movement disorders and ataxia
advertisement

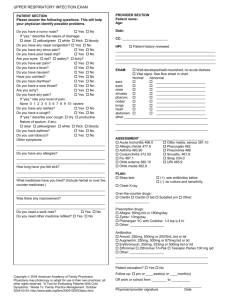
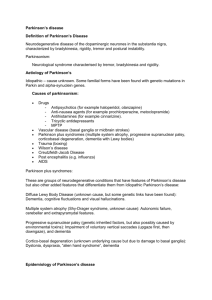
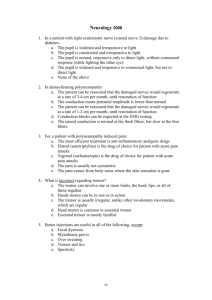
A. W. Flaherty MD, PhD, Dept. of Neurology, MGH Cambridge Hospital HMS III Tutorial 4/05 MOVEMENT DISORDERS AND ATAXIA A. Movement disorder consult service jingle: “Trouble with tone? Just get on the phone. Jerky or stiff? We’re there in a jiff.” B. H&P: What tasks are difficult? Nature and frequency of falls. Ask about incontinence, dementia, alcohol, benzodiazepine, or neuroleptic use. Assess facial expression, EOM, voice, handwriting, rapid movements, involuntary movements, tone, ability to rise from a chair, posture, postural reflexes, gait base and arm swing, Romberg sign, weakness, ataxia, festination, freezing. C. GAIT DISORDERS 1. Spastic gait: Stiff, circumducted leg(s), often flexor arm posturing. From corticospinal lesion. 2. Ataxic gait: Lurching, wide-based. Falls less common. From cerebellar (or rarely frontal) lesion. 3. Akinetic-rigid gait: Stooped, shuffling, trouble starting and stopping, often with tremor, decreased arm swing, poor postural reflexes. From basal ganglia lesion. 4. Frontal gait: Gait apraxia – trouble lifting feet, retropulsion, although leg movements may be normal in bed. Often mild ataxia. From cortical or white matter lesions; normal pressure hydrocephalus. 5. Neuropathic gait: High-stepping (steppage gait), Romberg positive, distal weakness. From peripheral nerve lesion. 6. Spastic ataxia: A characteristic bouncing gait. Often seen in multiple sclerosis, Chiari malformation, hydrocephalus in young people. 7. Others: Dystonic gait, choreic gait, action myoclonus, leg action tremor, abasia-astasia (psychogenic). D. CEREBELLAR OR BRAINSTEM MOVEMENT DISORDERS: 1. Function: The cerebellum aids movement error correction. 2. Signs: Ataxia, dysmetria; with vertigo, nystagmus, often N/V, irregular prosody. 3. Causes of cerebellar disorders: a. Acute: Bleed, infarct, toxins, drugs. Secondary edema may be life-threatening and require rapid neurosurgical intervention b. Subacute: Tumor, post-infectious cerebellitis, vasculitis, toxins, drugs. c. Chronic progressive: Alcoholism, Wilson's disease, drugs, toxins, Creutzfeldt-Jakob disease, hereditary cerebellar degeneration, hereditary metabolic diseases, paraneoplastic syndromes. d. DDx: Other gait disorders, above. E. BASAL GANGLIA MOVEMENT DISORDERS: 1. Anatomy: The basal ganglia form a circuit roughly containing the striatum (caudate nucleus + putamen), globus pallidus, and part of the thalamus – modulated by the subthalamic nucleus and, importantly, dopamine inputs from the substantia nigra. They act as a feedback loop on motor cortex. 2. Function: Crudely, determines the likelihood that the organism will move. Also important for habit learning. 3. Pathophysiology: The current model suggests that lesions that affect the excitatory pathway through the internal pallidum cause hypokinetic movement disorders, those that affect the inhibitory pathway through the external pallidum cause hyperkinetic ones. 4. Parkinsonism a. Pathophysiology: Dopaminergic neurons in the substantia nigra pars compacta die, causing dopamine depletion in the striatum (caudate nucleus and putamen). b. H&P: Rest tremor, bradykinesia, cogwheel rigidity. Response to Sinemet; on/off phenomena. Cognitive changes, depression, nightmares, hallucinations on drugs. Orthostasis, bladder changes. Look for masked facies, decreased arm swing, postural instability, festination. 1 c. Tests: None, except to exclude other diseases. In young pts, consider MRI, 24h urine copper, serum lactate. d. DDx of Parkinson’s disease (PD; idiopathic parkinsonism): ATYPICAL FOR PD: 1) Chemicals: e.g. neuroleptics, Wilson’s disease, manganese, carbon Age < 50 monoxide.... Sudden onset or fast progression 2) “Parkinson’s plus” syndromes: Usually poor response to Early falls Early dementia Sinemet. They include Lewy body disease (early hallucinations and Unusual tremor or myoclonus delirium), striatonigral degeneration (no tremor), Shy-Drager Early autonomic disturbances Poor levodopa response syndrome, AKA multiple system atrophy (more autonomic Gaze palsies dysfunction), progressive supranuclear palsy (more gaze palsy), Marked dysarthria or dysphagia Family history olivopontocerebellar atrophy (intention tremor; pseudobulbar signs) .... 3) Other: essential tremor, depression, arthritis, repeated head trauma (dementia pugilistica), normal pressure hydrocephalus, Creutzfeldt-Jacob disease.... e. Treatment of PD: 1) Dopaminergic agents: a) Levodopa + carbidopa (Sinemet). Start 25/100 (carbidopa/levodopa) qd, bring to tid over 3 wks if outpatient, ~3 days if inpatient. If necessary, increase up to total 1000 mg/d of levodopa, dosing q 2-4h. b) Selegeline (MAO-B inhibitor). Sometimes the first drug used. Start 2.5 mg bid, to 5 bid. c) Dopamine agonists: e.g. Mirapex (pramipexole): Start 0.125 mg tid, max 1.5 mg tid. Pergolide: Start 0.05 mg qd, to 2-4 mg/d. 2) Anticholinergics: Used less for idiopathic PD than for neuroleptic-induced Parkinsonism. 3) Amantidine: An NMDA-receptor blocker, best for suppressing dyskinesias. Start 100 mg qd; to 100 bid or tid. 4) Atypical neuroleptics: e.g. quetiapine (Seroquel). For dopa-induced hallucinations. a) Avoid traditional neuroleptics e.g. haloperidol. Watch out even for risperidone. 5) Surgery: Deep brain stimulator in the subthalamic nucleus. 5. Tremor: Oscillation from alternating contraction of antagonist muscles. a. Rest (Parkinsonian) tremor: 3-5 Hz, decreases during movement, often asymmetric, “pill-rolling.” b. Action tremors: Worse with movement. 1) Physiologic tremor: Normal, low-amplitude, 8-13 Hz. Worse with adrenergic stimulation (anxiety, caffeine, hyperthyroidism, sedative withdrawal…). 2) Essential (benign) tremor: Usually hereditary, 4-8 Hz. Rx includes a) Propranolol: start 10-20 mg tid, to 60-200 mg/d. b) Primidone: Start 50 mg qd, to 125 tid. c) Surgery: Thalamic stimulator. 3) Cerebellar “tremor”: Strictly, dysmetria. Oscillations worsen as limb approaches target. 4) Rubral tremor: Violent beating or flapping, from midbrain lesion. 5) Mixed action and rest tremors: usually a PD-plus syndrome, or drug effects (e.g. a bipolar patient on lithium and risperidone) 6. Dyskinesia: A general term for abnormal involuntary movements. Often a side-effect of drugs for Parkinson’s disease. 7. Choreoathetosis: Chorea is involuntary, rapid movements, often incorporated into voluntary movements. Athetosis is slower, more writhing. a. Causes of choreoathetosis: 1) Chemicals: Especially neuroleptics. 2) Immune-mediated: Sydenham’s, lupus, chorea gravidorum…. 3) Hereditary disorders: Huntington’s, Wilson’s, Hallervorden-Spatz disease, idiopathic torsion dystonia (DYT-1)…. a) Huntington’s disease: Autosomal dominant CAG repeat, genetic test available. Presents usually in adulthood with chorea or psychiatric symptoms. 2 b. Treatment of choreoathetosis: 1) Haloperidol: Start 0.5 mg tid, up to 8-16 mg/d. 2) Reserpine (depletes monamines): 0.5 mg qd. Not often used. Side-effects include angina, arrhythmia, N/V, depression. 8. Dystonia: Involuntary maintenance of abnormal posture or limb position from co-contraction of antagonists. When spasmodic, it grades into choreoathetosis. It is often task-specific and may be overcome with sensory tricks. a. DDx of dystonia: Spasticity, musculoskeletal lesion, choreoathetosis.... b. Causes of dystonia: 1) Acute: Reaction to antiemetic or neuroleptic, carbon monoxide, stroke.... 2) Chronic: a) Focal: Repetitive strain injury; idiopathic torticollis, writer’s cramp, blepharospasm, Meige’s syndrome (lip smacking and blepharospasm).... b) Global, hereditary: See causes of choreoathetosis, above. c. Treatment of dystonia: 1) Acute dystonic reaction: Diphenhydramine 50 mg IV/IM. 2) Chronic dystonia: a) Botox (botulinum toxin), for focal dystonias e.g. torticollis. b) Trihexyphenidyl (Artane, anticholinergic). Start 1 mg/d, to 1-6 tid. c) Benztropine (Cogentin, anticholinergic). Start 0.5 mg bid, to 0.5-4 bid. d) Other: Sinemet, baclofen, diazepam, carbamazepine, globus pallidus stimulation. 9. Tics: Quick, repetitive, semi-voluntary, coordinated movements or vocalizations, driven by urge, partly repressible. Compare chorea, myoclonus. a. DDx: Sydenham’s chorea, Wilson’s disease, Lesch-Nyhan’s syndrome, Tourette’s syndrome, myoclonus.... b. Rx: (generally not well-tolerated) 1) Clonidine (central alpha-agonist): Start 0.1 mg bid, to 2 mg/d. 2) Pimozide (or other D2 antagonist): Start 1-2 mg qd, to 8-16 mg qd. 10.Akathisia: Motor restlessness. Often a transient side-effect of a neuroleptic. 11.Asterixis: Irregular, slow, tremor-like flapping of hands, trunk, caused by temporary lapses of tone. a. Causes: Usually metabolic, e.g. liver failure. b. Treatment: Treat underlying cause. 12.Myoclonus: Brief, monophasic, irregular jerks from unopposed contraction of agonists (compare tremor, myotonia). Often precipitated by sensory stimuli. a. Causes of myoclonus: Encephalopathy, myoclonic epilepsy, benign essential myoclonus (including nocturnal myoclonus), physiological myoclonus (sleep jerks), drugs (e.g. opiates)…. b. Treatment of myoclonus 1) Clonazepam (benzodiazepine): start 0.5 mg tid, to 2 tid. 2) Valproic acid: Start 15 mg/kg/d divided bid-tid. 3) 5-OH-tryptophan: Start 100 mg bid, increase by 100 bid q 2-3 days to total of 500-750 bid. Can give carbidopa to decrease extracerebral metabolism. 13.Neuroleptic-induced movement disorders: a. Neuroleptic malignant syndrome: An emergency. Caused by a sudden release of calcium from sarcoplasmic reticulum as idiopathic response to a neuroleptic, or to withdrawal of antiparkinsonian drug. 1) H&P: Recent drugs. See tachycardia, then acidosis, tachypnea, arrhythmias, muscle stiffness, and fever. 2) DDx of NMS: Malignant hyperthermia, drug interactions with monoamine oxidase inhibitors, central anticholinergic syndromes, catatonia.... 3) Tests: ABG, electrolytes, CBC, CPK, EKG. 4) Treatment of NMS: a) Transfer to ICU. 3 b) Maintain ventilation. c) Surface and core cooling. d) Dantrolene: Start 1 mg/kg IV, repeat prn to 10 mg/kg/d. Beware hepatotoxicity, CHF. e) Bromocriptine: Start 2.5-10 mg IV/pNGT q 4-6h. b. Acute dystonia: Within a few days of drug initiation. See Dystonia, above, for treatment. c. Akathisia: Motor restlessness. Try propranolol 10-20 mg tid or clonazepam 0.5-1.0 mg bid. d. Subacute parkinsonian symptoms: Days to weeks after drug initiation. e. Treatment: Stop neuroleptic; add anticholinergic drugs (No indication for prophylactic use) 1) Benztropine 0.5-4.0 mg bid. 2) Trihexyphenidyl 1-5 mg bid-tid. 14.Tardive dyskinesia: Choreoathetosis, dystonia, orobuccal dyskinesia as late (> 1 yr) response to chronic neuroleptic use. a. Treatment: Switch to an atypical neuroleptic. Avoid anticholinergics. Consider tetrabenazine, reserpine. F. DOPAMINERGIC DRUGS 1. DA receptors: a. D1 receptors: Cause vasodilation. b. D2 receptors: inhibit sympathetic transmission, inhibit prolactin release, cause vomiting. c. D3, 4, 5 receptors: Less well-characterized; limbic more than motor effects. 2. DA agonists: Used for Parkinson’s disease, alertness disorders. a. Levodopa: a precursor to dopamine, used in Parkinson’s disease. Given with carbidopa, which blocks peripheral, but not central, levodopa use. b. Side-effects: N/V, low BP, confusion, dyskinesias, hallucinations. c. D2 agonists: e.g. bromocriptine, ropinrole, pramiprexole (D3 >D2). Side-effects like levodopa. d. D3 agonists: pergolide and pramiprexole are relatively selective agonists used for Parkinson’s. Sideeffects like levodopa; pergolide also associated with arrhythmia. e. Modafinil. (Provigil). Poorly understood, seems to work in hypothalamus to decrease sleepiness. f. Inhibitors of DA metabolism: 1) Monoamine oxidase inhibitors: a) MAO-B inhibitors: e.g. selegiline (Eldepryl). They slow dopamine degradation. For Parkinson’s Side-effects: N/V. Avoid opiates, TCAs and SSRIs (can cause hyperthermia, rigidity, autonomic instability). b) Nonspecific MAO inhibitors: Used as antidepressants. Many dietary and drug contraindications, notably meperidine (Demerol), SSRIs. 2) Amantidine: DA agonist, mechanism unclear, also anticholinergic and antiviral. a) Used for Parkinson’s disease, fatigue in multiple sclerosis. b) Side-effects: Well-tolerated; sometimes confusion, depression, edema. 3) COMT inhibitors: e.g. tolcapone (associated with fulminant liver failure). Used in severe Parkinson’s. 3. DA antagonists: neuroleptics e.g. haloperidol. Used for sedation, psychosis, antiemesis. Extrapyramidal side-effects are proportional to D2 binding. Generic name haloperidol perphenazine thioridazine clozapine risperidone quetiapine Trade name Haldol Trilafon Mellaril Clozaril Risperdal Seroquel Sedation, orthostasis +/++ ++++ ++++ +/+/- Extrapyr. symptoms ++++ ++ +/+/- Receptor D2, high D2, med D2, low 5HT>D2 5HT>D2 5HT>D2 4 G. THE BASAL GANGLIA AND PSYCHIATRY, or, why all movement disorders are psychogenic. More Coming Soon 5