SWOT AnalysisTemplate – 23 7 15 Summary OT
advertisement
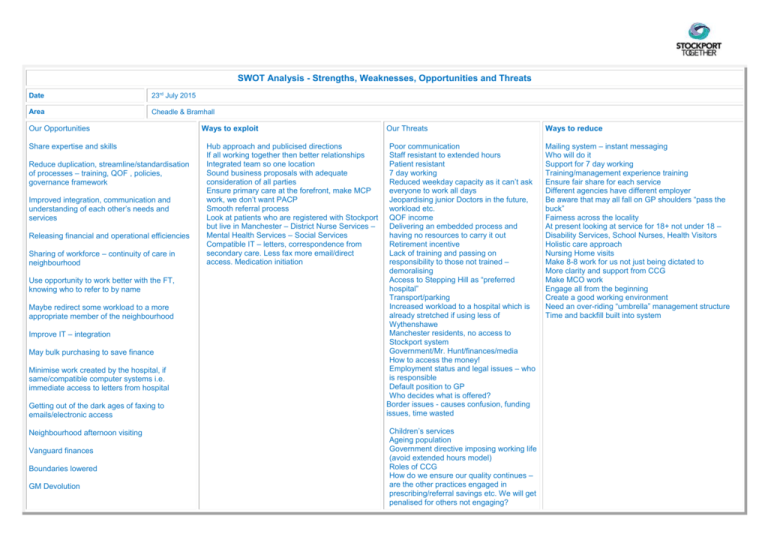
SWOT Analysis - Strengths, Weaknesses, Opportunities and Threats Date 23rd July 2015 Area Cheadle & Bramhall Our Opportunities Share expertise and skills Reduce duplication, streamline/standardisation of processes – training, QOF , policies, governance framework Improved integration, communication and understanding of each other’s needs and services Releasing financial and operational efficiencies Sharing of workforce – continuity of care in neighbourhood Use opportunity to work better with the FT, knowing who to refer to by name Maybe redirect some workload to a more appropriate member of the neighbourhood Improve IT – integration May bulk purchasing to save finance Minimise work created by the hospital, if same/compatible computer systems i.e. immediate access to letters from hospital Getting out of the dark ages of faxing to emails/electronic access Neighbourhood afternoon visiting Vanguard finances Boundaries lowered GM Devolution Ways to exploit Hub approach and publicised directions If all working together then better relationships Integrated team so one location Sound business proposals with adequate consideration of all parties Ensure primary care at the forefront, make MCP work, we don’t want PACP Smooth referral process Look at patients who are registered with Stockport but live in Manchester – District Nurse Services – Mental Health Services – Social Services Compatible IT – letters, correspondence from secondary care. Less fax more email/direct access. Medication initiation Our Threats Ways to reduce Poor communication Staff resistant to extended hours Patient resistant 7 day working Reduced weekday capacity as it can’t ask everyone to work all days Jeopardising junior Doctors in the future, workload etc. QOF income Delivering an embedded process and having no resources to carry it out Retirement incentive Lack of training and passing on responsibility to those not trained – demoralising Access to Stepping Hill as “preferred hospital” Transport/parking Increased workload to a hospital which is already stretched if using less of Wythenshawe Manchester residents, no access to Stockport system Government/Mr. Hunt/finances/media How to access the money! Employment status and legal issues – who is responsible Default position to GP Who decides what is offered? Border issues - causes confusion, funding issues, time wasted Mailing system – instant messaging Who will do it Support for 7 day working Training/management experience training Ensure fair share for each service Different agencies have different employer Be aware that may all fall on GP shoulders “pass the buck” Fairness across the locality At present looking at service for 18+ not under 18 – Disability Services, School Nurses, Health Visitors Holistic care approach Nursing Home visits Make 8-8 work for us not just being dictated to More clarity and support from CCG Make MCO work Engage all from the beginning Create a good working environment Need an over-riding “umbrella” management structure Time and backfill built into system Children’s services Ageing population Government directive imposing working life (avoid extended hours model) Roles of CCG How do we ensure our quality continues – are the other practices engaged in prescribing/referral savings etc. We will get penalised for others not engaging? Reduce bureaucracy Sector specialists e.g. GPSI, sector Consultants, Physios and other paramedical staff Phlebotomy service and house bounds for locality Visiting Doctor for locality Border issues Reduce silo working Could increase QOF – increase access in chronic disease management e.g. weekends – asthma reviews, diabetics reviews, especially Practice Nurse time Acute care – neighbourhood afternoon visiting Minimise work generated from hospital Community organisation – access to GP records/IT? (Social, District Nursing) Patient access to records Public Health/prevention in neighbourhoods Quick response times to support practices e.g. Acupuncture/yoga Co-location in the neighbourhood – DN, Physio, CPN, OT Possible employ on a neighbourhood basis Opportunities for more commissioning services at a local level, shape outcome not respond probably more efficient Keep out of PACS model Solution to threat of 7 day working Better outreach with diabetics/Geriatricians Financial – QOF (templates, computer access) Stepping Hill – access, parking. Increased workload to already stretched hospital if preferable over Wythenshawe Financial – funding. The reorganisation, could funding be an issue i.e. individual GP contracts GM versus national Financial – pensions, with changes in funding etc. Manchester residents access to Stockport system Staff registered with another neighbourhood/practice Patients – they are opting out of the spine but now having to agree to their records being accessed by the neighbourhood or Social Workers having access 7 days what about weekend phlebotomy – hospital lab involvement Pharmacy in community, Sunday opening? Don’t know what funding is available Larger organisation may not be sufficiently flexible/may be protectionist Does hospital have capacity and can Consultants have the time/desire to change Will it results in merged practices? What will Vanguard offer? PCAS system None engagement/resistance Less finance Change of culture/thinking Recruiting good quality staff, clinical and admin Maintenance of quality – who will regulate Contract payments may not change Wythenshawe Time for regular meetings in neighbourhood local OP services Opportunities to work with the third sector Opportunity to co-produce with District Nurse, keeps out PACS model Refashioning of secondary care services, specialist opportunistic opinion Opportunities for better working Avoiding admission Avoiding referral rates Reducing administration and duplication Use of GPSI within locality, minor ops Specialist Nurse clinics, DM, COPD, HF, travel, FP, Ims Geriatrician to phone/email Joining up MDT working over boundaries