Benzodiazepines & anxiety
advertisement
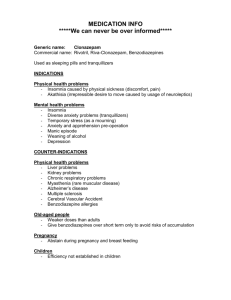
Benzodiazepines & anxiety 1. Outline the current treatment of anxiety disorders Primary Treatments: - psychological counseling - drug treatment o Sedative-hypnotics (eg benzodiazepines – BZDs) o Antidepressants o Antipsychotics Sedative-hypnotics-anxiolytics: Depress the CNS, with their effect being critically linked to dose. At low to high dose the effects range from: - tranquilisation (relaxed, unconcerned patient) - sedative (decreased patient activity, calmed & awake) - hypnotic (drowsy patient, facilitates sleep onset and duration) - anaesthesia (loss of consciousness, patient cannot be aroused) Benzodiazepines are sedative-hypnotic agents that relieve anxiety (for example, for pre-operation anxiety). The first used was chlordiazepoxide (1961), and there are now many. They are classified according to their duration of action, but do differ in activity as well. They are also useful for treating insomnia, alcohol withdrawal, and muscle spasm. 2. Describe the function of GABAA receptor chloride channels in neuronal excitability. Gamma-aminobutyric acid (GABA) is the primary fast inhibitory neurotransmitter in the brain. The effect of GABA is to open Cl- channels in its receptor (GABAA), causing the cell to become hypopolarised. This causes an inhibitory effect on neurotransmission by diminishing the chance of a successful action potential occurring. The GABA receptors contain an α1 and α2 subunit, which account for anxiolytic/muscle relaxant, and sedative/amnesic/anticonvulsant properties respectively. Hence α1-selective drugs should not display sedation. 3. Indicate the effects of benzodiazepines, alcohol and barbiturates on these channels. BZDs, ethanol, and barbiturates allosterically enhance the affinity of GABA for the GABAA receptor. Binding of benzodiazepines to this receptor complex promotes binding of GABA, which in turn increases the conduction of chloride ions across the neuronal cell membrane. This increased conductance raises the membrane potential of the neuron resulting in inhibition of neuronal firing. The binding site for benzodiazepines is distinct from the binding site for barbiturates and GABA on the GABAA receptor, and also produces different effects on binding,[11] with the benzodiazepines causing bursts of chloride channel opening to occur more often, while the barbiturates cause the duration of bursts of chloride channel opening to become longer. Regarding ethanol, the main theories of action are as follows: - Enhancement of GABA mediated inhibition, similar to the action of benzodiazepines - Inhibition of calcium entry through voltage gated calcium channels - Inhibition of NMDA receptor function 4. Relate the duration of effect of benzodiazepines to the presence of active metabolites. Many of the metabolites of BZD are pharmacologically active, increasing the duration of action of the drug in the body. The primary compound is also active. Hence the duration of action may not be related to the half-life of elimination of the parent compound (as is typical in many other drugs). Benzodiazepines are orally active, but can be given through IV or intramuscular injection. 70-99% bound to plasma proteins and all are completely absorbed across the GIT within ~1hour. Peak plasma concentration in ~ 1 hour, and excreted as glucuronide conjugates in urine. Metabolism of benzodiazepines occurs in three main phases: o Phase 1: Removal of extra groups o Phase 2: Hydroxylation (40- 50 hours) o Phase 3: Conjugation with glucuronic acid (6- 12 hours) Nb Some are metabolised by CYP enzymes into active metabolites which have a long half-life (60 hrs). Metabolism can also cause the production of active metabolites. In these cases the half life of the active metabolites will influence the duration of action of the benzodiazepine dose: - Benzodiazepines which have active metabolites have a longer duration of action (e.g. diazepam > desmethyldiazepam) . - Those have no active metabolism or which are inactivated immediately upon metabolism (e.g. temazepam, oxazepam) have a shorter half life. 5. Briefly outline the management of benzodiazepine overdose in particular the use of flumazenil and activated charcoal Generally BZDs are relatively safe, with respiratory assistance needed only if patients have taken another CNS depressant (eg alcohol). Overdose situation can arise from the above description, where active metabolites of BZD remain in the body when subsequent doses are given – although these instances are rare. Alternatively these drugs are used in a more extreme ‘overdose’ scenario. Flumazenil is a selective competitive antagonist of the GABA receptor and the only available specific antidote for BZDs. In an overdose situation, cardiac regularity, IV, oximetry, and vital signs should be monitored. Activated charcoal (a charcoal material that will absorb phenolic compounds) at single dose can be used if within 4hrs of ingestion, and is used to minimize the systemic absorption of the toxin. Ie it will absorb drug present in the GIT. Although benzodiazepines are adsorbed by activated charcoal, gastric decontamination with activated charcoal is not beneficial in pure benzodiazepine overdose as the risk of adverse effects would outweigh any potential benefit from the procedure. It is only recommended if benzodiazepines have been taken in combination with other drugs that may benefit from decontamination.