Document
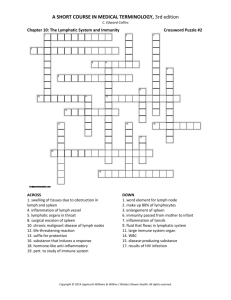
advertisement
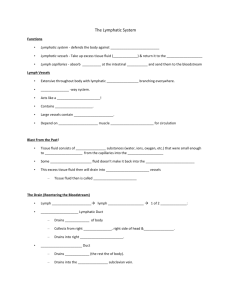
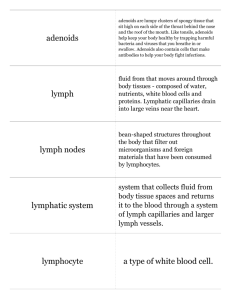
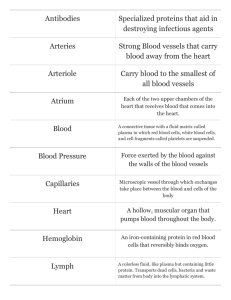
Ch. 21: Lymphatic and Immune Systems I. Lymphatic System An open system of vessels. Functions: fluid recovery; immunity; lipid absorption and transport. Components: lymph; lymph vessels; lymphatic tissue; lymphatic organs. (A) Lymph and Lymphatic Vessels Lymph similar to plasma but with less protein. Collected by lymph capillaries (extra leaky). Vessels similar to veins. Capillaries -> collecting vessels -> lymphatic trunks -> collecting ducts = right collecting duct and thoracic duct (on left), which is larger. Flow similar to venous flow. Enhanced with surrounding muscle contraction, valves. (B) Lymphatic Cells and Tissue -1- T Cells -2- B Cells -3- Macrophages: display foreign antigens (Ags), one type of ‘antigen presenting cell’ (APCs). -4- Dendritic cells: APCs in skin (Langerhans), mucous membranes and lymphatic organs. -5- Reticular cells: branched, help form stroma of lymphatic organs, act as APCs in thymus. Diffuse lymphatic tissue throughout body, often called MALT (mucosa associated lymphatic tissue). Also forms nodules (transient) and clusters (Peyers patches). (C) Lymphatic Organs -1- lymph nodes: cleanse lymph and notify immune cells of pathogens. Many in cervical, axillary, inguinal areas. Also in body cavities. Divided into compartments by connective tissue. Contain lymphocytes and APCs. Afferent and efferent lymphatic vessels. When swollen = lymphadenitis. -2- tonsils: crypts lined with nodules. b. palatine c. lingual a. pharyngeal = adenoids -3- thymus: lymphatic and endocrine functions. T Cell development. -4- spleen: red pulp with RBCs; white pulp with lymphocytes and macrophages. Filters blood, removes aged RBCs. Vulnerable location. II. Nonspecific Resistance Defenses against pathogens: disease-causing organisms. External barriers, antimicrobial mechanisms, immune system. 19 (A) External Barriers: skin, mucous membranes, secretions: tears, sweat, saliva, gastric….. (B) Leukocytes and Macrophages – phagocytic -1- leukocytes a. neutrophils – combat bacteria with respiratory burst, uses lysosomes to release toxins. Create killing zones. b. eosinophils – phagocytize Ag/ Ab complexes, allergens, combat parasitic worms. c. basophils – release heparin and histamine to enhance action of other WBCs. d. lymphocytes – NK cells nonspecific, combat cancerous or infected host cells. Immunological surveillance. Secrete perforins. -2- macrophages Include histiocytes in loose CT; dendritic cells in skin; microglia in CNS; alveolar macrophages; hepatic macrophages. (C) Antimicrobial Proteins -1- interferons: inhibit viral reproduction. -2- complement: at least 20 proteins, activated by pathogens. Results in enhanced inflammation, opsonization: makes bacteria easier to phagocytize, cytolysis. (D) Inflammation – redness, swelling, heat and pain triggered by chemicals such as histamine, leukotrienes. Three processes: -1- mobilization of defenses: vasodilation, hyperemia. Leukocyte diapedesis. -2- containment and destruction of pathogens. Chemotaxis attracts neutrophils. -3- tissue cleanup and repair. Monocytes transform into macrophages. Edema, pus- collects in abscesses. (E) Fever = pyrexia. Adjective: febrile. WBCs release pyrogens. Promotes interferons, increases metabolism, inhibits microbial reproduction. III. Specific Immunity Overview Advantages = specificity and memory. 20 (A) Forms of Immunity -1- Cell mediated: direct attack of ‘suspicious’ cells. Results in lysis or enhancement of non-specific defenses. -2- humoral = antibody mediated. a. natural active – sickness experience. b. artificial active – vaccination c. natural passive – via placenta, milk. d. artificial passive – gamma globulin injections. No memory with passive forms. (B) Antigens Molecules which trigger immune responses. (C) Lymphocytes T and B Cells (D) Antigen Presenting Cells Present Ags on MHC (major histocompatability complex) Proteins, which are genetically programmed. (E) Interleukins – released by WBCs. IV. Cellular Immunity Involves Cytotoxic T Cells = Killer Ts; Helper Ts; Suppressor Ts; Memory Ts. (A) Recognition -1- antigen presentation: occurs in lymph nodes. Cytotoxic and Helper Ts respond to APCs. -2- T Cell Activation: costimulation (double check) results in clonal selection. (B) Attack -1- Helper Ts: attract neutrophils and NK Cells, macrophages. Stimulate T and B Cell mitosis and maturation. -2- Cytotoxic T Cells: directly attack and kill infected cells, transplants, cancer cells. -3- Suppressor Ts: inhibit T and B Cells as pathogen disappearing. Prevents autoimmunity. (C) Memory - Some Cytotoxic and Helper Ts become memory cells. Create much faster response upon secondary exposure. 21 V. Humoral Immunity (A) Recognition – B Cells bring antigens in via receptor-mediated endocytosis, then display some on MHC proteins. If Helper Ts bind, they activate B Cells into clonal selection. Most are plasma cells, which produce antibodies (2000/ sec). (B) Attack – antibody (Ab) structure: four polypeptides, two heavy & two light, each with variable (forms AG bindings sites) and constant regions. -1- Five Ab Classes a. IgA in secretions- blood, mucous, saliva, tears, milk….. b. IgD on B Cell membranes c. IgE in tonsils, skin, mucous membranes. d. IgG are most circulating Abs, cross placenta. e. IgM on B Cell membranes. Can be customized via different combinations of ~35,000 genes. -2- mechanisms a. neutralization: AB binds to pathogenic portion of Ag. b. complement fixation: IgM and IgG expose foreign cells to complement . c. agglutination: prevents spread of pathogens. d. precipitation: follows agglutination. (C) Memory – Memory B Cells responsible for much faster secondary response. VI. Immune Disorders (A) Hypersenitivity – allergies = responses to allergens. Most common is Type I (acute). May lead to anaphylaxis. (B) Autoimmunity – failures of self-tolerance. Rheumatoid arthritis; Type I DM; lupus; MS,…. (C) Immunodeficiency SCID; AIDS – infects Helper Ts, dendritic Cells and macrophages. Problem = opportunistic infections. 22