THE URINARY SYSTEM dissection
advertisement

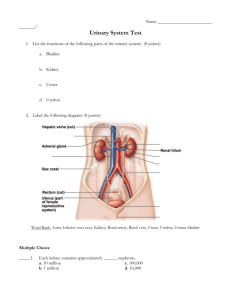
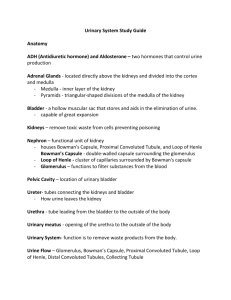
THE URINARY SYSTEM: KIDNEY STRUCTURE AND FUNCTION Purpose: Introduction: The kidneys are responsible for the elimination of most of the waste products from the metabolism of nitrogen-containing compounds such as urea and creatinine from protein catabolism, as well as ketone bodies from fat catabolism. The difficulty of this kidney function is compounded by the fact that the kidney also reabsorbs molecules necessary for normal body function such as glucose, amino acids, and bicarbonate. The kidneys are involved in the maintenance of a constant internal environment (homeostasis) of electrolyte (salt) concentrations, fluid balance, and acid-base balance. The fluid volume of the blood is maintained by the reabsorption of 98-99% of the water that leaves the blood in the initial step of urine formation, while the electrolyte and pH balance of the blood is maintained by the selective reabsorption of such ions as Na+, K+, Cl- and HCO3-. Organs of the Urinary System Figure 1.1 illustrates the components of the urinary system with its principal blood supply. It consists of two kidneys, two ureters, the urinary bladder, and a urethra. The kidney is an anteroposteriorly compressed lima bean-shaped organ embedded retroperitoneally in a fatty fibrous pouch lateral to the vertebral column. The kidney is high in the abdominal cavity, between the levels of the twelfth thoracic and the third lumbar vertebrae. The left kidney is usually slightly higher than the right due to the large area occupied by the liver. Each kidney is supplied blood through a renal artery that is a branch of the abdominal aorta. Blood leaves each kidney through a renal vein that empties into the inferior vena cava. Figure 1.1 Urinary System Label the designated structures. Renal artery and vein - vessels that transport blood to and from the kidney. Kidney - paired organ located lateral to the vertebral column; high in the abdominal cavity. Ureter - tube that transports urine from the kidney to the urinary bladder. Urethra - tube that transports urine from the urinary bladder out of the body. Bladder - distensible sac in the pelvic cavity, just posterior to the pubis symphysis; stores urine Urine passes from each kidney to the urinary bladder through a ureter. The upper end of each ureter is enlarged to form a funnel-like renal pelvis. The lower end of each ureter enters the posterior surface of the bladder. Leading from the urinary bladder to the exterior is a short tube, the urethra. In males the urethra is about 20 centimeters long; in females, it is approximately 4 centimeters in length. The exit of urine from the bladder is called micturition. Two sphincter muscles control the passage of urine from the bladder. The sphincter viscae is a smooth muscle sphincter that is near the exit of the bladder. When approximately 300 ml of urine has accumulated in the bladder, the muscular walls of the bladder are stretched sufficiently to initiate a parasympathetic reflex that causes the bladder wall to contract. These contractions force urine past the sphincter vesicae into the urethra above the sphincter urethrae. This second sphincter, located approximately 1-3 centimeters below the sphincter vesicae, consists of skeletal muscle fibers and is voluntarily controlled. The presence of urine in the urethra above this sphincter creates the desire to micturate; however, since the valve is under voluntary control, micturition can be inhibited. When both sphincters are relaxed, urine passes from the body. Kidney Anatomy Figure 1.2 reveals a frontal section of a mammalian kidney. Its outer surface is covered with a thin fibrous renal capsule. In addition to this thin covering, the kidney is provided support and protection by a fatty capsule that completely encases it. Figure 1.2. Longitudinal section of a kidney. Immediately under the capsule is the cortex of the kidney. The cortex is reddish-brown due to its great blood supply. The lighter inner portion is called the medulla. The medulla is divided into several coneshaped renal pyramids. Cortical tissue, in the form of renal columns, extends down between the pyramids. Each renal pyramid terminates as a renal papilla, which projects into a calyx. The calyces are short tubes that receive urine from the renal papillae; they empty into the large renal pelvis. Procedure: Sheep Kidney Dissection 1. Obtain a sheep kidney. If the kidney is still encased in fat, peel off this adipose layer carefully. As you lift the fat from the kidney, look carefully for the adrenal gland, which should be embedded in the fat near one end of the kidney. Remove the adrenal gland from the fat and cut it in half. Note that the gland has a distinct outer cortex and inner medulla. 2. Identify the renal vessels and the ureter. 3. The shiny covering of the kidney is the renal capsule. Probe into the surface of the kidney with a sharp dissecting needle to see if you can differentiate the capsule from the underlying tissue. 4. With a scalpel, slice the kidney longitudinally to produce a frontal section (posterior and anterior halves) similar to Figure 1.2. Identify the following structures. Call me over to verify that you have located each structure. Renal cortex Renal medulla Renal papilla Renal Pyramids Renal pelvis Renal artery Renal vein Ureter Histological examination of renal tissue The basic functional unit of the kidney is the nephron. Figure 1.3 illustrates a single nephron in detail. It has been estimated that there are around one million nephrons in each kidney. Approximately 80% of the nephrons are located in the cortex; these are called cortical nephrons. The remainder are the juxtamedullary nephrons which are located partially in the cortex and partially in the medulla. Figure 1.3. Diagram of a nephron. Each nephron is composed of two parts: 1) the glomerulus, which is a tightly woven, highly permeable capillary bed at the end of an arteriole; and 2) the renal tubule, which is a bent and convoluted tube composed of kidney cells. The mouth of the renal tubule (Bowman's capsule) envelops the glomerulus. The last part of the renal tubule (the collecting duct) empties its contents into the renal pelvis, which funnels urine to the ureters. The formation of urine in the nephron can be divided into two stages. 1) The hydrostatic pressure of the blood squeezes fluid out of the capillary wall of the glomerulus, producing an ultrafiltrate of blood. Except for proteins, which are usually too large to leave the capillaries, the glomerular filtrate contains the same solute molecules as plasma and is isotonic to plasma. 2) As the glomerular filtrate passes through the renal tubules, the cells of the tubules selectively reabsorb solute molecules and ions. The solution that emerges at the end of the collecting duct (urine) is thus very different in composition and concentration from the solution that enters the tubule (glomerular filtrate). In the adult human, 180 liters of filtrate are produced each day, but the daily urine output is only 0.6 to 2.0 liters. If we assume that the plasma volume is 3 liters, the production of 180 liters of filtrate means that all of the blood plasma must be filtered through the glomeruli once every 40 minutes or 60 times in 24 hours. Therefore, 178 to 179 liters of fluid must be reabsorbed along with many solutes, a huge energetically expensive process.