Chapter 1 Introduction
advertisement

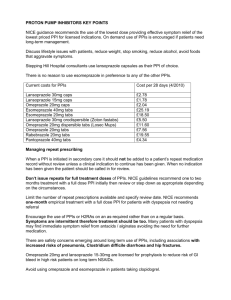
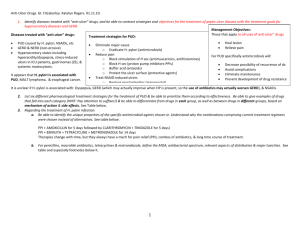
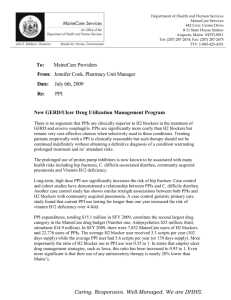
Chapter 1 Introduction CHAPTER-I INTRODUCTION 1.1. ACID-LABILE DRUGS Several acid-labile drugs from different chemical classes are currently on the market, demonstrating varying degrees of acid-lability. Due to their sensitivity to the acidic conditions, acid-labile compounds present many challenges during manufacturing and production and, therefore, should be dealt with appropriately. Some drugs are extremely acid-labile, including proton pump inhibitors (PPIs), penicillin G, didanosine (DDI), peptides and proteins. The therapeutic activity of such drugs can be compromised when exposed to acidic conditions; hence, they require suitable formulation technologies or structural modifications to remain stable and efficacious. Various structural moieties have been accounted for acid-lability of the drug molecules; however, there are at least two main recognized functional groups that may lead to this condition, namely, ester moiety and amide moiety in either aliphatic or cyclic forms. In the case of labile drugs, ester or amide moieties may undergo hydrolysis in the presence of acid which further yields an alcohol and a carboxylic acid or an amine and a carboxylic acid, for ester and amide groups, respectively. Table 1.1 outlines examples of commonly known acid-labile drugs. Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 1 Chapter 1 Introduction Table 1.1. Examples of commonly known acid-labile drugs (Volberding and Mitsuyasu, 1985; Gan et al., 1996; U.S. Patent No. 5,972,389, 1999; Morçöl et al, 2004; Physician’s Desk Reference (PDR), 2004) Drug Category Acid-labile moiety/Acid induced Examples reaction Antibiotics Lactam ring Penicillin G Carbenicillin Methicillin Peptides/Proteins Cyclic lactone Erythrmoycin Peptide bond Insulin Calcitonin Erythropoietin Interferons (IFN) Human recombinant Interleukin-2 Pancreatin (pancreatic enzymes) Immunoglobulins Nucleoside Cleavage of the glycosyl bond Didanosine Proton Pump Rearrangement to sulfenic acid Omeprazole Inhibitors and sulfenamide analogs Esomeprazole Lansoprazole Rabeprazole Pantoprazole Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 2 Chapter 1 Introduction It should be noted that the positioning of other groups such as methyl, methoxyl and others on the drug molecule and their spatial configurations may increase or decrease the acid sensitivity of the drug. Therefore, the molecular structure of the drug as a whole should be taken into consideration in this regard. For instance, Penicillin G has been recognized as an acid-labile drug due to the presence of a lactam ring (amide moiety) on its structure, and is available only as a parenteral formulation. However, Penicillin V is an acid-stable drug with a minor structural modification compared to Penicillin G and is available in oral dosage forms (Figure 1.1). Figure 1.1. The structural difference between acid- labile Penicillin G (A) and acid –stable Penicillin V (B) (Adapted from University of Michigan, 2004) On the other hand, for some drug molecules, esterification is a means to improve the stability and possibly bioavailability of the active ingredient. For instance, erythromycin as a free base, is very unstable in gastric acid, due to the presence of a cyclic ester (lactone) moiety in its structure while erythromycin propionate (a prodrug of erythromycin) demonstrates improved pharmaceutical Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 3 Chapter 1 Introduction properties (Figure 1.2). Another example is carbenicillin indanyl, where the ester improves the stability and lipophilicity of the drug. Figure 1.2. Chemical structures of Erythromycin as a free base (A) and a more stable erythromycin propionate (B) (Sigma Aldrich, 2004) There are several active ingredients that are decomposed in acidic conditions due to the presence of other structural features. Pantoprazole can serve as a representative example. Although Pantoprazole molecules rapidly degrade in an acidic medium, they demonstrate acceptable stability under alkaline conditions. Due to its severe instability in acidic environment and many formulation challenges, like proper enteric coating process, sensitivity to moisture and hence the stability of the formulation, its incompatibility with several excipients, Pantoprazole has been selected as a model acid-labile drug in the present research Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 4 Chapter 1 Introduction work. The application of Pantoprazole in therapeutics, the specifications of the drug molecule and the formulation strategies are investigated in the subsequent sections. 1.2. GASTROINTESTINAL CONDITIONS AND THERAPEUTIC VALUE OF PROTON PUMP INHIBITORS Peptic Ulcer Disease (PUD) and Gastroesophageal Reflux Disease (GERD) are common ailments, affecting the digestive system. PUD describes a heterogeneous group of disorders characterized by ulceration of the upper gastrointestinal tract (GIT), most commonly affecting the duodenum (duodenal ulcer) as compared to the stomach (gastric ulcer). Over 25 million Americans, an estimated 10% of the population, develop the disease in their lifetime. In the United States, there are approximately 500,000 new cases and 4 million recurrences of PUD annually (National Guideline Clearinghouse, 2004). Males and females are shown to be equally affected, although prevalence in older females appears to be higher. While the overall prevalence of PUD-associated mortality is decreasing, incidence remains high, particularly in .the elderly. Every year, an estimated 6,500 deaths in the United States are attributed to this condition (Shayne, 2004). Uncontrolled PUD may significantly decrease the life quality of the patient and lead to serious clinical consequences such as pain, ulceration and bleeding which may potentially result in anaemia, perforation of the GIT or haemorrhage (Soll, 1993). Disease- related costs to the health care system are also substantial. Annually in the U.S., the combination of PUD-associated direct and indirect costs exceeds 5.65 billion dollars (Garnett, 2000). PUD represents a disruption in the mucosal layer of the stomach or duodenum. As opposed to erosion, which is a superficial lesion, an ulcer has perceivable depth extending into the sub mucosa. PUD is thought to be the imbalance between the defensive factors that protect the mucosa and offensive or Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 5 Chapter 1 Introduction aggressive factors that disrupt this important barrier. Some mucosal protective factors include the water-insoluble mucous gel layer, presence of prostaglandins, local production of bicarbonate and adequate mucosal blood flow. Aggressive factors include the acid-pepsin environment, mucosal ischemia and most importantly, infection with Helicobacter pylori, a spiral- shaped Gram-negative bacillus, which is believed to be the leading cause of PUD (Marshall and Warren, 1984; Walsh and Peterson, 1995; Roll et al., 1997; Kethu and Moss, 2004). The term PUD is commonly used to refer to gastric and duodenal ulcers that are caused by acid-peptic injury although this type of ulcers can develop in any part of the gastrointestinal tract that is exposed to acid and pepsin in sufficient concentration and duration (Spechler, 2002). On the other hand, Gastroesophageal Reflux Disease (GERD) is a pathophysiologic phenomenon that can result in mild to severe symptoms. GERD can be described as any symptomatic clinical condition or change in tissue structure that results from the reflux of stomach or duodenal contents into the esophagus. Heartburn is the most common symptom of GERD. It may be accompanied by regurgitation of gastric contents into the mouth or the lungs. In patients with severe GERD dysphagia is common which may be a sign of a stricture formation in the esophagus. In some patients, pulmonary manifestations such as asthma, coughing or intermittent wheezing and vocal cord inflammation with hoarseness may occur (GERD Information Resource Center; Snape, 2000). Figure 1.3 shows the normal gastroesophageal anatomy and anatomy of stomach showing gastroesophageal reflux. Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 6 Chapter 1 Introduction (A) (B) Figure 1.3. Normal Gastroesophageal anatomy (A) and Anatomy of Stomach showing Gastroesophageal Reflux (B). Complications of GERD include esophageal erosion, esophageal ulcer and esophageal stricture. It is also speculated that GERD predisposes to Barrett’s Esophagus which may further develop into esophageal adenocarcinoma (El-Serag et al., 2004). The etiology of GERD can be attributed to such factors as transient relaxations of lower esophageal sphincter, delayed stomach emptying, ineffective esophageal clearance and diminished salivation. Other contributing factors include Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 7 Chapter 1 Introduction the potency of the refluxed material and the inability of the esophageal tissue to resist injury and repair itself. GERD afflicts millions of individuals in the U.S. An estimated 25-35% of the U.S. population is affected by this disease (Scott and Gelhot, 1999). Table 1.2 represents the frequency of common GERD symptoms in the general population. Table 1.2. The frequency of common GERD symptoms in the general population and their percentage of occurrence Symptoms Frequency Heart burn 70 – 85% Regurgitation 60% Dysphagia 15 – 20% Angina like pain 33% Bronchospasm 15 – 20% During the last three decades, the management of these disorders has been revolutionized by the introduction of histamine- 2 receptor antagonists (H2RAs) and proton pump inhibitors (PPIs). The PPIs are highly effective irreversible inhibitors of H+/K+ ATPase, the final step in gastric acid secretion. 1.2.1. Anatomy and Physiology of Stomach The main function of the stomach is to process and transport food. After feeding, the contractile activity of the stomach helps to mix, grind and gradually empty small portions of chyme into the small intestine, while the rest of the chyme is mixed and ground. From the anatomical perspective, the stomach can be divided into four major regions: fundus (the most proximal), body or corpus, antrum, and cardia. Histologically, the fundus and corpus are hardly separable. In the antral area, the density of the smooth muscle cells increases (Smout et al., 1980) Figure 1.4 represents the gross anatomy of the stomach. Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 8 Chapter 1 Introduction Figure 1.4. Gross Anatomy of the Stomach The stomach wall consists of three layers; mucosal (the innermost), muscularis (the middle) and serosal (the outermost). The mucosal layer itself can be divided into three layers: the mucosa (the epithelial lining of the gastric cavity), the muscularis mucosa (low density smooth muscle cells) and the submucosal layer (consisting of connective tissue interlaced with plexi of the enteric nervous system) (Gray, 1985). Functionally, the stomach can be divided into two areas, the oxyntic glands and pyloric glands. Oxyntic glands are located in the gastric fundus and corpus and are composed of several cell types, including parietal cells which secrete hydrochloric acid, ‘HC1’ and intrinsic factor, chief cells which secrete pepsinogen, D cells which generate somatostatin, mast-cell (MC) and enterochromaffin-like (ECL) cells which secrete histamine and mucus-secreting cells. The pyloric glands are located in the antrum and contain mucus-secreting cells, D cells and G cells which synthesize and secrete gastrin. Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 9 Chapter 1 Introduction 1.2.2. Physiology of acid secretion The secretion of acid is regulated by parietal cell. These cells generate protons (H which are secreted into the lumen by a cellular H ATPase (the proton pump) that constitutes the final common pathway of gastric acid secretion. Three main stimuli act on the parietal cell, namely, gastrin (a hormone), acetylcholine (a neurotransmitter) and histamine (a local hormone). On the other hand, prostaglandins E2 and I2 play an inhibitory role on acid secretion. Figure 1.5 represents acid secretion in the parietal cell. Hydrochloric acid (HCl) is secreted into the lumen of the stomach by parietal cells in the glands of the oxyntic mucosa. Gastric H+,K+-ATPase is fundamental to this process of acid secretion. This enzyme, located in the apical membrane of the parietal cell, transports H+ into the parietal cell canaliculus in exchange for K+. The secretion of H+ is accompanied by the passage of clacross, the apical membrane into the canaliculus, which ensures that acid secretion is electroneutral. In the resting parietal cell the H+,K+-ATPase is inactive and present largely in tubulo-vesicles in the cytoplasm of the cell. Stimulation of the parietal cell occurs with the involvement of the acetylcholine (M3), gastrin (CCK2) and/or histamine (H2) receptors on the baso lateral membrane via secondary messengers. This causes movement of H+,K+-ATPase to the apical membrane of the cell where it can exchange H+ for K+. Chloride ions enter the secretory canaliculi from the cytoplasm by a passive transport mechanism, resulting in the secretion of HCl. Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 10 Chapter 1 Introduction Figure 1.5. Schematic representation of acid secretion in the parietal cell The exact mechanism of action of these three secretagogues on the parietal cell is not fully known. There are two main hypotheses, single-cell and two-cell. According to the single-cell theory, the parietal cell possesses H2 receptor, muscarinic receptor and gastrin receptor for histamine, acetylcholine and gastrin respectively. Stimulation of H2 receptor increases cyclic adenosine monophosphate (cAMP), while stimulation of the muscarinic and gastrin receptors increases cytosolic calcium. The synergistic effect of these intracellular messengers generates acid secretion, when they all act directly on the parietal cell. According to the two-cell hypothesis, gastrin and acetylcholine act either only by releasing histamine or partly by releasing histamine and partly by direct action on their specific receptors on the parietal cell (Rang et al., 1995). Acid secretion in response to a meal can be divided into three phases: cephalic, gastric, and intestinal. The cephalic phase is mediated by the vagus nerve in response to the sight, smell, or thought of food and accounts for 30% to 35% of the total acid output in response to a meal. Basal and nocturnal acid Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 11 Chapter 1 Introduction secretion is also mediated by the vagus nerve; thus, both the cephalic phase of a meal and the basal circadian rhythm of acid secretion can be abolished by vagotomy. The gastric phase of acid secretion accounts for 50% to 60% of total meal-stimulated acid release and more than 90% of this phase is mediated by gastrin release from the G cells. Gastrin release is mediated by two principal components of the ingested meal: protein content and pH. Gastrin is secreted when the luminal pH increases above 3.5 and diminishes at a pH of less than 1.5. The intestinal phase of acid secretion plays only a minor role, accounting for less than 5% of the acid response to a meal, and appears to result from the effects of absorbed amino acids. A negative feedback loop governs the means by which both gastrin release and acid secretion return to basal levels. This process represents a vital auto regulatory mechanism for preventing postprandial acid hypersecretion. After ingestion of a meal, gastrin release stimulates the secretion of gastric acid. The pH of the lumen begins to decrease as the buffering capacity of the meal is overwhelmed by continued acid secretion. The increasing acidity appears to stimulate the release of somatostatin from the D cells. Somatostatin, in turn, inhibits the further release of gastrin from G cells and acid secretion is subsequently diminished. D cells may also directly inhibit acid secretion from parietal cells or may suppress histamine release from ECL cells (Spechler, 2002). 1.2.3. Acid Secretion and the Role of the Proton Pump As cited earlier, proton pump is the final step in the mechanism of gastric acid secretion. When gastric acid secretion is stimulated, there is a morphologic transformation of the membrane of the parietal cell (Helander, 1984). Tubulovesicular membranes, which are prominent in the cytoplasm of the resting cell, diminish in accordance with a 6-10 fold increase in an apical canalicular membrane and the appearance of long apical microvilli. The tubulovesicular Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 12 Chapter 1 Introduction membranes appear to fuse with the apical plasma membrane. There is evidence that H+/K+ ATPase (the proton pump) as well as potassium and chloride ion transporters are translocated from the tubulovesicles to the secretory canaliculus just before initiation of H+ secretion (Hersey and Sachs, 1995). The proton pumps of parietal cells secrete protons, or more likely, hydronium ions (H3O+) (Munson et al., 2000). Chloride ions accompanying hydrogen ions are secreted against both a parietal cell-to-lumen concentration gradient and an electrical gradient. Thus, HC1 secretion by parietal cells is an active energy-dependent process. Parietal cells contain abundant mitochondria to accomplish the active proton transport. Adenosine triphosphate (ATP) provides the energy required for the active pumping of protons by the H+/K+ ATPase (Munson et al, 2000). This enzyme is magnesium-dependent and is found on the secretory membranes of the parietal cells. The sequential phosphorylation and dephosphorylation of the proton pump results in H+ secretion in exchange for recycled K+. Figure 1.6 represents gastric acid secretion by the parietal cell. Acid is produced within the parietal cell from the dissociation of water. The hydroxyl ions formed in this process rapidly combine with carbon dioxide to form bicarbonate ion, a reaction catalyzed by carbonic anhydrase. Bicarbonate ions are then transported out of the basolateral membrane of the parietal cell in exchange for chloride ions. The rapid entry of bicarbonate ions into blood results in a slight elevation of blood pH known as the ‘alkaline tide’. This process serves to maintain intracellular pH of about 7.4 in the parietal cell (Schreiber et al, 2000). Chloride and potassium ions are transported into the lumen of the canaliculus of the stimulated cell via conductance channels. Hydrogen ion is pumped out of the cell, into the lumen, in exchange for potassium through the action of the proton Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 13 Chapter 1 Introduction pump; thus, potassium is effectively recycled. Accumulation of osmotically-active hydrogen ion in the canaliculus generates an osmotic gradient across the membrane which leads to outward diffusion of water. The resulting gastric juice contains about 150 mM HC1, 15 mM KC1 and a small amount of NaC1 (Spechler, 2002). Figure 1.6. Pictorial presentation of gastric acid secretion by the parietal cell 1.2.4. Targeting acid secretion by blocking gastric H+, K+-ATPase Proton pump inhibitors (PPIs), which inhibit the H+,K+-ATPase, are a more effective class of agents than H2RAs, providing superior symptom relief and achieving higher healing rates in GERD. Despite the undoubted efficacy of PPIs, several areas have been suggested where treatment could be further refined or enhanced (e.g., faster and better symptom control and more rapid healing). Rather than targeting the receptors involved in acid production, PPIs inhibit the final step in the process. They achieve this by covalently binding to the H+,K+-ATPase enzyme. After absorption, PPIs have a relatively short plasma half-life of 90–120 minutes, during which time they accumulate in the acid space Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 14 Chapter 1 Introduction of the actively secreting parietal cell. Figure 1.7 represents the mechanism of action of PPIs. Here they are transformed into the active sulfenamide, which forms covalent (and therefore irreversible) disulfide bonds with key cysteine residues of the H+,K+-ATPase (Besancon et al, 1993; Besancon et al, 1997). This mechanism of action results in the unique pharmacokinetic– pharmacodynamic effect pattern of PPIs. The inhibitory effect on acid secretion is related to the amount of sulfenamide formed, which for a given dose is related to the AUC (area under the plasma concentration time curve) and there is no direct correlation between blood plasma concentration and effect at any given time. The duration of effect is determined by the half-life of the sulfenamide-enzyme complex (at least 24 hours), rather than by the half-life of the PPI in blood plasma. Therefore therapeutic oral doses of PPIs have a slow, cumulative onset of effect and achieve maximal effect levels only after 4–5 days of daily dosing. Figure 1.7. Mechanism of action of PPIs: conversion to sulphenamide and covalent binding to the H+,K+-ATPase Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 15 Chapter 1 Introduction 1.2.5. Historical Approach in Diagnosis and Treatment of Peptic Ulcer Disease (PUD) From the literature, it appears that PUD had been a rare disorder before the 19th century (Jennings, 1940). Early in that century, cases of perforated peptic ulcerations of the stomach were first described in young women. Over the following decades, PUD became more frequent in men and by the end of the 19th century; duodenal ulcer disease had surpassed gastric ulcer in frequency. The incidence of peptic ulceration rose dramatically through the first half of the 20th century. In the early 20th century, stress and diet were judged to be the important pathogenic factors for PUD. Consequently, patients with peptic ulcers were treated with hospitalization, bed rest and bland diets. By the 1950s, investigators focused their attention primarily on the pathogenic role of gastric acid; therefore, antacid therapy had become the treatment of choice for PUD. When H2 receptor antagonists became available for clinical use in the 1970s, antisecretory therapy for acid suppression rapidly emerged as the treatment of choice. With the advent of proton pump inhibitors (PPIs) in the l980s, even more potent acid suppression and consequently higher rates of ulcer healing could be achieved. Although numerous investigations showed that most acute peptic ulcerations healed with acid suppression therapy, most patients experienced recurrences within one year of discontinuing treatment with antacids or antisecretory agents alone (Graham et al., 1992). During the 1980s, it was reported that most peptic ulcerations were associated either with gastric infection by Helicobacterpylori (H. pylori), or with the ingestion of nonsteroidal anti-inflammatory drugs (NSAIDs) (Marshall, 1994). Furthermore, numerous studies revealed that if H. pylori infection and the use of NSAIDs could be eliminated, then peptic ulceration recurred infrequently. These observations revolutionized the therapeutic approach to peptic ulcer disease and the search for these causes of peptic ulceration has become a key component of Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 16 Chapter 1 Introduction modern patient management. Nevertheless, there still remains a minority of patients who are afflicted with PUD with no apparent predisposing factor (Kurata and Nogawa, 1997). At present, H. pylori and NSAIDs are still believed to be the two major contributing factors in the occurrence of PUD, with H. pylori to be the dominant cause (Howden, 1997; Levine, 2000). Approximately about 60 - 90%, of the patients with gastric ulcers and about 90% of the patients diagnosed with duodenal ulcers have been infected with H. pylori (Balaban and Peura, 1997; Levine, 2000). Figure 1.8 illustrates conditions associated with duodenal and gastric ulcers. In addition to H. pylori infection or NSAID ingestion, in some occasions, PUD may result from hypersecretory conditions, the disorders that cause the stomach to secrete large quantities of gastric acid which overwhelms the normal defence mechanisms. In addition to causing peptic ulceration, the excessive amounts of gastric acid which enters the duodenum in the hypersecretory conditions can denature pancreatic digestive enzymes and cause mal absorption and diarrhoea. Zollinger-Ellison syndrome (ZES) is an example of such conditions. In ZES, one or more neuroendocrine tumors, commonly referred to as gastrinomas, form in the pancreas or duodenum and secrete large amount of the hormone gastrin which further causes hypersecretion of gastric acid (Spechler, 2002). Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 17 Chapter 1 Introduction Figure 1.8. Pie charts illustrating conditions associated with duodenal and gastric ulcers Various risk factors such as dietary, genetic, pharmacologic and psychologic may also contribute to the occurrence of PUD and its complications (Gore, 2000; Ryan Harshman and Aldoori, 2004), for instance, smoking and alcohol, emotional stress and genetic factors. It has also been reported that a number of drugs, other than NSAIDs, appear to predispose to peptic injury, for example, 5-fluorouracil (Shike et al., 1986), potassium chloride pills (Sherman and Bini, 1999), crack cocaine (Feliciano et al., 1999), and alendronate (Graham and Malàty, 1999; Lowe et al., 2000). 1.2.6. Current Treatment of Ulcer Disease The objective of treatment for PUD has been defined as healing the ulcer, alleviating the symptoms and prevention of ulcer recurrence, hence, improving the quality of life (Howden, 1997). The treatment plan is based on the etiology of PUD. If H. pylori infection is present, patients should be treated with a regimen containing specific antibiotics, irrespective of whether there is a history of NSAID use. It is recommended that, if possible, NSAID therapy be discontinued. Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 18 Chapter 1 Introduction Specific non-anti-infective therapies for PUD include antacids, H antagonists, sucralfate, bismuth, prostaglandin analogs, anticholinergics, proton pump inhibitors (PPIs) and, if necessary, surgical operations (Horn, 2000; Spechler, 2002; Der, 2003). PPIs are the focus of the present study and will be discussed in details. 1.2.7. Overview of Proton Pump Inhibitors (PPIs) Proton pump inhibitors (PPIs) were introduced in the United States in the late 1980s and have emerged as the treatment of choice for most acid-related disorders, including PUD, GERD and its complications such as erosive esophagitis (EE) and Barrett’s esophagus (BE), Zollinger-Ellison syndrome (ZES) and idiopathic hypersecretion. PPIs are also effectively used for the treatment of H. pylori infection and upper gastrointestinal bleeding (Horn, 2000; Spechler, 2002; Der, 2003). Table-1.3 gives the solid oral dosage forms of PPIs available on the U.S. market. The first indication of substituted benzimidazoles with gastric acid secretion inhibiting effect is encountered in US Patent No. 4,045,563 which discloses substituted 2- (Berntsson et al., 1977) and EP Patent No. 0005129 that describes omeprazole, 5-methoxy-2(((4-methoxy-3,5-dimethyl-2-pyridinyl) methyl) sulfinyl)-1H-benzimidazole, as a potent inhibitor of gastric acid secretion (Sjostrand and Junggren, 1979). Omeprazole was the first PPI on the market, launched in 1989. Lansoprazole was the second PPI, followed by rabeprazole, pantoprazole, and esomeprazole (Der, 2003). Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 19 Chapter 1 Introduction Table 1.3. Solid oral dosage forms of PPIs available on the U.S. market PPI Proprietary Manufacturer Solid Strength FDA name in the Dosage (mg) Approval U.S. Form* Year Omeprazole Prilosec® Astrazeneca Capsule 10, 20, 40 1989 Omeprazole Prilosec Astrazeneca Tablet 20 2003 magnesium OTCTM Lansoprazole Prevacid® TAP Capsule 15, 30 1995 Tablet 20 1999 Pharmaceuticals Inc. Rabeprazole Aciphex® sodium Janssen Pharmaceutica Pantoprazole Protonix® Wyeth-Ayerst Tablet 20, 40 2000 Nexium® Astrazeneca Capsule 20, 40 2001 sodium Esomeprazole magnesium * Available solid dosage forms are either enteric-coated tablets, or capsules containing enteric-coated pellets All members of the PPI family are substituted 2-pyridyl methyl-sulfinyl benzimidazoles, sharing a similar core structure (Horn, 2000; PDR 2004). Table 1.4 gives the chemical structures of the proton pump inhibitors. Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 20 Chapter 1 Introduction Table 1.4. Chemical structures of the proton pump inhibitors PPIs are lipophilic weak bases, with a pKa of approximately 4.0 for omeprazole, esomeprazole, lansoprazole, pantoprazole, and a pKa of about 5.0 for rabeprazole. Thus, they can selectively accumulate in the acidic environment with a pH of less than 4, which is primarily found in the secretory canaliculus of the gastric parietal cell. At neutral pH, PPIs are chemically stable and are devoid of the antisecretory activity, hence, are referred to as prodrugs. However, these agents are acid-labile; in acidic conditions they become protonated and rearrange to form a tetracyclic sulfenamide which represents the active form of the drug (Brunton, 1996). It then binds to the exposed cysteine residues in the alpha subunit of H+/K+ ATPase to form covalent disulfide bonds, which irreversibly inhibit the activity of the proton pump. Cysteine at position 813 is a common binding site for all PPIs; however, pantoprazole also interacts with cysteine 822. PPIs possess an extraordinary selectivity. The lumen of the canaliculus of the parietal cell has a representative pH of less than 1.0 which is highly acidic compared to any other space within the body. At these acidic pH levels, the acidcatalyzed transformation of PPIs takes place in fractions of seconds, hence Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 21 Chapter 1 Introduction increasing the accumulation of these drugs. Also, the other members of the gastric ATPase lack the cysteines that are the target of the PPIs (Sachs, 2003). Since PPIs bind covalently, the duration of acid inhibition is long (over 24 hours) although the plasma half-life of these agents is short (about 1-2 hours) (Cederberg et al., 1985). Gastric acid secretion is restored by translocation of new pumps to the secretory canaliculus membrane. Although all PPIs share the same mode of action, they may differ in their clinical pharmacology. Rabeprazole, for instance, has been reported to be a more rapid and potent inhibitor of H+/K+ ATPase compared to the other PPIs, possibly due to its faster activation in the parietal cell canaliculus (Besancon et al., 1997). Owing to their specific inhibitory action of the proton pump, PPIs, therefore, offer a unique and highly selective means of controlling gastric acid production (Larsson et al., 1985). It has been reported that PPIs demonstrate antibacterial activity against H. pylori in-vitro and may also exert an anti-inflammatory effect by interfering with the cellular immune response to the infection. Their antimicrobial activity is selective for H. pylori; however, different PPIs may demonstrate varying levels of effectiveness against the microorganism. The mechanisms that account for the antibacterial effects of PPIs may depend on several parameters including, (1) structural similarity of PPIs to the antibiotics which are active against H. pylori, (2) inhibition of bacterial urease exerted by PPIs, or (3) the possible interaction of PPIs with bacterial ATPases that regulate the transmembrane ion flux (Hirai et al., 1995; Dattilo and Figura, 1998; Nahao and Malfertheiner, 1998; Horn, 2000). In order to increase the eradication rates of H. pylori, co-administration of antibiotics and bismuth salt with a PPI appears to have a synergistic effect. Recommended Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 22 Chapter 1 Introduction antibiotics include, but not limited to, metronidazole, tetracycline, clarithromycin and amoxicillin (Horn, 2000). PPIs have demonstrated superiority over the other anti-ulcer agents, due to their fewer side effects and drug interactions and offering the convenience of less frequent administration (Carao et al., 2001; Kawano et al., 2002). As for pharmacokinetic considerations of PPIs, it has been reported that these agents are well absorbed after oral dosing. Although food may delay the absorption of PPIs, (Andersson, 1996) this delay does not alter the clinical efficacy of these agents (Lew, 1999). Absorption of the enteric-coated agents, especially tablets, may be erratic and peak plasma concentrations are generally not achieved until 2-5 hours after the oral administration. The bioavailability of omeprazole appears to increase with multiple dosing, rising from 35% for the first dose to 60% after repeated dosing (Cederberg et al., 1989; Andersson et al., 1990). This phenomenon may be due to the antisecretory effects of the early doses which may lead to decreased degradation of the acid-labile omeprazole in the stomach or duodenum. In addition, hepatic enzymes may become saturated with omeprazole, thus decreasing the first-pass metabolism of the subsequent doses (Clissold and Campoli-Richards, 1986). On the other hand, the bioavailability of rabeprazole does not appear to change appreciably with multiple dosing which can further result in a greater antisecretory effect for this drug during the first day of therapy, although the clinical importance of this phenomenon in the treatment of peptic ulcer disease has been shown to be minimal (Yasuda et al., 1994). PPIs are extensively bound to the plasma proteins (more than 95%) (Brunton, 1996). This process inactivates some of the drug in the bloodstream and Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 23 Chapter 1 Introduction carries it throughout the body; only the unbound drugs can act on target tissues (Der, 2003). PPIs are metabolized in the liver by the cytochrome P450 enzyme system (specifically CYP2C19) and the inactive products of this metabolism are mainly excreted in the urine (Cederberg et al., 1989; Petersen, 1995; Pichard et al., 1995). It has been shown that omeprazole has a complex metabolic fate in the human body which involves excretion of at least 50 metabolites (Weidolf and Castagnoli, 2001). The metabolites among others, include omeprazole sulfone, 5.hydroxymethylomeprazole and 5-carboxyomeprazole. Liver failure can delay PPI clearance, but clearance is not significantly affected by renal insufficiency since the metabolites excreted in the urine are not active (Hoyumpa et al, 1999). With mild to moderate liver impairment, PPI dose adjustments generally are not necessary because of the wide safety margins of these agents. In the case of severe hepatic failure, the PPI should be reduced to the lowest dose possible or the interval should be extended to every other day. As a result of their requirement for concentration and activation in an acidic environment, PPIs bind predominantly to the proton pumps that are actively secreting acid. Thus, the efficacy of the PPIs for inhibiting acid secretion is limited if they are administered during the fasting state, when only about 5% of the stomach’s proton pumps are active. In contrast, in the fed state, 60% to 70% of the proton pumps actively secrete acid. Thus, PPIs are most effective if they are administered immediately before meals. If given in this manner, the PPIs are remarkably effective inhibitors of gastric acid secretion. After one week of conventional-dose therapy, the PPIs inhibit basal and gastrin-stimulated acid secretion by more than 98% (Sachs et al., 1990). Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 24 Chapter 1 Introduction When using PPIs in the once-daily dose regimens, healing rates for duodenal ulcer of 80% to 100% can be achieved after 4 to 8 weeks of therapy. Healing rates for gastric ulcer at 4 to 8 weeks appear to be somewhat lower, in the range of 70% to 85%. No single PPI has been shown to be clearly superior to the others in healing efficacy (Dekkers et al., 1999; Holt and Howden, 1991). PPIs are remarkably safe and well-tolerated. The occurrence of serious side effects with PPI therapy is rare. The most frequently reported side effects are headache and diarrhea (Clissold and Campoli-Richards, 1986; Solvell, 1990). The elevation of gastric pH induced by the PPIs can affect the absorption of a number of medications. For instance, ketoconazole requires stomach acid for absorption, and this drug may not be absorbed effectively after administration of PPIs. Also, since PPIs are metabolized by the cytochrome P450 system, they may interfere with the metabolism of other drugs that are eliminated by the same enzyme. Among the PPIs, omeprazole appears to have the greatest potential for such drug interactions and it has been shown to delay the clearance of warfarin, diazepam and phenytoin; however, clinically important drug interactions are uncommon (Humphries and Merritt, 1999). It has been reported that most pharmacokinetic and pharmacodynamic variations among the PPIs do not result in clinically significant differences between patients. The choice to select one PPI over another is most likely based on acquisition cost, differences in formulation, labeled indications and interaction potential. Overall, PPIs are all well- tolerated and portray a good safety record (Spechler, 2002). 1.2.8. Pharmacokinetics of Proton Pump Inhibitors (PPIs) Although PPIs are highly effective in acid suppression, there are differences in pharmacokinetics, such as bioavailability, elimination, half-life and Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 25 Chapter 1 Introduction metabolism between individual PPIs and these differences may translate into differences in clinical outcomes. The pharmacokinetics of currently available PPIs, based on information available from the product monographs are summarised and shown in Table 1.5. The absolute bioavailability ranges from 35% for a single dose of omeprazole to 89% with repeat administration of esomeprazole. Unlike other PPIs, the bioavailability of rabeprazole remains unchanged with repeat dosing. On the whole, the time to reach the peak plasma concentration (tmax) is about 2 hours. After absorption into the circulation, PPIs are taken up preferentially by gastric parietal cells, especially when they are actively secreting acid. Table 1.5. Pharmacokinetics of Delayed Release PPIs Parameters Esomeprazole Lansoprazole Omeprazole Pantoprazole 40 77 Absolute bioavailability 64-90 >80 (%) Time to peak plasma level 1.5 1.7 0.5-3.5 2-4 1.0-1.5 1.5 0.5-1.0 1.0 97 97 95 98 Yes Yes Yes Yes (h) Plasma halflife (h) Plasma protein binding (%) Hepatic metabolism Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 26 Chapter 1 Introduction 1.2.9. Delayed-release enteric-coated PPIs Acid labile drugs such as the proton pump inhibitors tend to be unstable at acidic pH and therefore have to be formulated as enteric-coated dosage forms to prevent acid degradation. The coating protects the active ingredient from degradation by gastric acid, but it also delays absorption, so that the peak plasma concentration (Cmax) is not typically attained for up to five hours after oral administration of these formulations. Although these drugs are stable at alkaline pH, they are destroyed rapidly as pH falls (for example, in the presence of gastric acid). Or, if the enteric-coating of the composition is disrupted by chewing resulting in degradation of the active ingredient by the gastric acid in the stomach. Upon ingestion, an acid-labile pharmaceutical compound must be protected from contact with acidic stomach secretions to maintain its pharmaceutical activity. Certain acid labile drug compositions with enteric-coating have been designed to dissolve at basic or near neutral pH to ensure that the drug is released in the proximal region of the small intestine (duodenum), not in the stomach. However, due to their pH-dependent attributes and the uncertainty of gastric retention time, in-vivo performances as well as inter and intra subject variability are very high; making it an uncertain method. Nevertheless at basic/near neutral pH, most acidlabile pharmaceutical agents are still susceptible to degradation depending on the particular pKa of the agent. Further as an acid-labile compound upon ingestion must be transferred in intact form, i.e., a non-acid degraded or reacted form, to the duodenum where the pH is near or above its pKa, the enteric-coating must be resistant to dissolution and disintegration in the stomach, that is, be impermeable to gastric fluids while residing in the stomach. Additionally, since the therapeutic onset of an enteric-coated dosage form is largely dependent upon gastric emptying time, it varies between subjects. In most subjects, gastric emptying generally varies from about 30 minutes to several hours after ingestion. Thus, for a period of time following ingestion, an enteric-coated dosage form resides in the low pH Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 27 Chapter 1 Introduction environment of the stomach before moving into the duodenum. During this time, the enteric-coating may begin to dissolve or imperfections or cracks in the coating may develop, allowing gastric acid to penetrate the coating and prematurely release drug into the stomach rather than in the small intestine. In the absence of buffering agent, an acid-labile drug that is exposed to this gastric acid is rapidly degraded and rendered therapeutically ineffective (Paul, 2000). To overcome the disadvantages of gastric emptying time; enteric-coated dosage forms are generally taken on an empty stomach with a glass of water. This minimizes exposure time to gastric fluid, as it ensure gastric emptying within about 30 minutes or so and delivery of the dosage form from the stomach to the duodenum. Once in the duodenum, optimal conditions exist for the enteric-coating to dissolve and release the drug into the bloodstream where absorption of a nonacid degraded drug occurs. If food is ingested contemporaneously with the administration of an enteric-coated dosage form, gastric emptying may not only be slowed, but there is also an increase in the pH of the stomach from about pH 1 to about 5 over the next several hours, depending on, for example, the general health of the subject and the composition being administered (Charman et al., 1997). When the pH begins to approach 5, the enteric-coating begins to dissolve away resulting in premature release of the drug into the stomach. In geriatric patients the gastric pH is already elevated as there is a general decline in gastric acid secretion in the stomach with aging. In such patients; enteric coated acid labile drugs are less effective (Barry E Gidal, 2006). Also, when the ingested food contains any fat, gastric emptying can be delayed for up to 3 to 6 hours or more, as fat in any form combined with bile and pancreatic fluids strongly inhibits gastric emptying. As a general rule, enteric-coated dosage forms should only be ingested on an empty stomach with a glass of water to provide optimal conditions for dissolution and absorption. Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 28 Chapter 1 Introduction Currently available delayed-release proton-pump inhibitors (PPIs) are orally administered as enteric-coated preparations. Different formulations have been developed. Omeprazole (OME), Lansoprazole and Esomeprazole are generally administered as gelatin capsules containing enteric-coated granules, whereas Pantoprazole and Rabeprazole are given as enteric-coated tablets. The different enteric coatings, which are necessary to protect the acid-labile PPI from acid degradation within the stomach, have the potential disadvantage of delaying PPI absorption. The PPIs employing any form of enteric coating for oral administration can be considered to be delayed release (DR) preparations, as the enteric coating reduces the rate of absorption of the PPI into the systemic circulation. In its standard DR formulation, the proto-typical PPI OME has poor absorption after a single dose and displays marked inter individual variability in the parameters of maximum plasma concentration (Cmax), time to achieve Cmax (tmax) and area under the plasma concentration/time curve (AUC) (Howden et al., 1984; Howden et al., 1985). Although the delayed release PPIs have had an enormous impact on the management of gastro-esophageal reflux disease (GERD) and other acid-related disorders, they do not achieve maximum effectiveness after a single dose. This may be due in part to their poor absorption with initial dosing. A recent systematic review of the effectiveness of PPIs in relieving symptoms of GERD, found that most patients did not obtain complete relief of daytime or night-time symptoms with the first dose (McQuaid and Laine , 2005). Lack of a prompt response of GERD to PPI therapy may contribute to patient dissatisfaction with treatment and may lead to unnecessary increases in dose or inappropriate switching to alternate members of the class. Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 29 Chapter 1 Introduction Limitations to enteric-coated PPI formulations also include the potential for nocturnal acid breakthrough (NAB), defined as an intragastric pH below 4 for at least one hour during the night with PPI therapy. Despite adequate therapeutic dosing (including twice-daily administration), patients taking enteric coated, delayed-release PPIs may experience nocturnal gastric acidity. Whether or not the agent is taken before breakfast, before dinner or twice daily, the patients may still have night time symptoms of heartburn (Katz et al., 1998; Peghini et al., 1998; Ours et al., 2003). 1.2.10. Addressing unmet needs in PPI therapy Although these agents form the therapeutic cornerstone of management for a variety of acid-related disorders, there is still room for improvement in our armamentarium. There would, therefore, be some clinical utility of a formulation that ensured rapid absorption of the PPI and a more rapid onset of antisecretory activity. To overcome the problems of enteric coating; specifically, an acidsuppressing agent that shows more rapid absorption; that can be administered orally, that provides better nocturnal acid control; that shows greater dosing flexibility, that reduces inter individual variability, that shows maintained tolerability and safety and that sustains gastric pH above a critical threshold would be a welcome addition to the PPI class (Ralph E Small, 2005). 1.2.11. The advent of Immediate release formulations of PPI Approximately in 2004, the U.S. Food and Drug Administration (FDA) approved a unique IR formulation of omeprazole (Zegerid®) to treat a variety of acid-related disorders and to reduce the risk of upper gastrointestinal bleeding in critically ill patients. Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 30 Chapter 1 Introduction Scientists have developed the concept of immediate release of the proton pump inhibitor with compositions comprising large amounts of buffers, to prevent the degradation of acid labile drugs (Jeffrey owen Philips and Ashland MO, 2002). The potential advantage of this formulation is a more rapid absorption of the PPI compared to delayed-release formulations. More rapid absorption has been associated with more rapid onset of suppression of gastric acidity compared with delayed-release formulations (Howden, 2005). This compound was developed by combining a highly effective PPI (omeprazole) with an antacid buffer (sodium bicarbonate), which neutralizes gastric acid and protects the PPI from gastric acid degradation. Studies have found that the degradation half-life of non–enteric-coated omeprazole is approximately seven hours at a pH of 6, compared to less than three minutes at a pH of 1.2 (Kromer et al, 1998). In an in-vitro model, the sodium bicarbonate buffer in IROME rapidly increases the pH to greater than 6 within one minute and sustains this pH environment for approximately 30 minutes (Santarus, Inc. Data on file, 2004). This pharmacological synergy protects omeprazole from gastric acid degradation, allows it to be rapidly absorbed and eliminates the need for an enteric coating. 1.2.12. Mechanism of action of Immediate release PPI The absorption of OME and the onset of its antisecretory effect are more rapid when administered as IR-OME than as DR-OME. The putative mechanism of action to explain these observations is as follows. Following ingestion of IROME as an oral suspension, the sodium bicarbonate causes a prompt rise in intragastric pH. While this serves the primary function of protecting the uncoated OME from acid degradation within the stomach, it may also provide a temporary stimulus to gastrin release from antral G cells. Sodium bicarbonate solution has previously been shown to raise circulating gastrin levels within 30 min of oral Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 31 Chapter 1 Introduction ingestion. The rise in circulating gastrin may stimulate the parietal cell mass and promote the insertion of functioning molecules of H+,K+-ATPase into the secretory canaliculi. Since the peak plasma concentration of OME occurs around 30 min after ingestion of IR-OME, this allows for the rapid uptake of circulating OME by activated parietal cells leading to irreversible inhibition of a large proportion of available molecules of H+,K+-ATPase. This may help to explain both the rapidity of onset of the antisecretory effect and its prolonged duration. This hypothesis assumes that OME is principally absorbed from the proximal small intestine when ingested as IR-OME, just as with the conventional DR formulation. 1.2.13. Drawbacks of existing Immediate release PPI For instance, certain compositions of omeprazole, contain 1100 mg of sodium bicarbonate (equivalent to 300 mg of sodium) and oral suspension contains 1680 mg of sodium bicarbonate (equivalent to 460 mg of sodium). Such formulations utilizes the concept of microenvironment pH and hence a large quantity of alkali to neutralize the acid in the stomach, so as to protect the uncoated PPI from acid degradation. The American Heart Association's recommended daily intake of sodium is 2,400 mg for a normal person and these amounts should be taken into consideration by anyone on a sodium-restricted diet. Also, Sodium bicarbonate is contraindicated in patients with metabolic alkalosis and hypocalcemia (Ralph E Small, 2005). Also, such compositions weigh about 1.5-2.0 g making it difficult to swallow and hence leading to patient noncompliance. Further, since the amount of buffer depends on the pKa of the drug used, the amount of alkali required to make an immediate release composition of Pantoprazole or Rabeprazole, may be more than that required for Omeprazole. Moreover, sodium bicarbonate used in the composition has poor stability properties and decomposes by converting to carbonate and such; the decomposition is accelerated by agitation or heat (Wei-Youh Kuua et al., 1998). Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 32 Chapter 1 Introduction Hence, such compositions comprising large amount of buffers are also not suitable for long term usage. Findings indicate that sodium bicarbonate transiently buffers postprandial intragastric contents. Therefore, sodium bicarbonate fails to reconstitute the protein buffer of the meal effectively and the observations suggest that it leaves the stomach rapidly with the liquid phase of the meal. However, the water insoluble, aluminum-magnesium antacid has a longer duration of buffering, probably because it leaves the stomach more slowly, largely with the solid portion of the meal (Simmons et al., 1986). These formulations use the concept of micro environmental pH; also known as virtual pH. The micro environmental or virtual pH can be said as the pH of the immediate solution when the solid is dissolved in water. This virtual membrane pH determines the extent of drug ionization and hence drug dissolution and absorption. Thus the concept of microenvironment pH questions the basics of pH partition hypothesis. It has been demonstrated that the pH of the diffusion layer at the surface of the dosage form resembles that of a saturated solution of drug and excipients in a dissolution media and represents the microenvironment pH of the system (Bramhankar and Jaiswal, 1998). During dissolution, medium that may eventually penetrate into the core or during storage moisture may penetrate into the core resulting in a saturated solution of drug and excipients. If the microenvironment pH is low, it will lead to ultimate degradation of the drug. Hence; it is seen that the compositions of acid labile drugs of prior art either use an enteric coating or high concentration of buffers or are liable to degradation in the microenvironment pH. Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 33 Chapter 1 1.3. Introduction SPECIFICATIONS OF PANTOPRAZOLE - AN ACID-LABILE MODEL DRUG 1.3.1. Structure and physiology of Pantoprazole Pantoprazole is a membrane permeable substituted benzimidazole derivative that decreases gastric acid secretion by irreversibly inhibiting the H+/K+-ATPase located within gastric parietal cells (Cheer et al, 2003; Shi and Klotz, 2008; Sachs, 1997). It has high tissue selectivity for the canalicular lumen of the parietal cell, which has a pH of 1 (Richter et al, 2004). Like other PPIs, it is a weakly basic prodrug that accumulates within this highly acidic environment and becomes rapidly activated into a cationic sulphonamide (Cheer et al, 2003; Sachs, 1997; Calabrese et al, 2007). The protonated form then covalently binds to specific cysteine residues on the H+/K+ ATPase enzyme, thus irreversibly inactivating the pump. Compared to other PPIs, pantoprazole is less likely to become activated in neutral to moderately acidic environments (pH 3 to 5). The narrow pH window prevents pantoprazole from acting at nontarget areas in the body, thus reducing adverse effects (Cheer et al, 2003; Richter et al., 2004; Avner, 2000). In-vitro studies have shown that pantoprazole may actually have a longer duration of action than other PPIs because it is the only PPI to bind both cysteine 813 and cysteine 882, the more distal residue of the proton pump. Theoretically, the distal site is less accessible to agents such as glutathione or dithiothreitol that potentially reverse proton pump inhibition (Richter et al, 2004). Initially, Pantoprazole was approved for treatment and maintenance of erosive esophagitis (40 mg/day for 8 to 16 weeks) (Poole, 2001). Later in 2001, Pantoprazole IV was approved for short-term treatment (7 to 10 days) of GERD patients and a history of erosive esophagitis (40 mg/day), who are unable to tolerate oral Pantoprazole (Devault, 2007). Since then, the indications for Pantoprazole have expanded to include a variety of gastric acid-related diseases, including peptic ulcer disease (PUD), NSAID-induced ulcer prevention, Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 34 Chapter 1 Introduction Zollinger–Ellison syndrome and adjunctive therapy for Helicobacter pylori eradication (Poole, 2001). 1.3.2. Pharmacokinetics of Pantoprazole Pantoprazole follows dose linear pharmacokinetics. Oral Pantoprazole has a bioavailability of 77% and its absorption is not affected by food or antacids (Cheer et al, 2003). It is ultimately absorbed in the small bowel, resulting in a maximum serum concentration 2 to 3 hours post ingestion (Hartmann et al, 1996). Therefore, Pantoprazole is most effective when given prior to meals, so it reaches peak serum levels when the maximum number of proton pumps are activated postprandially (Devault, 2007). Unlike other PPIs, the serum concentration of Pantoprazole is not dose-dependent; serum concentration after 1 dose is similar to that after multiple doses (Van Rensburg et al, 1999). Pantoprazole is completely metabolized via the hepatic cytochrome P450 system by CYP2C19 and CYP3A4, and up to 80% of the inactive metabolites are eliminated via renal exctretion (Devault, 2007; Shi and Klotz, 2008). The metabolism of Pantoprazole is independent of the route of administration, with a half-life of approximately 1.1 hours (Cheer et al, 2003). However in patients with a mutation in the gene encoding the CYP2C19 enzyme, the half-life may be up to 3 hours (Tanaka et al, 2001). 1.3.3. Efficacy of Pantoprazole and current findings Numerous multicenter randomized control studies have shown Pantoprazole to be more efficacious than histamine-2 receptor antagonists (H2RAs) as the first-line drug for both treatment and maintenance therapy of erosive esophagitis associated with GERD (Cheer et al, 2003; Kahrilas et al, 2008; Gallo et al, 1998; Dammann and Von Kleist, 1997; Kovacs et al 2002). When compared to other PPIs, Pantoprazole has similarly efficacy in both the initial treatment and maintenance therapy of GERD. Although the efficacy seems to be Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 35 Chapter 1 Introduction relatively similar when comparing Pantoprazole to other PPIs, limited data indicate that Pantoprazole has a faster onset of symptom relief in patients with mild GERD (Scholten, 2000; Ehrlich et al, 1999). Pantoprazole is currently the only PPI that is FDA approved to treat night time symptoms of GERD (Castell et al, 2005). When compared to other PPIs, Pantoprazole has similarly efficacy in both the initial treatment and maintenance therapy of GERD. A double-blind, randomized, control study showed that Pantoprazole 40 mg/day and Esomeprazole 40 mg/day produce equivalent intraesophageal pH profiles and both similarly decrease esophageal acidity to normal levels 6 to 24 hours postingestion (Simon et al., 2003). Endoscopic healing rates at 4 weeks and 8 weeks show no statistically significant differences when comparing Pantoprazole 40 mg/day to Omeprazole 20 mg/day, Omeprazole multiple unit pellet system 40 mg/day and Lansoprazole 30 mg/day (Mulder et al., 2002; Glatzel et al., 2006; Koerner, 2002). For maintenance therapy, Pantoprazole 20 mg/day is equivalent to Esomeprazole 20 mg/day for both endoscopic healing rates and symptom control at both 6 months and 12 months (Goh et al., 2007; Laurtisen, 2000). Pantoprazole has been shown to improve health-related quality of life more effectively than H2RAs and with similar efficacy to other PPIs (Scholten, 2007; Enck et al., 1999; Dimenas et al., 1993; Holtmann, 2009). Pantoprazole 40 mg/day has also been shown to provide more effective control of night-time symptoms of GERD compared to esomeprazole 40 mg/day (Orr, 2005). Since pantoprazole is effective in controlling symptoms related to GERD and improving health-related quality of life, interest has arisen in using pantoprazole on an as-needed basis, rather than every-day doses. This concept is known as on-demand therapy. Although not currently FDA approved, on-demand therapy with Pantoprazole has been shown to be effective in the treatment of Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 36 Chapter 1 Introduction patients with mild GERD in randomized control studies (Scholten et al., 2007; Kaspari et al., 2005; Scholten et al., 2005). 1.3.4. Special administration considerations of Pantoprazole Conventional Pantoprazole is formulated as an enteric-coated, delayedrelease tablet. However, Pantoprazole is one of the few PPIs available in both iv and oral suspension form for the treatment of GERD in patients who are unable to tolerate the delayed-release capsule form (Devault, 2007). Pantoprazole iv, which was approved in 2001 by the FDA, has equivalent efficacy to oral Pantoprazole in its ability to suppress gastric acid output (Metz et al., 2000). In 2007, the FDA also approved Pantoprazole to be available in oral suspension form for the treatment of erosive esophagitis in patients unable to swallow capsules. Although studies are limited, a recent multicenter randomized control study (N = 60) showed oral suspension Pantoprazole to provide similar efficacy to oral capsules in suppressing gastric acid output (Hogan et al., 2007). 1.3.5. Safety and tolerability of Pantoprazole Short- and long-term clinical trials show oral Pantoprazole 40 to 120 mg/day to have an excellent safety profile (Fitton and Wiseman, 1996). Studies ranging from 8 weeks to 4 years have shown the incidence of adverse effects to be as low as 1% to 3% (Fitton and Wiseman, 1996; Martin de Argila, 2005). The most commonly reported side effects include diarrhea (2%), headaches (2%), nausea (1%), and constipation (1%). As with most PPIs, diarrhoea is the most prevalent of these side effects (Devault, 2007). Pantoprazole is both safe and effective in the initial treatment and maintenance therapy for the management of erosive and nonerosive GERD. It has superior efficacy to H2RAs and has relatively equivalent efficacy compared to Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 37 Chapter 1 Introduction other PPIs. It is efficacious for both esophageal healing and relief of symptoms associated with GERD. Pantoprazole’s favorable side effect profile and low incidence of drug–drug interactions make it ideal for using in special patient populations, such as the elderly and those with renal failure and moderate liver dysfunction. 1.4. CURRENTLY AVAILABLE DOSAGE FORMS OF PANTOPRAZOLE Pantoprazole is currently available in three dosage forms: a delayedrelease tablet, an intravenous infusion, and most recently, an oral suspension, provided as 40-mg unit dose packets, each containing enteric-coated granules. 1.5. CURRENTLY AVAILABLE IMMEDIATE RELEASE FORMULATIONS OF THE PPI The only non-delayed-release PPI formulation that is currently marketed is immediate-release omeprazole (IR-OME). This formulation consists of omeprazole protected from intragastric acid activation by sodium bicarbonate. The lack of enteric coating of IR-OME and the fact that it is administered as a liquid gives this preparation a theoretical advantage over other PPIs in regard to the onset of acid suppression and perhaps reduction in nocturnal acid breakthrough. It is currently available as immediate-release capsules and unit-dose packets as powder for oral suspension. Each capsule contains either 40 mg or 20 mg of omeprazole and 1100 mg of sodium bicarbonate. Packets of powder for oral suspension contain either 40 mg or 20 mg of omeprazole and 1680 mg of sodium bicarbonate and flavourings. Design And Development Of A Novel Concept For Immediate Release Of Pantoprazole 38