Normal menstrual cycle

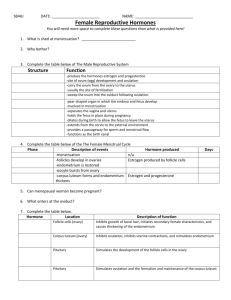
Normal menstrual cycle
Reproduction relies on a complex system of communications between the hypothalamus, pituitary and the ovarian follicular development and ovulation. Sex steroid hormones provides regularity of the phases of the reproductive cycle.
Normal ovulation depends on the complex and interactive hypothalamic — pituitary — ovarian system.
There are responsible changes during the complete reproductive cycle in the target organs: endometrium, breasts, vagina, fallopian tubes. Nervous and endocryne systems undergo cyclic changes too.
In response to the changes, sex steroid hormones are secreted during the ovarian cycle ( follicular maturation, ovulation, development of corpus luteum). There are four main stages of the endometrial cycle: desquamation that is menstruation, regeneration, proliferation, and secretion phases. Due to these changes reproductive function can be perfomed: ovulation, fertilization, implantation and emryo development. If implantation doesn't occur functional layer of the endometrium desquamates and the menstrual bleeding begins.
Regular menstrual cycle is a sign of normal function of female reproductive system.
The rythm is genetically determinated and healthy women have it stable during reproductive age. The first day of menstrual bleeding is considered to be the first day of the menstrual cycle.
The modal interval when menstruation occurs is considered to be 27-29 days and may vary from 21 till 35 days.
The duration of menstrual flow is 3-4 days (from 2 till 7 days)
The amount of blood lost is about 50-150 ml per cycle.
The menstruation must be regular, painless.
The reproductive cycle has two phases.
Regulation of menstrual cycle
The function of reproductive system is controlled by the complex of brain cortexhypothalamus, composed of the groups of nerve fibers and cells in which biogenic
amines, steroid hormones and gonadotropins perfom reception, translation and transmission of signals from environment and organism. This system has 5 levels and is regulated by feedback mechanisms, while high level structures control the lower level.
V-level is suprahypothalamic cerebral structures . The menstrual cycle is regulated by brain cortex. Stress or climatic changes can cause abnormalities of ovulation and menstrual cycle. Receiving of information from environment and interreceptions with neurotransmitter structures of central nerves system sends impulses to neurosecretory hypothalamic nuclei.
IV level—hypothalamus.
Hypothalamic nuclei produce the specific neurohormones, which stimulate pituitary (called as Liberins) and inhibit it (called
Statins). Hypothalamic ventromedial, arcuate and dorsomedial nuclei produce such hormones as Luhberin — releasing hormone that stimulates luteomzmg hormone (LH) secretion and Foliberin — releasing hormone that stimulates follicle-stimulating hormone (FSH) secretion by the anterior pituitary.
Gonadotropic liberins mark as GT-RH (gonadotropic releasing hormones) because only they stimulate the pituitary LH and FSH secretion.
The hypothalamus is the pulse generator of the reproductive clock. There is a network of neurons in the anterior and medial parts of the hypothalamus that produces
GT-RH. The drops of this neurosecretion have been released from the ends of the bram medial emmentia neurons. GT-RH reaches the anterior pituitary gland through the hypothalamic-pituitary portal plexus. Another goes via veins that flow through dura mater sinuses "to the general flow.
Besides GT-RH, there are hypothalamic prolactin-releasing factors and depressing substances which contain dopamine. As hypothalamus responds to steroid hormones secretion with estradiol production, there is a negative feedback which has been controlled by vertebral arteries. There are estradiol receptors in the arcuate nucleus of hypothalamus. Pulsative infusion of GnRH at 70-90-minutes intervals depends on the level of estradiol hormones.
III. level—anterior pituitary . Anterior pituitary produces such gonadotropin hormones as follicular-stimulating hormone, luteinizing hormone, prolactin and other
tropin hormones such as tireotropic, somatotropic, adrenocorticotropic and lipotropic.
Basophilic cells of the peripheral areas of the anterior pituitary produce FSH. By the chemical structure it is a glycoproteid which has been stimulating the growth and maturation of follicles and follicular fluid secretion.
The basophilic cells of the anterior pituitary central area produce LH. It responds massive estradiol secretion, follicular rupture, ovulation, corpus luteum formation and progesterone production.
Prolactin is a polypeptide. It has opposite function as FSH and LH have had. It responds to breast and target organs growth, maturation and milk secretion.
II level — ovaries . An ovary is a target organ for the pituitary hormones. Ovaries respond to pituitary gonadotropin secretion. Ovarian follicles are the basic anatomophysiologic structure of the ovarian theca.
At birth, human ovary is filled with approximately one million primordial follicles.
Each follicle contains an oocyte that is arrested in the prophase stage of meiosis. A single layer of pregranulosa cells surrounds the oocyte, which become the granulosa cells. Premordial follicle is surrounded by basilar membrane that is called hematofollicular barrier. The last one protects oocyte from the uncontrolled influence.
The next stage of the development is the transformation of premordial follicle into the primary one. It occurs as a result of excessive reproduction of granulosa cells which contain mucopolysaccharide. The last one forms a special brilliance membrane, which surrounds the oocyte. It is the second protective barrier. As a primary follicle is stimulated, the pretheca cells form two layers — internal (theca interna) which is situated near basilar membrane and secretes hormones and external layer (theca externa). Primary follicle is transformed into antral follicle that contains follicular antrum between the ovum and granulosa cells.
Dominant follicle is the final stage of the follicular maturation. Antral follicles can be transformed into dominant follicles. The follicles undergo ovulation or degeneration.
At the period of puberty only 200 out of 400 000 follicles undergo maturation. Rest of them degenerate.
During the complete reproductive cycle one oocyte is brought to maturity before
ovulation. In the process of bringing one oocyte to maturation, a number of oocytes are stimulated to partial maturation but subsequently undergo atresia before reaching ovulation.
Ovarian cycle
An ovarian cycle consists of two phases. The first one —follicular phase, the second — luteal phase. There is an increase of FSH, which stimulates the growth and maturation of follicles in the first phase (fig. 14). It lasts 14 days in 28-days reproductive cycle, 10-11 days in 21-days reproductive cycle, and 17-18 days in 35days reproductive cycle.
In the beginning of this phase follicle consists of ovum which is surrounded by the thick membrane. It is 2-2,5 mm in diameter. An ovum increases in its sizes and has brilliante membrane in the surface that is called zona pellucida. An ovum is packed with biochemicals that new organism will use until its own genes begin to function. These biochemicals include proteins, RNA, ribosomes, lipids and the molecules that influence cell specialization in the early embryo. An ovum can be an impressive storehouse and it becomes maturate after two-cell divisions in meiosis I, the primary oocyte is divided to form a small polar body and a large haploid secondary oocyte. In meiosis II, reductional secondary oocyte is divided to yield another small polar body and a mature ovum.
Polar bodies are absorbed by the woman's body and normally play no further role in the development. Follicle granulosa membrane forms as a result of follicle cells proliferation. By that time in the central part of these cells the cavity is formed. The last one contains follicular liquid. Granulosa cells those form corona radiata surround an ovum. It is situated in the numerous cells which have been situated near the follicle.
This number of cells is called a cumulus oophorus. The follicular fluid contains follicular or estrogenic hormones.
The dominant follicle reaches a diameter of 12-20 mm. As the dominant follicle enlarges and follicular fluid accumulates in it, it grows and rupture. It is the final stage of the follicular phase, which is called ovulation. Ovulation is the process when the membrane of mature follicle is ruptured and oocyte is expelled from the follicle.
Oocyte gets into abdominal cavity and is taken by the uterine tube fimbrias.
Process of fertilization takes place in the uterine tubes. After ovulation the dominant follicle transform into the corpus luteum. The second luteal phase of the reproductive cycle begins. There is luteinization — the conversion of granulosa and theca cells to luteal cells with the acquinisation of LH receptors. After this luteal cells can synthesize and secrete large amount of progesterone, that is protein hormone inhibiting FSH secretion.
The corpus luteum has a fixed life term during 14 days, since 15-th to 28-th days of menstrual cycle. There are following processes in corpus luteum: 1) vascularization 2) blossoming 3) involution — in case when pregnancy doesn't occur corpus luteum is called corpus luteum of menstruation. Regression of corpus luteum lasts for 2 months and is over with the formation of white body. If oocyte becomes fertilized and implants within the endometrium, the early pregnancy begins secreting human chorionic gonadotropin (hCG), which sustains the corpus luteum for the following 10-12 weeks.
Corpus luteum of pregnancy produces such hormone as relaxin which has tocolytic effect on the uterus.
I level — target organs (uterus, vagina and breasts).
Uterine cycle
The endometrial lining of the uterus undergoes dramatic histologic changes during the reproductive cycle. There are cyclic changes in the uterus as well as in the ovaries.
They are the most considerable in the functional layer of endometrium and are composed of such phases as desquamation, regeneration, proliferation and secretion.
Desquamation (mensis) lasts from the first to the second or fifth day of the reproductive cycle. During menstruation, the endometrium is sloughed out both with blood.
Functional layer of the endometrium is supplied with blood by spiral arteries. The spiral arteries extend from the arteries of the basal layer. Estrogen is a mitogenic hormone, which stimulates cell growth. With rising estradiol production during the follicular phase of the cycle, there is growth of the spiral arteries those extend into the surface of endometrium only at the end of the proliferative phase. There is an excessive growth of the spiral arteries in the secretory phase. They become most twisty and look
like tangles. The capillaries those are situated in the superficial layer of endometrium enlarge in their sizes and look like sinusoids. Spiral arteries of the functional layer contracts before the beginning of menstruation. It causes blood stasis, thrombosis, increasing vessel's permeability and their destroying. The necrosis and sloughing of the tissue occurs. It finishes on the third or fourth day of the menstrual cycle.
At the same time there is an inverse development of corpus luteum in ovaries, progesterone level decreases, hypothalamus produces foliberin and pituitary folitropin which stimulates the maturation of the new follicle in the ovary.
Regeneration phase takes place simultaneously with desquamation and is finally completed up to the 6-7th day of menstrual cycle. The thickness of the endometrium at this moment is 2-5 mm. There is maturing of follicle in the ovary at this time.
Proliferation phase lasts from the 7th to the 14th days of the cycle. The endometrium continues to thicken and the endometrial glands continue to elongate under the estrogens influence. The endometrium thickness is 20 mm, but its glands don't function. Endometrial glands are straight or somewhat twisted. There is a network of argyrophile fibers inside of the endometrial strome. At the final stage of proliferation the endometrial glands become tortuous and spiral arteries reach the surface of endometrium.
There is a completion of the follicle maturation in the ovary, the production of estrogens is peak on the 14th day until the end of proliferative phase. Pituitary stops the
FSH-secretion, hypothalamus starts production of luliberin which stimulates the production of LTH-in pituitary. As a result of this the level of luteonising hormone increases.
Secretion phase . After ovulation, the corpus luteum produces significant amounts of progesterone, which act on the endometrium to increase the size of endometrial glands and to promote the synthesis and secretion of proteins and other factors
(secretory endometrium) in preparation for pregnancy and implantation. This phase lasts from the 14th until the 28th day of cycle.
Glandular epithelium starts to produce the secretion containing glycopro-teids and glycogen. The signs of secretory transformation are revealed on the 15th-18th day. The
endometrial glands become tortuous and contain secretory material within the lumina.
There is maximum amount of the secretions on the 20th-21th day of cycle. Proteolytic and fibrinolytic activity at this time is the highest.On the 24-27th day of the cycle (late secretion) the endometrium is destroyed and degenerative changes occur in it.
Argyrofilic fibers destroy lacunar distension of cappillaries and focal hemorrhages into stroma occur. Endometrium is ready to desintegration and abruptio. Ovarian corpus luteum is well developed by this time. It produces progesterone, which is not a mitogen but causes differentiation of the tissues containing progesterone receptors. Progesterone converts the proliferate endometrium into a secretory one.
If fertilization and implantation don't occur, progesterone production rapidly diminishes, menstrual corpus luteum is destroyed, functional layer of endometrium is leading to desquamation. Initiating events lead to the beginning of the new cyclic changes in the ovaries and neuroendocrinous system in the whole female organism.
Some of the foreign authors have described three phases of reproductive cycle:
proliferation (5-14-th day of cycle) which is divided into early (5-7th day) and late proliferation
secretion — 15-28-th day
desquamation — 1-4-th day of the cycle
Cervical cycle
Uterine cervix is an important biological valve that controles the flow of biological substances into the uterine cavity and from it. Besides, it protects the uterine cavity from the infective agents' penetration. It provides menstrual blood outflow and excretion from the uterine cavity. Endocervix is covered by a simple columnar epithelium which contains secretory crypts. Secretory crypts produce cervical mucus. All uterine cervix structures are very sensitive to the steroid influence. Secretory cells of the endocervix constantly produce sticky transparent liquid, which is called cervical mucus. The quantity and composition of the mucus are regulated by the ovarian hormones secretion and they change during the reproductive cycle. In periovulation period the quantity of the mucus increases up to 600 mg per day, but in luteal phase the mucus quantity is only
50 mg per day.
Hydrated gel is the main component of the mucus that contains hydrocarbonates and glycoproteins. Such endocervical mucus characteristics as quantity, water contents and viscosity are maximal at the time of ovulation when the estradiol production is increased. All these changes create the most favourable conditions for fertilization.
Mucus flows down from the internal os to the external one. Epithelial cell microvilli oscillations direct the mucus flow into periphery of the endocervix. It favors the movement of active spermatocytes into the uterine cavity, which are able to overcome cervical mucus flow. Defective spermatocytes move away from the uterine cavity.
Prostaglandines and relaxin also can influence on the uterine cervix. These hormones promote dilation of the cervix in pre-ovulatory period.
Under the influence of estradiol, the endocervical glands secrete large quantity of thin transparent mucus. Pure watery endocervical mucus contains the increased number of mucin, glycoproteides, salts and decreased quantity of cellular elements. An external os of the cervical canal is more dilated in the ovulation; microfibrils of endocervix are situated parallely. The last one creates the microcanals which promote the migration of spermatocytes. Under the influence of progesterone in post-ovulatory period the cervical canal is closed, the quantity of mucus is decreased, microfrbriles are situated as network which is non permeable for spermatocytes.
Vaginal cycle
Estradiol stimulates vaginal thickening and maturation of the surface epithelial cells of the vaginal mucous in the follicular phase. Estradiol also facilitates vaginal transudation during the sexual excitement, creating a moist lubricated vagina for sexual intercourse. During the luteal phase of the cycle the vaginal epithelium stops its thickness but the secretory changes are diminished. The thickness of epithelium becomes twice less. In the result of this desquamation occurs. The superficial layer of vaginal epithelium is desquamated in this phase.
Cellular composition of vaginal contents is a biological test of sexual glands' hormonal activity. Superficial, intermediate, parabasal and basal cells ratio depends on the vaginal hormonal state. The quantity of superficial cells are correlated with the
estradiol saturation of organism. The more estradiol production results in more superficial cells. During the luteal phase of the cycle the quantity of intermediate cells predominates. Parabasal and basal cells appear during ovarian hypofunction and menopause. They are absent during the normal ovary function in the reproductive women.
Cyclic changes in uterine tubes
The fallopian tubes mucus has parallel folds, which are well developed in the ampulla and become smooth in the isthmus. Folds' height and their direction depend on the ovarian estrogen influence. They are high and parallel in the follicular phase of the cycle that makes sperms' and ovum' migration easier. The fold surface becomes complicated in the luteal phase that blocks the sperm movement.
Under the estrogenic influence the direction of uterine tubes cilia epithelium, fluid composition, contractile activity are changed. The last ones create favorable conditions for fertilization.
Breast cycle
The ductal elements in the breasts, nipples and areolae respond to estradiol secretion. After ovulation, progesterone stimulates the acinar (milk producing) glands.
Because the acinar glands are located in the tissue of breasts, it gives the breasts a more rounded configuration. Moreover, progesterone makes the venous pattern on the surface of the breasts and it appears more prominent and accentuates the small Montgomery glands contained within the areolae. These dynamic changes can be observed during the reproductive cycle.
BIOLOGICAL ACTION OF THE OVARIAN SEX STEROIDS AND
GONADOTROPINS
Estrogens
Estrogens are produced by the follicular internal membrane cells and in less quantity by the adrenal cortex. Estradiol, estron and estriol are the main estrogenic hormones. Estradiol is the most active. Estrogenic hormones are circulated in the blood in free state and binding together with proteins. The last one is biological inactive form.
Cholesterol that has been created from lipoproteids is the main structural
compound for all the steroid hormones. Steroid hormone secretion is stimulated by FSH and LH and by some enzyme systems, for example aromatases.
The quantity of estrogens predominates in blood plasma. Estrogens enter the liver, then they go into the intestine. Estrogenic hormones are destroyed in the liver and excreted with urine via kidneys. Uterus (endometrium and myometrium), vagina and breasts are target organs for this group of hormones.
The main biological effects of estrogenic hormones:
provoke the growing and development of uterus and breasts during puberty
stimulate hypertrophy and hyperplasia of myometrium during pregnancy
cause the proliferative phase of endometrium
uterine-placental blood circulation regulation, increase blood supply of uterus
stimulate vaginal mucus epithelial cells maturation and differentiation
myometrium sensibilizing to contractile drugs, thus increasing uterine tension, excitability and contractivity
increase uterine tubes peristalsis during ovulation that accelerates sperm migration
endocervical stimulation to mucus production, increase mucus plug permeability for sperm
nitrogen, sodium and fluid retention in the organism; calcium and phosphorus retention in the bones
decrease the level of blood cholesterol
reticuloendothelial system stimulation in physiologic quantities, phagocytes activity that respond for antibacterial immunity
Thus, in general, estrogenic hormones promote fertilization, interm onset and normal duration of labor. Menopausal estrogenic deficiency leads to the bone's calcium and phosphorus loss, increases quantity of cholesterol. These factors provoke bones' fractures and cardiac diseases. Estrogenic action into organism depends on the doses: small or average doses stimulate ovaries, follicullar development and maturation; large doses depress ovulation; too large doses lead to atrophic processes in the ovaries.
Gestagenic hormones
Gestagens (progesterone, oxyprogesterone, pregnenol) are secreted by luteal cells of corpus luteum and by luteal cells of follicle granulosa layer and their membranes.
Besides, adrenal cortex also produces estrogens.
Progesterone is the main gestagenic hormone.
Biological effects of gestagens:
promote secretion phase in the endometrium and decidual membrane creation during pregnancy
stop endometrial proliferation
decrease uterine excitability, acting via decreasing of myometrium sensitivity to contractile medicines
maintenance of uterine isthmus tension
muscle fibers hypertrophy stimulation during pregnancy
stimulation of acinar (milk producing) glands
desrease endocervical mucus production, lead to mucus plug unpermeability for sperm
decrease uterine tubes contractile activity
water and salts retention in the organism
stimulation of gastric juice secretion, depression of bile secretion
light hyperthermic effect at the hypothalamic level
high progesterone doses block pituitary secretion of FSH and LH. It stops follicle maturation and is the base in contraceptive action
Progesterone is called protective pregnancy hormone because it creates favourable conditions for fertilization, implantation and conceptus' development.
Androgens
They are produced in the adrenal glands, ovaries, and adipose tissue where there is extraglandular production of testosterone and androstenon. The last ones are the precursors for estrogen biosynthesis.
The main biological effects of androgens:
clitoris and labia majors growing stimulation
depression of milk production
drive female libido
exposure to excess androgens, through either excess production or increased action results in increased body hair and acne
accelerate protein synthesis, have anabolic action
accelerate bone's growing
stimulation of hemopoiesis
cause capillaries spasm (from this reason androgens are applicated in the treatment of fibromyomas with uterine bleeding)
in the small quantity they increase estrogenic influence in the uterus, and in large ones depress estrogenic influence on the uterus
Pituitary hormones
Anterior pituitary gland produces seven hormones, three of them are gonadotropin: folliculestimulating hormone, luteinizing hormone and prolactin. These hormones regulate sexual glands function. Ovary is a target organ for gonadotropin hormones.
FSH causes granulosa cells proliferation and follicle fluid secretion. LH causes ovulation and transformation of follicle into corpus luteum. Prolactin supports corpus luteum function, accelerates the process of breasts' growing and stimulates milk production in puerperium.
Posterior pituitary doesn't produce hormones. It stores two hormones — oxytocin and vasopressin which are produced by supraoptical and paraventricular nuclei of hypothalamus. They are excreted into the blood in certain doses.
Oxytocin provokes uterine contractions, increases intestinal peristalsis, and stimulates lactation. Vasopressin has antidiuretic effect, leads to arterial hypertension.
Both of these hormones increase glucose concentration in blood.
Hypothalamus
Hypothalamus is a nervous cell accumulation which produces special neurosecretion. It is stored in the anterior pituitary. Hypothalamic neurohormones,
which stimulate pituitary hormone excretion are called Liberins. Hypothalamic neurohormones which depress pituitary hormone excretion are called Statins. Fo-liberin stimulates FSH production by anterior pituitary, Lu-liberin stimulates prolactin production. Corresponding statins decrease the quantity of pituitary hormones regulating the reproductive cycle by feedback principle.
Epiphysis
Epiphysis is a gland which is situated in the midbrain over the cerebellum. Some biological active substances, such as melatonin, serotonin, norepinephrine are synthesized in the epiphysis cells.
Melatonin limits foli- and lutropin production in the hypophysis. On humoral level epiphysis is an organ that transforms light nervous impulses into biological substances production forming biological rhythms of organism (biological clock). It controls the onset of labor. As a rule, labor starts at night, in a dark period of time when melatonin production is very low. As a result of removing of the suppressive acting of epiphysis hormones into hypothalamus oxytocin production increases and labor starts.
Adrenal glands
The cortex of the glands produces such steroidal adrenal glands hormones as aldosterone, glucocorticoids, androgens, and small quantities of estrogens.
Glucocorticoids (Cortisol, cortisone, corticosterone) increase plasma concentration of glucose and liver concentration of glycogen, have catabolic effect (inhibit protein synthesis in connective tissue), increase human resistance to irritants, have antiinflammatory and desensitizing effects.
Mineralocorticoids (aldosterone) provoke sodium retention and potassium excretion from organism.
Catecholamines (adrenalin and norepinephrine) provoke two types of effects.
Rapid effect is a result of α-adrenergic action. It causes vessels narrowing, uterine contraction, smooth intestinal muscles and bladder relaxation. Slow effect causes cardiac muscle regulation, intestinal peristalsis depressing and vessels dilation.
Prostaglandins
Prostaglandins are a group of endogenous 20-carbon hydroxy-unsaturated fatty
acids, whose biosynthetic pathway begins with the precursor of arachidonic, linoleva and linolenove acids, thanks to the phospholipase A2. They are similar to hormones by their acting on organism, but they are secreted not in the endocrine glands, but in the different cells of organism, especially in the secretory endometrium. There are such structural groups of prostaglandins as A, E, F, D. Prostaglandin's action has both local and systemic effect. There are no prostaglandins reserves in organism, their life cycle is very short. Estrogens and oxytocin intensify prostaglandin' action, progesterone and prolactin have depressive action.
Main biological action of prostaglandins.
effect upon uterine contractile activity, these injections provoke interruptions of pregnancy in different term. They increase upper uterine segment tension and provoke cervical effacement
cause the ovum' movement in the fallopian tubes
prostaglandin associates uterine contractions, also aid the normal expulsion of endometrium and interm stop of bleeding
they produce uterine musculature and vascular contractions causing contractile and ischemic pain
take part in inflammatory reaction.
Besides, different types of prostaglandins very often have antagonistic action.
Thus, PE2:
decreases systemic arterial blood pressure. Improves blood oxygenation
dilates small vessels, makes better cerebral, liver and kidney's circulation
decreases pathological aggregation of erythrocytes
Prostaglandin PF 2α :
increases arterial blood pressure
decreases organs' blood supply, decreases blood oxygenation
potentiates thrombocytes aggregation
Contrandications to prostaglandins employment are bronchial asthma, glaucoma, thyrotoxicosis, ulcerative colitis, epilepsy, severe kidney and liver diseases
FEMALE DEVELOPMENT
Female life is divided into such periods as embryonic, childhood, puberty, sexual maturity, climacterium, menopause and aging.
Embryonic period lasts from the moment of fertilization until fetal birth. Fetal sex is determined during fertilization thanks to parental chromosomal number. Sexual organs are formed at the end of the first month of embryogenesis: ovary — from indifferent sexual gland; uterus, fallopian tubes and the upper part of vagina — from
Muller's ducts; lower part of vagina and external genitalia — from cloaca and urogenital sinus. Muller's ducts are twin embryonic formations which are situated out of sides from the spine of embryon. From each of them one half of uterus, vagina, and one fallopian tube is developed. Muller's ducts are drawing together and they are connected with each other in the process of development. If there are some deviations during this process, defects of sexual organs will develop.
Childhood begins from the girl birth and lasts until the age of 10-11. Anatomic difference between male and female organisms is present, functional difference is absent.
Puberty starts from 10-11 until 16 years old. It is characterized by the development of secondary sex characteristics such as breast development, pubic and axillary hair development, menarche.
Reproductive period starts from 18 until 45-47.
Climacterium begins in 45-47th year and lasts for 2-3 years. Physiologic climacterium does't have any abnormalities of female general state. The number of menarche and the quantity of blood loss are decreased, intervals between them become longer. Acyclic uterine bleeding and neurovascular characterizes pathological climacterium.
Menopause begins at the period of menarche stopping and lasts until the age of 70.
Aging starts after 70 years of age and lasts until the end of life.