australia); Growth arising from higher rates of disease detection (eg diabetes); and The growth of defensive medicine. We might hope that policy would be informed by a full understanding of these factors and an attempt to quantify their importance. In practice little information is shared. There is some attempt by the Department to engage the wider community in a constructive dialogue through the Australian Pharmaceutical Advisory Council (APAC). It appears however that the requisite analysis of the PBS system is not being undertaken. There is concern that Government has been telling GP groups that GP prescribing habits are to be targeted with cost-saving measures in the next budget. This is occurring without substantiating the presumption that GP prescribing is the essence of the problem. 1 2 Australian National Audit Office. 1997, pg 5 Department Health & Ageing, 2001, pg 1 AMA - PBS Discussion paper prepared by Jennifer Thomson & Roger Kilham Feb 2002 2 The nature of the problem is also being over-inflated by the Government. Huge emphasis is placed on last year’s 19% growth. However, the upsurge in pharmaceutical spending is not limited to Australia by any means. Similar surges have been seen in North America and in Europe (although the policy responses are not the same). In the USA, spending on prescription drugs has increased from 6% of national health spending in 1994 to 9.4% in 2000 (representing a growth rate of over 14% p.a.). Private health funds in the US have rapidly increased their funding of pharmaceuticals in the same six years (growing by 21.5% p.a.). It is particularly interesting to note that public health funding of prescription drugs has grown even faster than private health funding. Furthermore, overall spending on pharmaceuticals in Australia is, if anything, below average by international standards. On the latest comparable data available (late 1990s) Australia was spending 1.0% of GDP on pharmaceuticals, the UK 1.1%, Japan 1.3% and the USA 1.4%. Some would say that Australia’s low spend relative to GDP reflects the success of Australia’s funding systems in controlling spending. The dilemma for Government is to find effective interventions that will maintain the integrity of the scheme (and its very significant health benefits) whilst managing the costs in an appropriate way. National Medicines Policy The PBS rests within the Department of Health and Ageing’s National Medicines Policy, which was endorsed by the Council of Australian Governments3 in 1999. The policy has four central objectives: “Timely access to the medicines that Australians need, at a cost individuals and the community can afford Medicines meeting appropriate standards of quality, safety and efficacy Quality use of medicines Maintaining a responsible and viable medicines industry”4 The Government has set up a Committee structure to advise on the implementation of this policy including the Australian Pharmaceutical Advisory Council (APAC) to enable a partnership approach with multi lateral and consensus development of broad advice. The Pharmaceutical Health and Rational Use of Medicines Committee (PHARM) together with the National Prescribing Service (NPS) have taken on a more specific role in the quality use of medicines. The PBS is the mechanism to deliver medicines to the community. The Pharmaceutical Benefits Advisory Committee (PBAC) advises on which drugs should be listed using cost effectiveness principles (from 1994 onwards) and with pricing being determined by the Pharmaceutical Benefits Pricing Authority (PBPA). AMA - PBS Discussion paper prepared by Jennifer Thomson & Roger Kilham Feb 2002 3 4 Department of Health & Aged Care, 2000, pg 1 ibid pg 3 The PBS pathway/ system2 AMA - PBS Discussion paper prepared by Jennifer Thomson & Roger Kilham Feb 2002 3 AMA - PBS Discussion paper prepared by Jennifer Thomson & Roger Kilham Feb 2002 3 The pathway of drug regulation, listing and prescription is a complex system 5. The steps include: a) Application for product registration considered by the Australian Drug Evaluation Committee (ADEC) of the Therapeutic Goods Administration (TGA). The basis for evaluation is quality, safety and efficacy. b) Product information and consumer information are developed and approved at this point. c) Application for listing on the PBS is considered by Pharmaceutical Benefits Advisory Committee (PBAC) of the Department of Health & Ageing (DH&A). The basis for evaluation is comparative safety, efficacy and cost-effectiveness. PBAC determines any restrictions on prescribing including restricted benefits listing and authority-required benefit listing which requires the prescriber to gain approval prior from the Health Insurance Commission (HIC). d) Products are then recommended to the Health Minister for approval. e) The Pharmaceutical Benefits Pricing Authority (PBPA) then negotiates PBS listed prices with the drug sponsor based upon information from PBAC. f) The prescriber who will have been issued a prescriber number by the HIC is able to prescribe drugs listed on the PBS. From this point government has little direct control. Prescribers are largely medical practitioners operating within a unique doctor-patient relationship where both parties are able to make independent choices. g) The patient will choose whether to have the script dispensed. h) The pharmacist will dispense the script with or without consumer medicine information. i) The patient will then choose to use the medicine as prescribed or not. j) Adverse drug reactions can be reported via the Adverse Drug Reaction Advisory Committee (ADRAC). Quality Use of Medicines The Quality Use of Medicines has been one of the principal platforms of the National Medicines Policy. In 1991 the Australian Pharmaceutical Advisory Council (APAC) and the Pharmaceutical Health and Rational Use of Medicines Committee (PHARM) were established in recognition of increasing rates of drug related morbidity and mortality. Over the last 10 years these bodies have driven the Quality Use of Medicines (QUM) policy development with the formation of implementation agencies such as the National Prescribing Service (NPS). The NPS has been responsible for education strategies to promote improved prescribing of medicines. Strategies have included using innovative and successful education with general practitioners particularly through Divisions of General Practice. Specialist doctors have received limited attention although it is known that specialist impact on prescribing behaviour of general practitioner is considerable in some cases. In a recent Australian study it was shown for some drugs specialist initiation was high e.g. proton pump inhibitors at 80%, for others low e.g. diuretics at 8 %.6 5 6 National Prescribing Service, 2001, pg 4 Robertson et al., 2001, pg 409 AMA - PBS Discussion paper prepared by Jennifer Thomson & Roger Kilham Feb 2002 4 Some of the outcomes of the QUM strategies of the last decade have recently been collated. For example, antibiotic use in Australia has been declining with evidence of more appropriate use of antibiotics as well as non steroidal anti inflammatory drug use for osteoarthritis 7 The NPS has a budget of $5 million per annum, a tiny amount compared to the marketing budgets of drug companies. Recent release of high cost new medicines onto the market without prior provision of evidence-based information to the public or prescribers has made it impossible for evidence-based decision making. Although direct marketing to the public of prescription drugs is not permitted, marketing to the public through other means has been highly successful in the release of some recent high cost medicines such as Zyban and Celebrex. The marketing methods to prescribers are numerous and effective. They include pharmaceutical representative detailing and Drug Company sponsored education and other activities. PBS cost framework The cost of the PBS is managed in various ways. While the PBS is currently demand driven and uncapped, controls are in place at various points in the system: 7 8 PBAC evaluation of drugs for listing since 1994 has been based on a cost effectiveness model, which was a world first at the time. In some cases based on PBAC advice, price /volume arrangements may be applied (i.e. the price reduces as volume of usage increases allowing for the fact that research and development costs will have been met once large volumes have been sold). The same pricing principles are applied to all PBS prescriptions. Under brand premium arrangements, the Commonwealth reimburses pharmacists based on the lowest priced brand. Under the therapeutic group premium arrangements, which apply for some therapeutic groups of drugs, reimbursement to the pharmacist is based on the lowest priced benefit within the identified therapeutic groups. Reimbursements to the pharmacist are managed by the HIC, which gathers data on these reimbursements 8. The cost to the patient is determined by the patient’s health concession card status. Currently some 79% of PBS costs are to concession cardholders whose maximum co-payment is currently $3.50 per script. The general maximum co-payment rate is $21.90. A safety net provision applies to high users of medicines with the current threshold as $669.70 for general users and $182.00 for concession cardholders. Because the Government has increased access to concessional health cards (including self-funded retirees subject to a generous income limit), public spending on the PBS has tended to outstrip patient spending (on the co-payments). Once patents expire, generic drug prices are renegotiated for PBS listing. PHARM.APAC DHAC, 2001, pg 45 Department of Health &Aged Care, 2001, pp36 AMA - PBS Discussion paper prepared by Jennifer Thomson & Roger Kilham Feb 2002 5 Cost effectiveness In 1994, the PBS internationally pioneered the use of a model cost effectiveness for the evaluation of all drugs being submitted for inclusion on the PBS. Despite such an approach, no Australian studies are available measuring the influence of the PBS on health outcomes. It is understood that what government is buying through it National Medicines Policy and therefore the PBS should be improved health outcomes at an acceptable price. Some studies in the US have measured pharmaceutical formularies and their impact on health outcomes in Health Maintenance Organisations. Similar studies must occur in Australia to inform rational policy decisions regarding the PBS. The cost effectiveness data and research made available to the PBAC in assisting it with its recommendations on listing is not made available generally. Transparency in these processes is needed to evaluate their effectiveness. There are some concerns that many of the trials and research justifying PBAC decisions may not be undertaken in a “real world” context. Post drug release research is also important in ongoing review of drugs on the PBS. In many instances, it is clear that pharmaceutical interventions are more cost effective than some surgical interventions eg treatments in peptic ulceration. Death rates for peptic ulcers have decreased markedly.9 Drug therapies have been critical in control of progression of major disease states such as diabetes, cardiovascular disease and mental health. Focus on such diseases within the National Health Priorities and implementation of current strategies in these areas will inevitably lead to further costs in the PBS. It is anticipated that 50% of diabetics are undiagnosed and with the current strong policy to identify diabetes, then short to medium term pressures on diabetic drugs will occur. However the enormous potential savings in long term disease progression and complications are enormous and must be recognised. It is not clear that integrated planning or policy development is occurring across government. The likely cost implications on the PBS of the current National Health Priorities are not being articulated. Drivers for PBS growth There are many possible drivers for PBS cost growth. Some might include: Increasing access to concession status eg 2001 budget Commonwealth Seniors’ Health Card entitlements. New listings such as Celebrex and Zyban with a trend to more expensive listings. Drug choice of new and more expensive drugs. Leakage (Doctors prescribing of PBS drugs for other than approved conditions) is probably increasing although there is little hard data available on this. It was estimated that proton pump inhibitors should be used by less than 35,000; in fact 177,000 people are receiving such medication costing an extra $220 mill per annum.10 As previously mentioned, these drugs are largely initiated by specialists who are not receiving the benefit of NPS education. 9 PHARM.APAC DHAC, 2001, loc. cit Department of Health & Ageing, 2001, pg 5 10 AMA - PBS Discussion paper prepared by Jennifer Thomson & Roger Kilham Feb 2002 6 Changing demographics of the population eg ageing population with the over 65 age group likely to double in the next fifty years. This group is the high user group. Disease patterns are constantly changing with demand for appropriate treatment interventions likely to be affected. The numbers estimated to be depressed or asthmatic in the population has increased. Disease prevalence and detection of diabetes has trebled in the last 20 years. A number of government strategies are in place around the National Health Priorities to increase identification and effective treatment of such patients. This will inevitably impact on the PBS. Drug trials on which decisions to list on the PBS are based, may not take into account these other trends and strategies. Marketing strategies of the industry are becoming more sophisticated and are well resourced. Other drivers have been mentioned previously and include the expansion of effective drug therapies for many of the chronic diseases, increasing community expectations around drug accessibility and the rise in the practice of defensive medicine. Prices paid for drugs The prices paid for drugs in Australia have been low compared to other OECD countries. Some of the increasing cost of the PBS can be attributed to a 1990s policy of moving drug prices closer to world parity prices. Part of the logic for this has been to sustain a viable Australian pharmaceutical industry. However, it is unlikely that any Australian Government would ever meet drug company hopes for prices. Pharmaceutical companies are far more profitable, on average, than companies in the remainder of the economy. The rapid rate of technological change may be one of the factors underpinning this profitability. In comparison with most other industries, the drug companies have a much higher proportion of their output protected by patent at any point in time. Most of the companies are large multinationals with considerable market power. In the USA, the companies enjoy very significant political influence, which they wield to protect their position and their profits. It is difficult for any one country to unilaterally influence the behaviour of drug companies. AMA endorsed principles relating to the PBS The AMA has been concerned at the rising costs and the potential risks to doctors and patients alike if the PBS is substantially changed by future government interventions. As such the Federal Council at its meeting in July 2001 passed several resolutions: That Federal Council supports the principles of the Pharmaceutical Benefits Scheme (PBS) to provide universal access to medicines for the public in an effective, efficient and equitable manner. That Federal Council urge that solutions to the funding crisis in the Pharmaceutical Benefits Scheme (PBS) be urgently found with input from the Government, the pharmaceutical manufacturers, the AMA and patients. AMA - PBS Discussion paper prepared by Jennifer Thomson & Roger Kilham Feb 2002 7 That Federal Council supports that the direction for such solutions include ensuring: a) The independence of the Pharmaceutical Benefits Advisory Committee and extending its role to incorporate a special pricing review subcommittee; b) The transparency of the listing process; c) Adopting evidence-based economic and clinical risk benefit review of already listed drugs; d) Improved prescribing decision support, patient information; and e) Monitoring the marketing methods of the manufacturers.11 Current government concerns The current growth in PBS expenditure is alarming government, with PBS growth of 259% over the last decade compared to the Medicare Benefits Schedule growth of 73%. These total change growth figures must be viewed in the light of the changes from cash to accrual accounting by Government. Growth would be better expressed as average annual real per capita growth rates to give a more realistic assessment of the situation. The PBS currently represents 15.4% of Commonwealth’s $27 billion annual health expenditure (at $4 billion) and last year was the fastest growing area of health budget, with a growth rate of 19% ($700 mill) in 2000/01, around half of that growth being attributed to lipid lowering drugs ($100 mill), Celebrex ($160 mill) and Zyban ($65 mill).12 However, growth is not expected to continue at 19% p.a. The underlying trend growth rate is more of the order of 10 to 11% pa. The Government has budgeted on PBS spending increasing by 8.0% for 2001-02. As mentioned, the trend growth is not unlike other equivalent countries and Australia is still a relatively modest spender on pharmaceuticals. Canadians spent $12 billion on prescription medicines in 2001, five times that spent in the mid 1980s.13 Physicians’ services and prescription drugs now generate equivalent total costs in Canada, while the ratio is still at 2:1 in Australia. The average cost per script is growing. In last 10 years in Australia, the cost per script has grown by 126% and volume of scripts by 54%. In 2000/1 volumes of scripts grew by 7% and cost per script by 12%.14 As in Canada the newer drugs are more expensive. In 1999 in Canada 60 % of prescriptions were for products of over 15 years of age, with the costs for these scripts only at 22% of the total. It would be worth exploring the relative use of older, cheaper, effective drugs in Australia. A systems approach Analysis of the cost increases in the PBS requires a system approach with the understanding that intervention or change at any point in the system will affect the 11 AMA Federal Council. 2001 Department of Health & Ageing, 2001, pg 2 13 Morgan , 2001, pg 1508 14 Department of Health & Ageing, 2001, pg 4 12 AMA - PBS Discussion paper prepared by Jennifer Thomson & Roger Kilham Feb 2002 8 system as a whole and often in ways that are not anticipated. Many have been advocating a more “holistic” approach to health care policy over the years. 15 However it is clear that no one intervention will achieve the cost containment. Evidence of effective strategies to date must be considered in the choice of interventions. Future approach to the PBS 1. The system The AMA strongly supports the PBS and is concerned that any future strategies for development of the PBS be strategies that enhance the strengths of the system, rather than change the current system. There is potential danger in the AMA aligning itself too closely with Government policy focussed mainly on control of PBS spending. Given the technological developments, the best health outcomes may indeed require pharmaceutical spending to increase as a proportion of total health spending. If new pharmaceuticals can achieve the results they aim to achieve, then doctors will want their patients to have access to them, and will expect their representative organisations to emphasise health outcomes and quality care. The AMA reiterates that it supports the principles of the Pharmaceutical Benefits Scheme (PBS) to provide universal access to medicines for the public in an effective, efficient and equitable manner. As such the AMA would support future approaches that strengthen the current checks and balances in the system rather than any major change. 2. Research and Evaluation Decisions around health policy should be based on best possible research and evaluation. There is a gap in Australian based research on PBS impact on health outcomes. There are also limited data sources for effective monitoring and evaluation of the PBS with sources such as HIC data consisting of billing data and not linked to disease states. The AMA recommends that: The Government properly fund Australian based research on PBS impact on health outcomes; and Development of data sources for effective monitoring and evaluation of the PBS. 3. Integrated health policy It is important in health policy development to take a systematic approach to change. The National Health Priorities (NHP) have set a framework for the development of 15 Leeder and McAuley, 2000, pg 50 AMA - PBS Discussion paper prepared by Jennifer Thomson & Roger Kilham Feb 2002 9 health policy in Australia. It is not clear that the impact of the strategies on the National Medicines Policy and particularly the PBS has been considered. The AMA recommends that a systems based approach be taken to health policy development and that the National Medicines Policy including the PBS be linked to other health policy eg the National Health Priorities. 4. PBAC processes The transparency of the PBAC processes has remained of some concerns to stakeholders. This has included issues such as objective membership of the Committee, transparency of the process where reasons for decisions cannot be released and where important evidence-based information is not made available to prescribers or users prior to drug release. The AMA supports increasing the independence and transparency of the drug listing process and improving the supply of evidence based information to prescribers and consumers in a timely fashion at the point of drug release. 5. Drug listing review The PBS introduced a world leading and innovative process of drug listing in 1994 when it required all new drugs to be evaluated against a cost effectiveness framework. Drugs listed prior to 1994 have not undergone such evaluation. There may be a case for looking at some of the pre-1994 drugs using a cost effectiveness evaluation model. The evidence-based medicine approach that underpins the QUM strategies has already resulted in significant changes in prescribing practice. There are clear risks in withdrawing well-used drugs for industry, health professionals and consumers. These probably represent the majority of prescription drugs. Canadian figures in 1999 indicated that 60% of scripts were for drugs at least 15 years old.16 The AMA supports the adoption of an evidence based economic and clinical risk benefit review of listed drugs that have not yet undergone such review. 6. Quality Use of Medicines The QUM approach has been important in setting the framework for evidence-based prescribing in Australia. Much of the information available to doctors is produced and distributed by drug companies who obviously have a vested interest in marketing their products and spend large resources on such promotion to the public indirectly as well as to the prescriber very directly. As an alternative, the NPS has provided an objective evidence-based source of information to prescribers (mostly general practitioners) and increasingly to pharmacists and consumers. It is clear that all participants have some responsibility in responsible prescribing. The doctor cannot become the defacto regulator of the system through an increasing process of authority prescription restrictions. Such restrictions require increased consultation time with patients and increased administration time for the practice. 16 Morgan, loc. cit AMA - PBS Discussion paper prepared by Jennifer Thomson & Roger Kilham Feb 2002 10 The AMA supports improved prescribing decision support and patient information. The principles of evidence-based medicine must apply to such strategies and increased resourcing must be provided to ensure timely and effective delivery of evidence to the point of clinical decision making for both general practitioners and specialists. The AMA recommends monitoring the marketing methods of manufacturers to both the public and health professionals. The AMA does not support increasing the number of new drugs being listed as authority prescriptions where the prescriber is being used as the primary mechanism for cost containment of that new drug. The responsibility for evidence-based usage of drugs rests with all stakeholders including government, the industry, health professionals and the consumer. 7. Signals for consumers Patient co-payments are typically set higher for pharmaceuticals than they are for doctor consultations. Australia is by no means alone in using this strategy, although it may go a bit further than other comparable countries (Canada and the UK aside) in attempting to avoid price signals for GP visits. However, patient co-payments have little use as a tool for managing demand because the demand for prescription drugs is referred demand (driven by the actions and the authority of the doctor). Therefore, the main purpose in applying patient co-payments is to share the financial risk of the PBS with householders. The only change of any significance in Australia’s co-payment policy in recent years has been the inclusion of many self-funded retirees in the concessional part of the PBS scheme (the Seniors Health card). This is subject to a generous income limit and, as noted earlier, it has resulted in the Federal Government increasing its share of the cost of the PBS. Even without any change in policy, the Federal Government’s share was increasing because of growing income inequality in Australia. Over time a higher proportion of the population has qualified for some sort of benefit, and therefore for a health care card of one sort or another. In this context, the PBS is not just a scheme for providing access to pharmaceuticals. It is also part of the overall social policy framework, and is used to redistribute income within the community. Aggregate demand for pharmaceuticals may be little affected by higher patient price signals. In the USA, for example, the sharing of the financial burden is radically different to that in Australia: Sharing the Financial Burden of Prescription Drugs USA versus Australia (percentage of funding) USA (1) Australia (2) Patient out-of-pocket 32% 16% Private health insurers (3) 46% 0% Government subsidies 22% 84% Total Footnotes: AMA - PBS Discussion paper prepared by Jennifer Thomson & Roger Kilham Feb 2002 11 (1) Prescription drugs. Source: CMS Health Expenditure database. (2) Benefit-paid pharmaceuticals. Source: AIHW Health Spending Bulletins. (3) Private health insurers in Australia do pay modest benefits on drugs, which do not attract a PBS benefit. However, higher price signals will have a deleterious effect on those with very low incomes. There is ample evidence from the USA that access to pharmaceuticals is very uneven, with some groups having little access which other groups are very high users. Ultimately this is a social policy issue and is about equitable access to quality health care. Labelling of dispensed medicines with information about their real cost has been trialed in some European countries. Effects of such labelling included consumers demanding the higher cost drugs, as these were perceived as “better” drugs. Clearly any mechanisms for sending signals to consumers need careful consideration. The AMA recommends exploring mechanisms for increasing direct consumer knowledge and responsibility for costs of new medicines. Bibliography AMA Federal Council, 2001. Minutes of AMA Federal Council meeting, 27-28 July 2001, Australian Medical Association, Canberra Australian National Audit Office, 1997. Pharmaceutical Benefits Scheme - Auditor General Performance Audit Report No 12, 1997-8. ANAO, Canberra Department of Health & Ageing, 2001. APAC Speaking Notes on the PBS, APAC 23 Nov 2001, DH&A., Canberra Department of Health & Aged Care, 2000. Australian Pharmaceutical Advisory Council 2000 –2002, Ausinfo, Canberra Department of Health & Aged Care, 2001. Schedule of Pharmaceutical Benefits August 2001, Ausinfo, Canberra Leeder, S. and McAuley, I., 2000.The future of Medicare and health service financing. MJA, July 3 Vol 173, No 1, pp. 48-51 Morgan, S., 2001. Statistics and drug utilization: Are prescribing rates really that high? CMAJ, Nov 27, 2001; 165 (11) pp. 1507-8 National Prescribing Service., 2001. NPS news, 19 December 2001, Surrey Hills, NSW PHARM & APAC, DHAC, 2001. Quality Use of Medicines: A Decade Of Research, Development and Service Activity 1991 – 2001. Quality Use of Medicines and Pharmacy Research Centre, University of South Australia, Adelaide Robertson, J et al., 2001. The impact of specialists on prescribing by general practitioners, MJA, Vol 175 No 8, pp. 407-411 AMA - PBS Discussion paper prepared by Jennifer Thomson & Roger Kilham Feb 2002 12 Resolutions from Australian Medical Association Federal Council Feb 02 Pharmaceutical Benefits Scheme 1. The AMA reiterates that it supports the principles of the Pharmaceutical Benefits Scheme (PBS) to provide universal access to medicines for the public in an effective, efficient and equitable manner. As such the AMA would support future approaches that strengthen the current checks and balances in the system rather than any major change. 2. The AMA supports the right of all Australians to be prescribed quality medications in a timely and user friendly manner. 3. The AMA recommends that the Government properly fund Australian based research on PBS impact on health outcomes and the development of data sources for effective monitoring and evaluation of the PBS. 4. The AMA recommends that a systems based approach be taken to health policy development and that the National Medicines Policy including the PBS be linked to other health policy eg the National Health Priorities. 5. That AMA recognises the Government’s ability to control the cost of the PBS, but any changes should be on the basis of scientific evidence and “ proper” economic modeling of health. 6. The AMA supports increasing the independence and transparency of the drug listing process and improving the supply of evidence based information to prescribers and consumers in a timely fashion at the point of drug release. 7. The AMA supports the adoption of evidence based economic and clinical risk benefit review of listed drugs that have not yet undergone such review. 8. The AMA supports improved prescribing decision support and patient information. The principles of evidence-based medicine must apply to such strategies and increased resourcing must be provided to ensure timely and effective delivery of evidence to the point of clinical decision making for both general practitioners and specialists. 9. The AMA recommends monitoring the marketing methods of manufacturers to both the public and health professionals. 10. The AMA does not support increasing the number of new drugs being listed as authority prescriptions where the prescriber is being used as the primary mechanism for cost containment of that new drug. The responsibility for evidence-based usage of drugs rests with all stakeholders including government, the industry, health professionals and the consumer. 11. The AMA rejects any suggestion that doctors are deliberately prescribing in any way other than in their patient’s best interest. 12. The AMA recommends exploring mechanisms for increasing direct consumer knowledge and responsibility for costs of new medicines. 13. The AMA urges Federal Council to mount a campaign, in collaboration with the consumer health organisations, to oppose bureaucratic, restrictive, prescribing regulations.