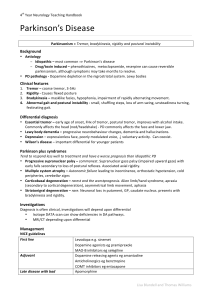
Parkinson`s disease
advertisement
Parkinson’s disease Definition of Parkinson’s Disease Neurodegenerative disease of the dopaminergic neurones in the substantia nigra, characterized by bradykinesia, rigidity, tremor and postural instability. Parkinsonism: Neurological syndrome characterised by tremor, bradykinesia and rigidity. Aetiology of Parkinson’s Idiopathic – cause unknown. Some familial forms have been found with genetic mutations in Parkin and alpha-synuclein genes. Causes of parkinsonism: Drugs - Antipsychotics (for example haloperidol, olanzapine) - Anti-nausea agents (for example prochlorperazine, metoclopramide) - Antihistamines (for example cinnarizine). - Tricyclic antidepressants - MPTP Vascular disease (basal ganglia or midbrain strokes) Parkinson plus syndromes (multiple system atrophy, progressive supranuclear palsy, corticobasal degeneration, dementia with Lewy bodies) Trauma (boxing) Wilson’s disease Creutzfeldt-Jacob Disease Post encephalitis (e.g. influenza) AIDS Parkinson plus syndromes: These are groups of neurodegenerative conditions that have features of Parkinson’s disease but also other added features that differentiate them from Idiopathic Parkinson’s disease: Diffuse Lewy Body Disease (unknown cause, but some genetic links have been found): Dementia, cognitive fluctuations and visual hallucinations. Multiple system atrophy (Shy-Drager syndrome, unknown cause): Autonomic failure, cerebellar and extrapyramydal features. Progressive supranuclear palsy (genetic inherited factors, but also possibly caused by environmental toxins): Impairment of voluntary vertical saccades (upgaze first, then downgaze), and dementia Cortico-basal degeneration (unknown underlying cause but due to damage to basal ganglia): Dystonia, dyspraxia, “alien hand syndrome”, dementia Epidemiology of Parkinson’s disease • Overall prevalence ≈ 160 / 100 000 • Incidence rates ≈ 20 / 100 000 / year • 2% of people over 80 are affected • Mean age at onset 60 Presentation – symptoms and signs Classic triad – Bradykinesia, pill rolling tremor, rigidity But UK Brain Bank Criteria is bradykinesia AND at least one of rigidity, 4-6Hz tremor, or postural instability Ask about: Onset - gradual Tremor – at rest, usually first noticed in the hands Stiffness and slowness of movement. Difficulty initiating movements (e.g. getting out of chair, rolling in bed) Falls – Not usually frequent early on Smaller hand writing (micrographia) Important: Remember that often patients will be more concerned about the non motor symptoms than the motor symptoms. The non-motor symptoms can be grouped into psychiatric and non-psychiatric. Most common are anxiety and depression, which many Parkinson's disease patients will have. There are also a long list of non-psychiatric symptoms such as insomnia,constipation, weight loss, urinary incontinence, and sexual dysfunction. Examination Remember there are a huge number of things you can comment on by just observing someone with Parkinson’s disease: - Tremor, decreased by action and usually asymmetrical Expressionless face (hypomimia), Frontalis overactivation (furrowing of the brow), soft monotonous voice (hypophonia). Gunslinger posture/Hands over hernias You should also get the patient to walk to assess their gait, check for rigidity, bradykinesia, and assess function: - - - Gait – Stooped posture, shuffling, small steps, reduced arm swing. Freezing (difficulty initiating walking) Rigidity – Leadpipe rigidity of muscle tone, with superimposed tremor (giving rise to cogwheel rigidity) Rigidity can be increased by distraction, e.g. by asking the patient to clap one hand on their thigh while you check tone in the other hand. Bradykinesia – thumb-finger test (Crab-claw test). Ask the patient to quickly open and close their hand with finger opposed to thumb. Parkinson’s patients are very slow to do this usually. Function – ask them to write, or do up some buttons. In the exam you could state after your initial examination that you would do a MMSE if you had more time to check for dementia Investigations Parkinson’s disease is a clinical diagnosis but investigations can be of help in excluding other causes of parkinsonism: Bedside tests o Levodopa trial – timed walking and clinical assessment after levodopa. Blood tests o Routine bloods o Serum ceruloplasmin for Wilson’s disease Imaging o CT and MRI usually normal but may exclude other causes of parkinsonism or gait decline (vascular disease, hydrocephalus) o Special tests – Dopamine transporter scintigraphy (DAT): Reduction in striatum and putamen. May be necessary to distinguish Parkinson’s from essential tremor. Management Conservative o Support societies o Physio o OT Medical o Dopamine agonists e.g. ropinirole, bromocriptine o MAO inhibitors e.g. selegeline o Levodopa + decarboxylase inhibitor o COMT e.g. Entacapone o Continuous dopamine therapy – Apomorphine (syringe driver) or Duodopa (Intrajejunal infusion of levodopa gel) o Supportive medication e.g. baclofen Dopamine agonist Significant functional disability Disease progression MAO-B inhibitor Levodopa (max 600mg/day) Add levodopa (max 600mg/day) Motor complications develop Guidelines for drug management of PD Add DA or entacapone Add entacapone or DA Switch to tolcapone if entacapone fails Add MAO-B inhibitor if not already given Add amantadine for dyskinesia Severe motor complications Consider apomorphine, Duodopa, DBS Surgery Stereotactic thalamic surgery - Bilateral subthalamic nucleus stimulation (deep brain stimulation) May reduce levodopa requirements and therefore reduce levodopa induced dyskinesias Complications of treatment (develops over months and years on chronic levodopa therapy): - On-off motor fluctuations Peak dose dyskinesias (typically choreiform/dancelike) On-off dystonia Impulse control disorders (e.g. pathological gambling, hypersexuality) Prognosis • Progression variable • Usually the course is over 10-15 years • Death from bronchopneumonia References/Sources: - Sam AH, Teo JTH, Rapid Medicine, Wiley-Blackwell 2010 - BMJ learning module: Parkinson's disease - initial assessment and referral - Lecture by Zoe Campell, Warwick Hospital, 2012 - SADH lecture by Naghme Adab, Management and treatment of Parkinson’s Disease, 2012