Neuro-Other
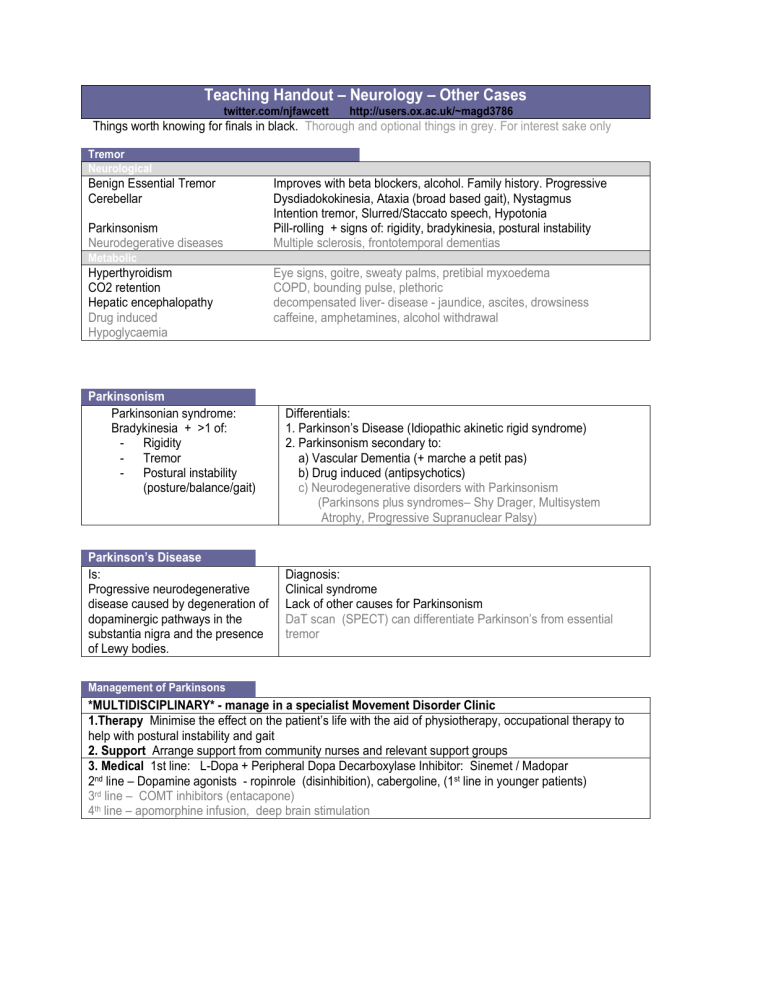
Teaching Handout – Neurology – Other Cases
twitter.com/njfawcett http://users.ox.ac.uk/~magd3786
Things worth knowing for finals in black. Thorough and optional things in grey. For interest sake only
Tremor
Neurological
Benign Essential Tremor
Cerebellar
Parkinsonism
Neurodegerative diseases
Metabolic
Hyperthyroidism
CO2 retention
Hepatic encephalopathy
Drug induced
Hypoglycaemia
Improves with beta blockers, alcohol. Family history. Progressive
Dysdiadokokinesia, Ataxia (broad based gait), Nystagmus
Intention tremor, Slurred/Staccato speech, Hypotonia
Pill-rolling + signs of: rigidity, bradykinesia, postural instability
Multiple sclerosis, frontotemporal dementias
Eye signs, goitre, sweaty palms, pretibial myxoedema
COPD, bounding pulse, plethoric decompensated liver- disease - jaundice, ascites, drowsiness caffeine, amphetamines, alcohol withdrawal
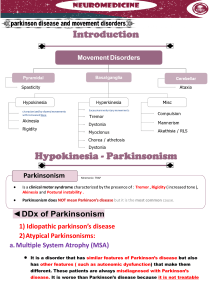
Parkinsonism
Parkinsonian syndrome:
Bradykinesia + >1 of:
Rigidity
Tremor
Postural instability
(posture/balance/gait)
Differentials:
1. Parkinson’s Disease (Idiopathic akinetic rigid syndrome)
2. Parkinsonism secondary to:
a) Vascular Dementia (+ marche a petit pas)
b) Drug induced (antipsychotics)
c) Neurodegenerative disorders with Parkinsonism
(Parkinsons plus syndromes– Shy Drager, Multisystem
Atrophy, Progressive Supranuclear Palsy)
Parkinson’s Disease
Is:
Progressive neurodegenerative disease caused by degeneration of dopaminergic pathways in the substantia nigra and the presence of Lewy bodies.
Diagnosis:
Clinical syndrome
Lack of other causes for Parkinsonism
DaT scan (SPECT) can differentiate Parkinson’s from essential tremor
Management of Parkinsons
*MULTIDISCIPLINARY* - manage in a specialist Movement Disorder Clinic
1.Therapy Minimise the effect on the patient’s life with the aid of physiotherapy, occupational therapy to help with postural instability and gait
2. Support Arrange support from community nurses and relevant support groups
3. Medical 1st line: L-Dopa + Peripheral Dopa Decarboxylase Inhibitor: Sinemet / Madopar
2 nd line – Dopamine agonists - ropinrole (disinhibition), cabergoline, (1 st line in younger patients)
3 rd line – COMT inhibitors (entacapone)
4 th line – apomorphine infusion, deep brain stimulation
Causes of Stroke
Haemorrhagic
Hypertension
Aneurysm / Arteriovenous Malformation
Amyloid Angiopathy
Ischaemic
Embolic - AF/ LV thrombus/LV aneurysm/PFO and paradoxical embolus, atrial myxoma
Atherosclerosis and thromboembolic– carotid( or vertebral) plaque or dissection
‘Haemodynamic ‘ – carotid or intracerebral circulation stenosis
Freidreich’s Ataxia
Is:
Congenital autosomal recessive multisystem degenerative disorder
Predominantly causing ataxia and a progressive mixed UMN and LMN deficit.
Degeneration of
Spinocerebellar, corticospinal and dorsal column tracts, and peripheral nerves.
CAA repeat in the Frataxin gene causing silencing
Defect in mitochondrial metabolism
Neurology
ATAXIA (spinocerebellar tract degeneration)
Combination of spastic and flaccid weakness, loss of deep tendon reflexes
Predominantly dorsal column sensory loss, can progress to full sensorimotor deficit 2’ peripheral nerves
Upgoing plantars (UMN) and absent ankle jerks (LMN)
Also:
Retinopathy and blindness
Cardiomyopathy and conduction defects
Scoliosis
Diabetes type I and II
Management:
MULTIDISCIPLINARY
“I would take a multidisciplinary approach to management, and involve the relevant physiotherapy, occupational therapy and social support to minimise the effect of the underlying disease on the patient’s quality of life . “
Medical –
No current treatment of underlying disease
Treat complications as appropriate (baclofen, antiarrythmics, warfarin, insulin therapy etc.)
Surgical-
Tendon release, scoliosis surgery