Ⅰ. Choice: Select the single most appropriate answer.
advertisement

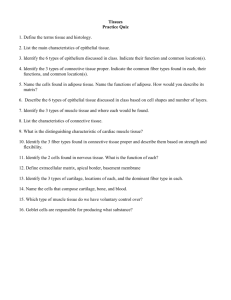
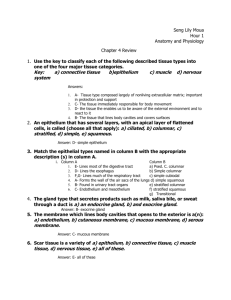
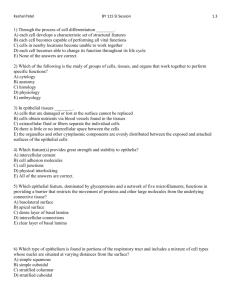
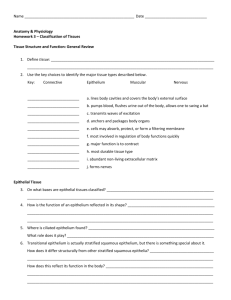
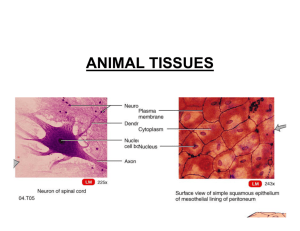
Exercise 1 for Histology (Epithelial tissue) I. 1.A II. 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. Choice: Select the single most appropriate answer.: 2.B 3.A 4.B Fill in the blanks: Eosin, Hematoxylin polysaccharides fixation, dehydration, embedding, stainin the surface features connexins epithelial tissue, muscle tissue, nerve tissue and connective tussie Mesothelium, Endothelium tight junction, intermediate junction, desmosome, gap junction, junctional complex Hemidesmosomes, basement membrane , basal infolding Goblet Cell , columnar cell , basal cell Cuboidal, polygonal, Squamous A Goblet Cell III. Questions: 1. Describe the characteristics of epithelial tissue. General structural feature:1)sheets; 2) polarization 3) avascularity 4) innervation Function: protection; secretion; absorption; excretion; sensory reception 2. Describe the structural characteristics and functions (location) of each covering epithelial type. Simple squamous – endothelium, mesothelium, endocardium, and lung – barrier Simple cuboidal – small ducts of exocrine glands – barrier, excretion / absorption Simple columnar – stomach lining and gastric glands – barrier and absorption / secretion Psuedostratified – bronchial tree and trachea – secretion Stratified squamous – skin, oral cavity, vagina – barrier major function transitional epithelium– bladder, urethra – barrier 3. Compare the structure of microvilli with cilia. Microvilli: finger-like projections of cell-membrane and cytoplasm protruding from the free surface. 0.1um in diameter, with different longth. The core of microvilli contains fine 6nm actin filaments running along their longitudinal axes which are capable of contraction. Cilla: elongated, mobile projections from the free surface, 5-10um long, 300-500nm in diameter, the axoneme of a cilium is composed of nine outer doublet microtubules and two central singlet microtubules 4. Compare the structure of intermediate junction with desmosome. intermediate junction 1) below the tight junction 2) a gap of 15-20nm in width with medium electron-density filament material 3) plaque of electron-dense materials, with attached microfilament-make up of terminal web desmosome 1) plate or spot-shaped 2) a gap of 20-30 nm, with low electron-density filaments interdigitate 3) Many tonofilaments are inserted into attachment plaque, each filament make a hairpin loop and then passes back into the cytoplasm Exercise 2 for Histology (Connective tissue) I. 1.E Choice: Select the single most appropriate answer.: 2.B 3.D 4.C II. Fill in the blanks: 1. cells, fiber, ground substance 2. proper connective tissue, blood, cartilage and bone 3. loose connective tissue, irregular dense connective tissue, regular connective tissue, reticular tissue, adipose tissue 4. arterial end, venous end 5. Chondroitin sulfate, Dermatan sulfate, Keratan sulfate, Heparan sulfate 6. bacteria, other microorganisms 7. fibroblast, macrophage, mast cell, plasma cell, fat cell, undifferentiated cell, wandering cell 8. collagenous fiber, elastic fiber, reticular fiber 9. rough endoplsmic reticulum, free ribosome, Golgi complex 10. α-chain, procollagen molecule, tropocollagen molecule 11. lysosomes, pinosomes, phagosomes 12. heparin, histamine, slow-reacting substance, eosinophil chemotactic factors, 13. reticular cells, reticular fibers III. Questions: 1. Describe the characteristics of connective tissue. 1) small number of cells and large amount of extracellular matrix (intercellular material) 2) the extracellular matrix is composed of fibers and an amorphous ground substance 3) all of them originate from mesenchyme -embryonic CT 4) functions: connection, supporting, protecting, nutrition, defense and repairing 2. Compare the structure of collagen fibers with elastic fibers. Collagen fiber: 1) 1-20 um in diameter, have periodic cross striation at 64nm interval 2) Belt-liked wave and branch to form a network 3) Eosinophilic elastic fiber: 1) thinner and less, 0.2-1.0 um 2) Slight red (HE) 3) branch and form a network 4) core: an amorphous substance--elastin-low electron density, 5) Peripheral: microfibril 10-12 nm, electron dense 3. Compare the fine structure and function of fibroblast with macrophage under the light microscope. Fibroblast: • large,flattened cell with processes, stellate in shape • Large ovoid pale nucleus - contain more fine chromatin, with clear one or two nucleoli • Weakly basophilic cytoplasm • function: synthesis of fibers and ground substance macrophage: • • • • • Round, ovoid or irregular in shape have short blunt processes: pseudopodium Small and dark nucleus Acidophilic cytoplasm Functions: Chemotaxis: chemotactic factor Phagocytosis Bioactive product secretion: lysozyme, complement and interleukin-1 (IL-1)and interferon(INF) Antigen presenting function 4. Compare the structure of plasma cell with mast cell. Plasma cell: • round or ovoid in shape • Nucleus with more clock-liked heterochromatin which located eccentrically • Basophilic cytoplasm Mast cell: • • • round and large cell Small dark-stained nucleus Basophilic secreting granules--metachromatically Exercise 3 for Histology (Cartilage and bone, blood) I. Choice: Select the single most appropriate answer.: 1.E II. 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 2.A 3.D 4.B Fill in the blanks: chondrocyte, fiber, griund substance cartilage tissue, perichondrium hyaline cartilage, elastic cartilage, fibrocartilage appositional growth, intersitial growth refractive index, delicate fibrils calcium, hydroxyapatite bone cells, ground substance, fibers osteoprogenitor cell, osteoblast, osteocyte, osteoclast periosteum, spongy bone, compact bone, endosteum, bone marrow outer circumferential lamellae, interstitial lamellae, osteons, inner circumferential lamellae, cement plasma, blood cells, erythrocytes, leukocytes,platelets haemoglobin, reticulocytes (4.2-5.5)X1012/L , 100-300×109/L biconcave, nuclei leukemia, leucopenia peripheral zone, organelle zone reticular tissue, hemopoietic cell, sinusoid epiphyseal plate, bone tissue III. Questions: 1. Describe the structural characteristic of chondrocyte. LM • embedded in cartilage lacuna • peripheral cells: --small and immature --single and flattened • central cell: --large and mature, --round and in group of 2-8 cells: isogenous group --small and round nucleus --basophilic cytoplasm --EM: rich in RER and Golgi complex 2. Describe the structural of bone matrix ( or bone lamellae). Thin layers a) Each layer contains collagen with one orientation b) c) d) Adjacent layers have different orientations Osteocytes are in lacunae between lamellae Both compact and spongy bone are lamellar bone Organic matrix: fibers and ground substance • Collagen Type I, up 90% of organic matter • Proteoglycans and Noncollagenous glycoproteins Inorganic matrix • About 65% of the weight of a bone • Calcium hydroxyapatite: crystalline calcium phosphate salts – – Deposited in and between collagen fibrils The mineral salts are responsible for the hardness and rigidity of bone 3. Compare the morphologic features of osteoblast with osteocyte and osteoclast. Osteoblast: Oval or pear-shaped Strong basophilic cytoplasm Osteocyte: flattened cell with multiple long thin processes located in bone lacuna basophilic cytoplasm adjacent cells connect in bone canaliculi by gap junctions soteoclast: irregularly shaped, 30-100um multinuclear large cell, 6-50 nuclei acidophilic cytoplasm 4. Describe the classification, percentage, size, structure and function of leukocytes. • granulocytes: neutrophil 50-70%, round, 10-12um in diameter, rob-liked or polymorphous nucleus, 2-5 lobes, fine neutrophilic granules-pink cytoplasm, Neutrophils are one of the most important lines of defence against bacterial infection. Eosinophil 0.5-3%, round,10-15 um in diameter, 2 lobes nucleus, rough bright red granules -acidophilic granules, counteract the infection of parasite reduce allergic reaction Basophil 0-1%, less, round 10-12 um , “S” shaped or irregular nucleus, Large, dark blue-staining granules, contains heparin, histamine and acidophil chemotactic factor, precise function is unknown, involve in allergic reaction • agranulocytes: lympocyte 20-30% , round, small LC 6-8 um, medium-sized LC 9-12 um, large LC 13-20 um in diameter, round nucleus appears as spot-liked and electron-dense , cytoplasm: less, basophilic--bright blue in color, contain azurophilic granules, involve in immune respons monocyte 3-8% , large round, 14-20um , nucleus appear as kidney, horse-shoe or ovoid in shape, cytoplasm: gray-blue in color, contain azurophilic granules, actively mobile and chemotaxis. Exercise 4 for histology (Muscular tissue) I. Choice: Select the single most appropriate answer.: 1.B 2.E 3.E 4.C II. Fill in the blanks: 1. skeletal muscle, cardiac muscle, smooth muscle 2. Z line, I band, A band, I band 3. terminal cisternae, transverse tubule, terminal cisternae 4. thin filament, thick filament, thin filament, thick filament 5. actin, tropomysin, troponin 6. endomysium, perimysium, epimysium 7. intercalated discs, desomosome, intermediate junction, gap junction 8. terminal cisternae, transverse tubule 9. dense patch, dense body, cytoskeleton 10. thin filament, thick filament, intermediate filament III. Questions: 1. Describe the characteristics of muscle tissue. components: ---cell: muscle cell-myofiber • Sarcolemma: muscle cell membrane • Sarcoplasm: the cytoplasm of muscle cell • sarcoplasmic reticulum: SER ---extracellular ground substance: CT with BV, LV and nerve classification According to the structure and function • skeletal muscle: striated voluntary muscle • cardiac muscle: striated involuntary muscle • smooth muscle: unstriated involuntary muscle Function: Muscle tissue is responsible for: -movement of the body and its parts -changes in the size and shape on internal organs 2. Compare the similar with the difference for three kinds of muscle cells according to their fine structure and ultrastructure. Skeletal muscle: LM: - long cylindrical, 10-100um in diameter,1-40mm long - Striated, composed of alternating dark and light bands - multinucleate, nuclei are ovoid, distributed under sarcolemma EM: • Each muscle fiber contains many longitudinal parallel-arranged myofibrils • Each myofibril contains many microfilaments Cardiac muscle: LM: • short column with branches in shaped, 100um long,15um in diameter, the branches associated with each other to form a network • 1-2 ovoid centrally-located nuclei • striated, but no very clear • intercalated disc: junctional part EM • similar to skeletal muscle, composed of thick, thin filament and have sarcomere • myofibril have different diameter, the boundary of myofibril is not very clear • Abundant mitochondria Smooth muscle: LM • elongated, spindle-shaped cells, marked variation in length and diameter • rod-liked or ovoid central nucleus • no striation • The narrower portion of one cell lies against the wider portions of its neighbor EM: • caveola: sarcolemma invaginate into cytoplasm • dense patch: inner surface of sarcolemma dense body: in sarcoplasm • intermediate filament: expand from one dense body to the next one, as well as to the dense patches, which constitute a cytoskeleton 3. Describe the molecular structure of myofilaments in detail. thick myofilament: myofibril • 1.5 um long, 15nm in diameter • Occur in place of the A-band • composed of myosin: -rod: in bundles -head: cross bridge- binding site (ATPase activity) thin myofilament: • Present in the I-band and extend for some distance into A-band • 1um long, 5nm in diameter A. actin: • spherical monomers of globular-actin arranged in two row and twisted around each other. Each individual strand is termed filamentous (F)-actin • Each monomer has a binding site for myosin B. tropomyosin: • a long filamentous protein composed of two polypeptide chains • Run along the outer edges of the groove between the two twisted actin strands C. troponin: three sub-units: -Tn T: strongly attaches to tropomyosin -Tn C: binds calcium ions -Tn I: inhibits the actin-myosin interaction 4. Explain briefly the contraction mechanism of the striated skeletal muscle. a. Myoneural junction transfer the impulse from NF to sarcolemme. b. The impulse spreads to interior part of cell by T- tubule, then through the triad, impulse is transferred to sarcoplasmic reticulum, the calcium ions are released to sarcoplasm. c. Calcium bind to Tn C, troponin and tropomyosin change their position and structure, the binding site on actin and myosin is exposed d. Binding site on actin and myosin combine, ATP(adenosine triphosphate) are splited into ADP(adenosine diphosphate) by ATPase on head of myosin, and energy are release. The energy is provided to band the head in the direction of M-line, and actin filament are pulled toward to M line. Muscle contraction. e. After contraction, calcium ions in sarcoplasm are withdrawed into sarcoplasmic reticulum. A new ATP molecules bind to the myosin, the actin-myosin separated, troponin-tropomyosin cover the binding site, the myofiber relax. Exercise 5 for histology (Nervous tissue) I. Choice: Select the single most appropriate answer.: : 1.C 2.D 3.A 4.B II. Fill in the blanks 1. Nissl body, neurofibril 2. axon, dendrite 3. multipolar neuron, bipolar neuron, pseudounipolar neuron 4. sensory neuron, motor neuron, interneuron 5. myelinated nerve fiber, unmyelinated nerve fiber 6. axon, myelin sheath, neurolemma 7. node of Ranvier 8. Schwann cells, oligodendrocyte 9. temperature, pain, touch, muscle length, deep or heavy pressure, vibration 10. presynaptic membrane, synaptic cleft, postsynaptic membrance 11. gap junction 12. astrocyte, oligodendrocyte, microglia, ependymal cell, capsular cell, Schwann cell 13. pia mater, arachnoid, dura mater III. Questions: 1. Describe the characteristics of nerve tissue. Components: • nerve cell: neuron, receive the stimulation, conduct the nerve impulse • Glial cell: neuroglia, support, protect and insulate, nourish neurons Function: • Transmit impulses and thus communicate with different parts of the body through these impulses. • Works closely with endocrine system in communication within the body. 2. Point out the different features of the structure both dendrite and axon. dendrites: ---short branches ---structure: similar to cell body ---dendritic spine: numerous fine projections (places for formation of synapse) ---function: receive the information from other nerve cells axon: ---longer and thinner process, have a uniform diameter ---structure: no Nissl body, but have microtubule, neurofilament, microfilament, mitochondria, SER and vesicle 3. Describe the structure and function of motor end-plate. LM: Plate-like mass with the terminal swelling of a nerve fiber EM • muscle F: rich in cytoplasm, nuclei and mito • presynaptic membrane: - synaptic vesicles- acetylcholine • synaptic cleft: • postsynaptic membrane: -acetylcholine receptor function: control the contraction of skeletal muscle fiber 4. Describe the structure of blood-brain barrier in detail. 1) The continuous endothelium of capillaries and the tight junctions between endothelial cell 2) a continuous basal membrane around the endothelium 3) The vascular foot processes of astrocytes surrounding the capillaries Function: Regulates the diffusion of many substances between the blood and brain 5. Describe the ultrastructure of Nissl body and neurofibril. a. Nissl body: Present throughout the cytoplasm of the cell body and dendrites, but absent from the axon hillock and axon LM: basophilic spot-liked or granule-liked structure EM: parallel-arranged RER and free ribosome b. neurofibril: LM: silver impregnation methods (silver preparation), thread-liked dark brown color fibril forming a network abundant in cell body, dendrites and axon EM: neurofilament: 10 nm in diameter microtubule: 25 nm in diameter Exercise 6 for histology (Cardiovascular system) I. Choice: Select the single most appropriate answer.: 1.D 2.E 3.D 4.B II. 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. fill in the blanks: heart, artery, vein, capillary lymph capillary, lymph vessel, lymph duct endothelial cell, basal lamina, connective tissue, pericyte continuous capillary, fenestrated capillary, sinusoid tunica intima, tunica media, tunica adventitia endothelium, subendothelial layer, internal elastic membrane smooth muscle cell medium-size artery, large artery endocardium, myocardium, epicardium, myocardium P-cells, transitional cells, Purkinje cells plasmalemmal vesicle, fenestrate pole, gap III. Questions: 1. Describe the ultrastructure and distribution of the 3 types of capillaries. Continuous capillary: -distributed in muscle tissue, brain, lung and connective tissue, etc. -endothelial cell: large number of pinocytotic vesicles, no pores, exist cell junctions between the endothelia -basal lamina: integrity Fenestrated capillary: -distributed in tissues where rapid interchange of substances occurs between the tissue and the blood, as in the kidney glomerulus, mucosa of gastrointestine, some endocrine glands -endothelial cells: present abundant pores, have or haven’t diaphragm on them -basal lamina: continuous Sinusoid: -distributed in tissues where interchange of substance in big size occurs, as in the liver, spleen, and some endocrine glands -a greatly enlarged diameter -endothelial cell: intercellular clefts are large between cells, many pores without diaphragm -absence of a continuous basement membrane -Macrophages are located either among or outside the cells of the endothelium 2. Compared the different structure between the artery and vein. -artery: The wall of Arteries consist of three layers or “coats” often referred to as tunics. a) Tunica itima – is the inner coat: 1) inner endothelial layer; 2) subendothelial layer: a layer of loose connective tissue ; 3) internal elastic membrane b) Tunica media – is the middle layer, This layer makes up the greatest part of the wall of the artery. It is comprised primarily of smooth muscle. In small arteries or arterioles it may be only 1-3 cells thick but in larger arteries may comprise hundreds of layers of muscle cells. In larger arteries, there in increased amounts of elastin fibers. c) Tunica adventitia or tunica externa is the outer layer of the wall of the blood vessel. It consists primarily of connective tissue and serves to attach the blood vessel into the surrounding connective tissue. Often contains adipose tissue and often contains blood vessels (vasa vasorum) that supply the walls of the blood vessels. Layers of arteries wall differ in different size blood vessels. The structure and function of arteries change as their diameter decreases. -vein: large lumen, thin wall, irregular internal and external elastic lamina are not clear tunica media is thin, with a few elastic fibers and smooth muscles tunica adventitia is thick many veins have valves 3. Compared the structure of medium-sized artery with that of small-sized and large artery. Medium-sized artery: muscular artery, diameter larger than 1mm, Tunica media: contain 10~40 layers of circular smooth muscle clear internal and external elastic membrane large artery: elastic artery, subendothelial layer is thicker with a few smooth muscles, tunica media is thick, contains a 40-70 concentrically- arranged elastic membrane, internal and external elastic lamina are not distinguished, tunica adventitia are thinner, abundant vasa vasorum. Small artery: muscular artery and peripheral resistance vessel, internal elastic lamina is clear, while external elastic lamina is not distinguished, the tunica media contains 3~9 layers of smooth muscles 4. Compared the structure between endocardium and epicardium. Endocardium: Endothelium Subendothelial layer: fined CT Subendocardial layer: LCT, blood vessels, nerves and the conducting system of the heart Epicardium: LCT: contain adipose cells, blood vessels and nerves Methothelium Exercise 7 for Histology (Immune system) I. Choice: Select the single most appropriate answer. 1.The source of T lymphocytes in peripheral lymphoid organ is derived from( A ) A. thymus B. tonsils C. lymph nodes D. bone marrow E. spleen 2. The afferent lymphatic vessels enter the parenchyma of lymph node from ( C ) A. hilum B. sinus C. capsule D. cortex E. medulla 3. The capsule of spleen is covered by ( E ) A. periosteum B. pericardium C. perimysium D. perineurium E. peritoneum 4. The place where the macrophages contact first with antigen in spleen is( D ) A. splenic cord B. splenic sinusoid C. splenic nodule D. marginal zone E. periarterial lymphatic sheath II. Fill in the blanks: 1. The central lymphoid organs include thymus and bone marrow . The peripheral lymphoid organs include lymph nodes , spleen and tonsils . 2. The main component of lymphoid organs are immune cells . They are composed of antigen-presenting cells , numerous lymphocytes and macrophages. 3. Each lobule of thymus has a peripheral zone of cortex and a central zone of medulla . 4. In the thymus, lymphocytes are also called thymocyte , the epithelial reticular cells can mainly secrete thymosin and thymopoietin to induce the division and differentiation of stem cells. 5. A characteristic feature of the thymus medulla is the prescence of thymic corpuscle which consist of concentric layers of medullary epithelial cell cells. 6. The blood-thymus barrier is formed by the following layers: non-fenestrated endothelium of the blood capillary wall, their basement membrane, a perivascular space containing some macrophages, the basal lamina of the epithelial reticular cells, and the processes of epithelial reticular cells . 7. The cortical region of lymph node is composed of superficial cortex , paracortical zone and cortical sinus . 8. The T lymphocytes are mainly found in the paracortical zone of lymph node and the periarterial sheaths of the white pulp of spleen. The B lymphocytes are mainly found in the lymphoid nodules of lymph node and splenic nodules of spleen. The T and B lymphocytes are found in medullary cord and splenic cord . 9. The post-capillary venules of lymph node may be found in paracortical zone and lined by thick endothelial cells. III. Questions: 1. Describe the characteristics of thymic cortex. The cortex is composed of an extensive population of T lymphocytes, dispersed epithelial reticular cells, and few macrophages. The epithelial reticular cells are stellate cells with light-staining oval nuclei. They are joined to similar adjacent cells by desmosomes between the ends of their processes. Some thymic epithelial cells with abundant cytoplasm are called nurse cells, which nurture thymocytes by secreting thymosin and thymopoietin necessary for thymocytic development. Thymocytes are early-staged immature T lymphocytes, and are densely located in the cortex, representing 85-90% of the cells in the cortex. Because of the proliferation of lymphocytes in the cortex, immature T lymphocytes are produced in quantity and accumulate in this region. Although most of these lymphocytes (95%) undergo apoptosis in the cortex and are removed by macrophages, a small number (5%) of them migrate to the medulla and enter into the bloodstream through the wall of venules. These cells migrate to nonthymic lymphatic structures and accumulate in specific sites as T lymphocytes. 2. Compare the structures of medullary region of lymph node with that of red pulp of spleen. The structure of medullary region: The medulla is composed of the medullary cords, cord-like, branched extensions of the inner cortex, that contain B lymphocytes and numerous plasma cells. The medullary cords are separated by dilated, capillary-like structures called medullary lymphatic sinuses. These are irregular spaces containing lymph; like the subcapsular and intermediate sinuses, they are partially lined by reticular cells and macrophages. Macrophages, concentrated in this area, work to cleanse the lymph. Reticular cells and fibers frequently bridge the sinus with a loose network. Large branched dendritic (follicular) cells are found in the lymph nodes and function as antigen-presenting. The structure of red pulp of spleen: The red pulp is composed of the splenic cords and the splenic sinus with a reticular tissue. The splenic cords lie between the sinusoids. In addition to reticular cells and fibers, the splenic cords contain plentiful macrophages, lymphocytes, plasma cells, and many blood elements (erythrocytes, platelets, and granulocytes). The sinusoids occupy the area between the red pulp cords. The sinusoidal endothelium is formed by fenestrated flattened cells with long axes parallel to the long axes of the sinusoids, which permit easy communication between its interior and the red pulp. The transverse and longitudinal fibers join with each other to form a network enveloping the sinusoid cells and macrophages that occupy the spaces between neighboring endothelial cells. Because the spaces between cells of the splenic sinusoids are 23 μm in diameter or smaller, only flexible cells are able to pass easily from the red pulp cords to the lumen of the sinusoids. 3. Describe the recirculation of lymphocytes. *Recirculation of LC: LC(blood) →(postcapillary venules) → LN → medulla → efferent LV → Blood →LN artery → postcapillary venules →LN Function: a.Filter the lymph; b.Place to give rise to the immune response; c. Involve in the recirculation of LC 4. Describe the blood circulation in spleen. splenic A→trabecular A→central A branches → marginal sinuses penicillar Arterioles(including: pulp arteriole→ sheathed capillary→ arterial capillary) → splenic sinus→ pulp venule→ trabecular vein→ splenic vein Exercies 8 for Histology (Skin) I. Choice: Select the single most appropriate answer. 1. Which function of skin is incorrect in following contents ( D ) A. protect the human body B. prevent the invasion from bacteria etc. C. sensory organ D. store and supply energy E. excrete water and some waste products 2. Nonkeratinocytes include ( E ) A. monocytes, Langerhans cells and Merkel cells B. melanocytes, islets of langerhans and Merkel cells C. basal cells, spinous cells and granular cells D. spinous cells, granular cells and horney cells E. melanocytes, Langerhans cells and Merkel cells 3. Racial differences in skin color are due to differences in the number and size of ( E ) A. melanosome B. melanocyte C. melanophore D. Langerhans cell E. melanin granule 4. Sweat glands are most numerous in the ( A ) A. palms and soles B. palm and axilla C. axilla and areola of the nipple D. sole and labia majora E. epidermis and dermis II. Fill in the blanks: 1. The skin consists of 2 layers: a superficial layer of epithelium called epidermis and a deep layer of connective tissue called dermis . 2. The epidermis is composed of stratified squamous keratinized epithelium; The dermis is mainly composed of loose and dense connective tissue. 3. The melanocytes are lack of bundles of keratin filaments in the cytoplasm, but have numerous ovoid melanosome and melanin granule with melanin. 4. The Langerhans cells have an lobulated nucleus and present more processes and characteristic racket-shape Birbeck granules in their cytoplasm. 5. The dermis consists of papillary layer and reticular layer. The subcutaneous tissue is composed of loose connective tissue , and contains more fat cells . 6. The skin appendages include hairs , sebaceous gland , sweat gland , nails and mammary gland. 7. Each hair root is surrounded by hair follicle , it is expanded into a hair bulb . The base of it is invaginated by connective tissue which called hair papilla . Arrector pili muscle is attached at one end to the connective tissue sheath of the follicle and at the other to the papillary layer of the dermis. 8. The cells of the sebaceous acini are small, undifferentiated flattened epithelial cells in outer layer and large rounded cells in center. They contain abundant fat droplets in their cytoplasm. The products of secretion are sebum, a complex mixture of lipid . III. Questions: 1. Describe simply the strata and histologic features of the epidermis of palms or soles. The epidermis consists mainly of a stratified squamous keratinized epithelium, but it also contains three less abundant cell types: melanocytes, Langerhans' cells, and Merkels cells. The keratinizing epidermal cells are called keratinocytes. It is customary to distinguish between the thick skin (glabrous, or smooth and non-hairy) found on the palms and soles and the thin skin (hairy) found elsewhere on the body. The thickness of the epidermal layer varies between 75 and 150 μm for thin skin and 400 and 600 μm for thick skin according to site. From the dermis outward, the epidermis consists of five layers of keratin-producing cells: Stratum Basale, Stratum Spinosum, Stratum Granulosum, Stratum Lucidum, Stratum Corneum. 2. Please explain the formed factors of cutaneous pigmentation. The color of the skin is the result of several factors, the most important of which are its content of melanin and carotene , the number of blood vessels in the dermis, and the color of the blood flowing in them. Melanocytes are derived from neural crest cells. They have rounded cell bodies from which long irregular extensions branch into the epidermis, running between the cells of the basal and spinosum layers. The electron microscope reveals a pale-staining cell containing numerous small mitochondria, a well-developed Golgi complex, and short cisternae of RER. Intermediate filaments, about 10 nm in diameter, and melanosomes are also present. Tyrosinase is synthesized in the RER and accumulated in vesicles of the Golgi complex. The free vesicles are melanosomes. While melanocytes are not attached to the adjacent keratinocytes by desmosomes, hemidesmosomes bind melanocytes to the basal lamina. Although melanocytes synthesize melanin, epithelial cells act as a depot and contain more of this pigment than melanocytes. A feedback mechanism of the transfer of the granules into the keratinocytes may exist between melanocytes and keratinocytes. Exercise 9 for Histology (Endocrine system) I. Choice: Select the single most appropriate answer. 1. Neural stalk in hypophysis is composed of ( E ) A. pars distalis and pars tuberalis B. pars nervosa and pars intermedia C. pars tuberalis and pars intermedia D. pars nervosa and median eminence E. infundibular stem and median eminence 2. Which results is not followed by hypophysectomy in following( E ) A. cessation of bone growth B. atrophy of thyroid C. atrophy of sex organs D. atrophy of suprarenal cortex E. increasing in the percentage of basophils 3. In pars nervosa of hypophysis, Herring bodies are composed of ( A ) A. groups of neurosecretory granules B. neuroglial cell C. dendrite of neuron D. dendrite of neuron E. axon of neuron 4. On electron microscopy, the most characteristic feature of component cells of the zona fasciculata is ( D ) A. numerous SER and RER B. well-developed RER and numerous mitochondria C. well-developed SER and numerous mitochondria D. well-developed SER and numerous mitochondria with tubular cristae and lipid droplets E. well-developed RER and numerous mitochondria with tubular cristae and lipid droplets II. Fill in the blanks: 1. Hypophysis is derived from two different tissues: The adenohypophysis is derived from ectoderm at the roof of the oral cavity of the embryo ; The neurohypophysis is derived from the floor of the diencephalons . 2. There are three types of cells in the pars distalis of pituitary gland: acidophils, basophils and chromophobe . 3. According to produced hormones, the acidophils of hypophysis are subdivided into two types of cells: somatrophs and mamotrophs . 4. According to produced hormones, the basophils of hypophysis are subdivided into three types of cells: thyrotroph , gonadotroph and corticotroph . 5. In the pars distalis of hypophysis, the cells with the largest number are chromophobe cell; the cells with the largest granules are acidophils the cells with the smalles granules are basophils . 6. In the pars distalis of hypophysis, somatotrophs secrete growth hormones (STH); mammotrophs secrete prolactin hormones (LTH); thyrotrophs secrete thyroid stimulating hormones (TSH), luteinizing hormones (LH) and interstitial cell stimulating hormones (ICSH) and corticotrophs secrete adrenocorticotropin hormones (ACTH). 7. Herring bodies contain two hormones: antidiuretic hormone (ADH) which is synthesized by the supraoptic nucleus and oxytocin which is synthesized by the paraventricular nucleus. 8. In amphibia, the pars intermedia is well developed and produces melanocyte stimulating hormone (MSH) which is a polypeptide that is produced by melanotroph cells. 9. In clinics, oversecretion of somatotropin causes gigantism in children and acromegaly in adults. Undersecretion of growth hormone leads to dwarfism in childhood. 10. The adrenal cortex may be divided into three zones: (1). Zona glomerulosa Which secretes mineralocorticoid , such as aldosterone that maintain electrolyte and water balance; (2). Zona fasciculata which secretes glucocorticoid , such as cortisol and corticosterone which effect on the glucose metabolism and the inflammations reactions and stress management. 11. The structure of medulla of adrenal gland includes groups of granular cells, sinus and connective tissue . 12. The medullary parenchymal cells of adrenal medulla is polygonal in shape. They contain two kinds of different secreting granules; adrenaline and noradrenaline . 13. The adrenal cortex is derived from mesoderm and the adrenal medulla is derive from ectoderm . III. Questions: 1. Write the component of hypophysis by list. The hypophysis, is a small but complex endocrine organ. the hypophysis consists of two different tissues: adenohypophysis and neurohypophysis. The adenohypophysis develops from the ectoderm at the roof of the oral cavity of the embryo. The neurohypophysis (nervous portion) is derived from an outgrowth of the floor of the diencephalons. The adenohypophysis is divided into three unequal parts, the pars distalis, the pars intermedia, and the pars tuberalis. The pars distalis is anterior to the lumen, and the pars intermedia is posterior to the lumen. The pars tuberalis is an extension of the pars distalis, enveloping the neural stalk. The neurohypophysis is also composed of two portions: pars nervosa and infundibulum. The pars infundibulum, consisting of infundibulum stem and median eminence, is connected to hypothalamus. The pars nervosa is the major portion; it lies immediately behind the pars intermedia. The pars nervosa is continuous, with the infundibulum and median eminence. The pars tuberalis and infundibulum form the hypophyseal stalk. The term anterior lobe refers to the pars distalis, and the posterior lobe refers to the pars nervosa and the pars intermedia. 2. Describe the blood supply of the hypophysis and their significance. The blood supply of the hypophysis derives from two groups of blood vessels that come from the internal carotid artery. The right and left superior hypophyseal arteries supply the median eminence and the neural stalk; from below, the right and left inferior hypophyseal arteries provide blood mainly for the neurohypophysis, with a small supply to the stalk. The superior hypophyseal arteries form a primary capillary plexus of fenestrated capillaries that irrigate the stalk and median eminence. They then rejoin to form several hypophysis portal venules, which then develop a secondary plexus in the adenohypophysis. The primary and secondary capillary and the hypophysis portal venules constitute the so-called hypophyseal portal system. This hypophyseal portal system is of utmost importance in regulating hypophyseal function: it carries neurohormones from the median eminence and hypothalamus to the adenohypophysis. 3. Compare the structure and function of the zona glomerulosa with that of the zona fasciculata in adrenal cortex. The zona glomerulosa located immediately beneath the capsule, is composed of cuboidal, columnar, or pyramidal cells arranged in irregular, ovoid clumps, surrounded by delicate connective tissue containing capillaries. Some clumps show central lumina, similar to the acini in other kinds of glands. The cells have darkly stained spherical nuclei and slightly basophilic cytoplasm. The zona glomerulosa produces mineralocorticoids (principally aldosterone), which control water and electrolyte balance by the regulation of the sodium and potassium ion level. The secretion of aldosterone is independent of ACTH. The zona fasciculate is the intermediate and thickest layer of the three zones of the cortex. It is composed of large, polyhedral cells arranged in long, radial cords usually two cells wide. These cords are perpendicular to the surface of the gland, and separated from one another by parallel capillaries. The secretory cells have round, centrally located nuclei and pale-stained cytoplasm filled with 1ipid droplets that give rise to the characteristic foamy appearance of the cells. The zona fasciculata secretes glucocorticoids (hydrocortisone and cortisone). Secretion of this class of hormones is controlled by the hypothalamus via the anterior pituitary hormone ACTH. Glucocorticoids have wide-ranging effects, such as those on the metabolism of carbohydrates, proteins, and lipids, as well as on suppressing the immune response. Excercise 10 for Histology (Digestive tract) 1. Choice: Select the single most appropriate answer. 1. The adventitia of esophagus is ( C ) A. mucosa B. mesothelium C. fibrosa D. Serosa E. capsule 2. The location of synthesizing hydrochloric acid in parietal cells of gastric gland is in ( E ) A. tubulovesicular system B. RER C. pinocytotic vesicles D. Golgi complex E. surface of intracellular canaliculi 3. The intrinsic factor which aids vitamin B12 absorption is secreted by (B ) A. chief cell B. parietal cell C. mucous neck cell D. enteroendocrine cell E. gastric epithelial cell 4. Which structure of appendix is incorrect in following contents.( C ) A. without goblet cells B. villi are absent C. incomplete epithelium D. less and short intestinal glands E. a mass of lymphoid mass II. Fill in the blanks: 1. There are esophageal glands or duodenum glands in the submucosa of the digestive tract. 2. In the middle third muscular layer of esophagus consists of skeletal muscles and smooth muscles. 3. The epithelium of stomach is simple columnar epithelium. The neutral glycoprotein mucus secreted by these epithelial cells protects the gastric mucosa. 4. The gastric glands are composed of parietal cells , chief cells, mucous neck cells, stem cells and enteroendocrine cells . These glands open into the bottom of the gastric pit . 5. The cardiac glands and pyloric glands in stomach are branched tubular glands, they are distributed in the laminar propria of cardia and pylorus . 6. In the cytoplasm of parietal cells there are an abundance mitochondria and the apical plasma membrane forms the intracellular secretory canaliculi . 7. The three special structures to increase the surface areas of absorption in the small intestine are Plicae circulates , intestinal villi and microvilli . 8. The cell coat on the microvilli of columnar cell surface of small intestinal epithelium contains enzyme , including disaccharidase and peptidase , trypsin and amylopsin to help digestion. 9. The intestinal glands of small intestine consist of five types of cells: absorptive cell , goblet cell , paneth’s cell , stem cell and endocrine cell . 10. The duodenal glands (Brunner’s ) are of compound tubular submucosal type. The product of its secretion is to neutralize the acid gastric juice. 11. In the adult, amino acids and glucoses are absorbed by the fenestrated capillary and enter the blood ; The micelles of fatty acids and monoglycerides are absorbed by the central lacteal and enter the lymph system . 12. The general structure of the digestive tract may be divided into 4 layers from the inner to the outer: mucosa , submucosa , muscularis and adventitia . 13. The muscularis externa intestinal tract is composed of smooth muscle arranged in an inner circular and an outer longitudinal layer. Between these two layers are a vascular vessels and myenteric nerve plexus. 14. Adventitia of digestive tract is composed of fibrosa or serosa . III. Questions: 1. Compare the mucosal structure of stomach with that of esophagus, small intestine and large intestine. Stomach: The gastric mucosa consists of a surface epithelium that invaginates to varying extents into the lamina propria, forming about 350 gastric pits. Emptying into each gastric pit is 3-5 branched, tubular glands characteristic of each region of the stomach. Esophagus: The mucosa is in turn composed of three layers: an epithelial lining formed by nonkeratinized stratified squamous epithelium, the lamina propria, and the muscularis mucosae. The esophagocardiac junction shows an abrupt transition from the stratified squamous epithelium of the esophagus into simple columnar epithelium of the cardiac area of the stomach. The lamina propria, muscularis mucosae, and submucosa in the esophagus are continuous with those in the cardia. The lamina propria of the esophagus contains lymphatic tissue, whereas the lamina propria of the cardia shows numerous blood vessels, plasma cells, and macrophages. Diffuse lymphatic tissue is often seen in the lamina propria. Small intestine: The small intestine is relatively long-approximately 5m, permitting enough time for the contact between food and digestive enzymes, as well as between the digested products and the absorptive cells of the epithelial lining. The lining of the small intestine shows a series of permanent folds, plicae circulates, consisting of mucosa and submucosa and having a semilunar, circular, or spiral form. The plicae are most developed in the end of duodenum and the beginning of the jejunum. Then, they become shorter and fewer, and disappear from the middle of ileum. Intestinal villi are seen under magnification. These structures, 0.5-l.5 mm long, are outgrowths of the mucosa (epithelium plus lamina propria) projecting into the lumen of the small intestine. They are more abundant in duodenum and the beginning of jejunum. In the duodenum they are leaf shaped, gradually assuming finger-like shapes as they reach the ileum. Between the villi are small openings of simple tubular glands called intestinal glands, or glands of Lieberkdhn in the lamina propria. They open directly into the intestinal cavity. Large intestine: The large intestine consists of a smooth mucosal membrane with no permanent plicae circulares or villi as seen in the mucosa of the small intestine. The mucosa is characterized by the presence of the mucosal glands. The lamina propria is rich in lymphatic cells and in solitary lymphoid nodules that frequently extend into the submucosa. This richness in lymphatic tissue is probably the result of the extremely abundant bacterial population of the large intestine. The muscularis comprises longitudinal and circular strands. This layer differs here from that of the small intestine, since fibers of the outer longitudinal layer congregate in three thick longitudinal bands called teniae coli. In the anal region, the mucous membrane forms a series of longitudinal folds. About 2 cm above the anal opening, the intestinal mucosa is replaced by stratified squamous epithelium. In this region, the lamina propria contains a plexus of large veins that, when excessively dilated and varicose, produce hemorrhoids. Epithelial cells of the large intestine are replaced about every 6 days by the proliferation and differentiation of stem cells in the bottom third of the glands. 2. Describe the fine structure and ultra-structure of the parietal cell and chief cell in the gastric gland. Chief cells, predominate in the fundus of the gland and intermingle with parietal and mucous neck cells toward the neck region. They are low columnar cells and have the typically histological characteristics of protein-producing cells, with a spherical nucleus located toward the base, basophilic basal cytoplasm due to the abundant rough endoplasmic reticulum, and apical cytoplasm filled with acidophilic zymogen granules. Parietal cells are located mainly in the isthmus and neck regions, but are also scattered in the fundic region. Characteristically they are large, rounded, or pyramidal cells with central spherical nuclei and extensive eosinophilic cytoplasm. The most striking features seen in the electron microscope are an abundance of mitochondria, intracellular secretory canaliculi, deep circular invaginations of the luminal surface with associated microvilli; and tubulovesicular system. 3. Describe the different formation of villi and plicae in small intestine. The lining of the small intestine shows a series of permanent folds, plicae circulates, consisting of mucosa and submucosa and having a semilunar, circular, or spiral form. The plicae are most developed in the end of duodenum and the beginning of the jejunum. Then, they become shorter and fewer, and disappear from the middle of ileum. Intestinal villi are seen under magnification. These structures, 0.5-l.5 mm long, are outgrowths of the mucosa (epithelium plus lamina propria) projecting into the lumen of the small intestine. They are more abundant in duodenum and the beginning of jejunum. In the duodenum they are leaf shaped, gradually assuming finger-like shapes as they reach the ileum. 4. Describe the structure of mucosa of the digestive tract. The mucosa (mucous membrane layer), the most important layer of the tract, consists of an epithelial lining, supported by connective tissue call a lamina propria, and surrounded by a thin layer of smooth muscle called the muscularis mucosae. The structures vary largely with the sites where they locate. The epithelial type varies with the site where it locates. At the two ends of digestive tract, the epithelium is stratified squmous epithelium, protecting the epithelium from various injuries. The others belong to simple columnar epithelium with a strong absorptive activiy. The epithelium may contain glandular epithelial cells that secret digestive enzymes and goblet cells that secret mucus. The epithelium always connects itself with the glands within the dissepiment. The main functions of the epithelial lining of the digestive tract are to provide a selectively permeable barrier between the contents of the tract and the tissues of the body, to facilitate the transport and digestion of food, to promote the absorption of the products of this digestion, and to produce hormones that affect the activity of the digestive system. Cells in this layer produce mucus for lubrication and protection. The lamina propria consists of loose connective tissue rich in blood and lymph vessels and smooth muscle cells, sometimes also containing glands and lymphatic tissue. This layer is a zone rich in macrophages and lymphoid cells, some of which actively produce antibodies. These antibodies are mainly immunoglobulin A (IgA) and are bound to a secretory protein (S) produced by the epithelial cells of the intestinal lining and are secreted into the intestinal lumen, SIgA. This complex provides a protective activity against viral and bacterial invasion. The muscularis mucosae is a thin inner circular layer and an outer longitudinal layer of smooth muscle cells separating the mucosa from the submucosa. The contraction of this layer helps to expel the glandular productions from the acini, and to facilitate the blood circulation and food absorption and transportation Exercise 11 for Histology (Digestive gland) I. Choice: Select the single most appropriate answer. 1. The B cells in islet of Langerhans secrete ( B ) A. glucagon B. insulin C. serotonin D. pepsin E. trypsin 2. Vasoactive intestinal peptide and pancreatic polypeptid are secreted by ( E ) A. A cell B. B cell C. C cell D. D cell E. PP cell 3. The perisinusoidal space ( space of Disse ) in hepatic lobule is located between ( C ) A. two adjacent hepatocytes B. hepatic macrophage and endothelium of hepatic sinusoid C. hepatocyte and endothelium of hepatic sinusoid D. hepatic plate and hepatic plate E. fat-storing cell and endothelium of hepatic sinusoid 4. The organelles in hepatocyte which possess detoxification which some drugs can be inactivated are ( E ) A. microbodies B. mitochondria C. Golgi complex D. Lysosome E. SER 5. The A cells in islet of Langerhans secrete ( D ) A. trypsin B. pepsin C. serotonin D. Glucagon E. insulin II. Fill in the blanks: 1. They are serous acini in the exocrine portion of pancreas. The zymogen granules present in cytoplasma of cells. 2. Each portal space contains a interlobular veins , an interlobular arteries , interlobular bile duct and lymphatic vessels. 3. Bile canaliculi are tiny cavities limited by only the plasma membrane of two adjacent hepatocytes. The junctions of them with bile duct in a portal space are called intralobular duct . The cell membranes near these bile canaliculi are firmly joined by tight junction and desmosome . 4. The hepatic sinusoid are the spaces between the hepatic plates. They contain kupffer cells and NK cells. 5. The ultrastructures of cytoplasm of Kupffer cells contain prominent lysosomes , many pinosomes and well developed phagososmes . 6. Spaces of Disse is a narrow space. There are many microvilli on the surface of the hepatocyte. The space contains fat-storing cells, which contain vitamin A-rich lipid inclusions. 7. There are three hepatic functional surfaces: the face adjacent cell each other , face the sinusoid and face bile canaliculus surfaces. 8. The functions of liver include: (1). Synthesize proteins by ribosome and RER , (2). Synthesize bile acid by Golgi complex , (3). Detoxification by SER of hepatocyte, (4), Phagocytosis by lysosome and so on. 9. The major salivary glands are composed of secretory portion and duct portion . 10. Ducts of the major salivary glands are subdivided into intercalated ducts, intralobular duct and interlobular duct . 11. They are pure serous acini in the parotid gland. Most of acini are mixed in the submandibular. The majority of acini are mucous in the sublingual glands. III. Questions: 1. What are the structures and functions of islets of Langerhans. The pancreas islets of Langerhans are multihormonal endocrine microorgans of the pancreas; they appear as rounded clusters of endocrine cells embedded within exocrine pancreatic tissue. They are pale-stained in HE sections, and are extremely different from the exocrine portion. There may be more than l million islets in the human pancreas, with a slight tendency for islets to be more abundant in the tail region. While most islets are 75-500 mm in diameter and contain several hundred endocrine cells, small islets of endocrine cells can also be found interspersed among pancreatic exocrine cells. Each islet consists of lightly stained polygonal or rounded cells arranged in cords separated by a network of fenestrated blood capillaries. Both the parenchymal cells and the blood vessels are innervated by autonomic nerve fibers. A fine capsule of reticular fibers surrounds each islet, separating it from the adjacent exocrine pancreatic tissue. Using immunocytochemical methods, four types of cells--A, B, D, and PP--have been located in the islets. The secretory granules of these cells vary according to the species studied. In humans, the A cells have regular granules with a dense core surrounded by a clear region bounded by a membrane. The B cells have irregular granules with a core formed by irregular crystals of insulin complexed with zinc. The relative quantities of the four cell types found in islets are not uniform; they vary considerably with their location in the pancreas. The following table summarizes the types, quantities, and functions of the hormones produced by the islet cells. The ultrastructure of these cells resembles that of cells synthesizing polypeptides. 2. Describe the ultra-structures and functions of hepatocytes in detail. The Hepatocyte Liver cells, making up 97% of total cells in the liver, are polyhedral, with six or more surfaces, and have a diameter of 15-30 mm. In sections stained with hematoxylin and eosin, the cytoplasm of the hepatocyte is eosinophilic. The liver cell has one or two rounded nuclei with one or two typical nucleoli. The hepatocyte has an extremly abundant organells including endoplasmic reticulum--both smooth and rough, mitochondria, Golgi complexes, Hepatocyte lysosomes, Peroxisomes. In addition, it contains glycogen. Another common cellular component is the lipid droplet, whose numbers vary greatly. Functions of the Liver Cell The liver cell probably is the most versatile cell in the body. It is a cell with both endocrine and exocrine functions; it also synthesizes, or accumulates, or detoxifies, or transports certain substances. 3. Describe the structures of the liver lobule. The hepatic lobule (liver lobule) serves as the structural and functional unit of the liver. It is a polygonal prism in shape measuring about 2 mm in size, and usually appears hexagonal in cross section, although this is difficult to see in human liver. One adult liver has about 500,000-1,000,000 hepatic lobules. Each hepatic lobule has a central vein in the middle, with hepatic plates or cords radiating from it to the periphery like the spokes of a wheel from a central hub中芯. The human liver has a structural pattern of lobules similar to that of pig liver, but human hepatic lobules are not compartmentalized by distinct connective tissue of the interlobular septa. The organization of pig liver makes it ideal for understanding the concept of the hepatic lobule. The hepatic plate consists of a single layer of parenchymal cells called the hepatocytes, anastomosing with one another to form a network in three dimensions. Between the eosinophilic hepatic plates (also called hepatic cords) are sinusoids filled with blood and phagocytic cells. Under higher magnification, very thin holes or canals between hepatocytes can be observed. These are the bile canaliculi, l-2 mm in diameter, formed by the invagination of the junctional membranes of hepatic cells. Thus, hepatic plates, hepatic sinusoids, and bile canaliculiunitedly form a both complex and closely associated network. 4. Describe the blood circulation of liver. The liver is unusual in that it receives blood from two sources: 80% of the blood derives from the portal vein that carries oxygen-poor but nutrient-rich blood from the abdominal viscera; and 20% from the hepatic artery that supplies oxygen-rich blood. Exercise 12 for Histology (Respiratory system) I. Choice: Select the single most appropriate answer. 1. The small granular cells of respiratory epithelium constitute ( D ) A. immune system B. nervous system C. endocrine system D. neuroendocrine system E. sensory system 2. The basic unit of the lung is lung lobule which is formed by ( E ) A. alveoli B. alveolar duct C. respiratory bronchiole and its tributaries D. terminal bronchiole and its tributaries E. bronchiole and its tributaries 3. When a bronchiole is obstructed, which structure may equalize pressure in the alveoli are make possible collateral circulation of air. ( D ) A. alveolar septa B. intercellular space C. alveolar sac D. Alveolar pore E. endothelium of capillary 4. Nonciliated cells of terminal bronchioles are ( B ) A. goblet cells B. Clara cells C. brush cells D. basal cells E. small granule cells II. Fill in the blanks: 1. The main functions of respiratory system are gas exchange . The respiratory system includes a conducting portion and a respiratory portion . 2. From the inner to the outer, the trachea is composed of the mucosa, submucosa and adventitia .The C-shaped hyaline cartilage is located in adventitia . 3. There are numerous bundles of smooth muscles , connective tissue and abundant glands in portion of membranous wall of trachea, but there is no hyaline cartilage . 4. The typical respiratory epithelium is composed of pseudostratified ciliated columnar epithelium.They include five cell types: ciliated columnar cell , goblet cell , brush cell , small granule cell , and basal cell . 5. The conducting portion of lung consists of small bronchus, bronchiole and terminal bronchiole . 6. The respiratory portion of lung consists of respiratory bronchiole , alveolar duct , alveolar sac and alveoli . 7. A lung lobule is pyramid in shape with the apex directed toward the the pulmonary hilum . 8. The structure of the discontinuous wall of alveolar duct composed of simple cuboidal epithelium, thin layer of smooth muscle fibers and collagenous fibers and elastic fibers. The wall appear as knob-like structure between adjacent alveoli. 9. There are two types of alveolar epithelium: type I alveolar cell is also named squamous alveolar cell; type II alveolar cell is the great alveolar II cell. In the cytoplasm of type II alveolar cells it contains many osmiophilic multi-lamellar body giving rise to surfactant . 10. The interalveolar septum is the connective tissue between the neighbouring alveoli, within this thin wall there are abundant alveolar capillaries , elastic fiber and reticular fiber and so on. 11. Surfactant may aid in reducing the surface tension of the alveolar cells and stabilizing the shape of the alveoli. 12. There are two kinds of macrophages of lung: dust cell and heart failure cell . III. Questions: 1. Compare the structure of bronchiole with that of terminal bronchiole. A bronchiole, with a diameter of 0.5-1 mm, supplies a single lobule. Its lumen is lined by a lower ciliated pseudostratified columnar epithelium or simple ciliated columnar epithelium with the progressive decrease of goblet cells. The basement membrane becomes thinner. The cartilage and glands decrease or are absent. The prominent bundles of smooth muscle and elastic fibers comprise the lamina propria, supporting the wall of the bronchiole. Also seen in the wall of the bronchiole are blood vessels and nerve fibers. The mucosal folds appear processing into the lumen. The terminal bronchioles are the thin-walled branches of the bronchiole, 0.5mm in diameter. The epithelium becomes ciliated simple columnar type, without goblet cells. The cartilage and glands completely disappear. The connective tissue is much reduced, and the smooth muscle fibers form a complete layer encircling the lumen. The terminal bronchiole gives rise to respiratory bronchioles. The folds are more significant. 2. Describe the morphology and function of type I cell and type II cell in lung in detail. Type I alveolar cells: also called squamous alveolar cells, are extremely flattened cells that line the alveolar surfaces and attenuated cytoplasm about 50-100mm wide, about 0.2mm thick. Under electron microscope, organelles such as the Golgi complex, endoplasmic reticulum, and mitochondria are grouped around the nucleus. The cytoplasm in the thin portion contains abundant pinocytotic vesicles, which may play a role in the turnover of surfactant and the removal of small particulate contaminants from the outer surface. In addition to desmosomes, all type I epithelial cells have occluding junctions that serve to prevent the leakage of tissue fluid into the alveolar air space. They lack the ability of proliferation so type II cells are needed when injuried. Type II alveolar cells: the great alveolar cellsⅡ, are scattered singly or are present in a small group among the squamous alveolar cells. They are roughly small cuboidal or rounded with a large rounded nucleus, and rest on a basement membrane. At the electron microscopic level, they have mitochondria, rough endoplasmic reticulum, a well-developed Golgi complex, and microvilli on their free apical surfaces. These cells are characterized by multilamellar bodies within its cytoplasm. Surfactant may aid in reducing the surface tension of the alveolar cells and stabilizing the shape of the alveoli. 3. What is the air-blood barrier (or respiratory memebrane) composed of? The structures through which gaseous exchange occurs between air in alveoli and blood in alveolar capillaries are known collectively as the blood-air barrier. These structures, measuring about 0.2-0.5 mm in thickness, include three components. (1)The surface lining of surfactant secreted by the type II cells; (2) The attenuated cytoplasm of pulmonary epithelial cells (type I cells) and the basement membrane of the epithelium; a thin layer of connective tissue; (3) The basement membrane of the capillary; and the very thin cytoplasm of capillary endothelial cells. To reduce the thickness of the blood-air barrier, the two basement membranes are generally fused into one layer. Oxygen from the alveolar air passes into the capillary blood through these layers; CO2 diffuses in the opposite direction. Exercise 13 for histology (Urinary and endocrine system) I.Choice: Select the single most appropriate answer: 1. The structural and functional units for urine secretion in kidney are ( C ) A. renal corpuscle B. filtration barrier C. nephron D. collecting tubule E. uriniferous tubule 2. In two kidneys of adult, the total glomerular filtrate (primary urine) in per minute produce about (B) A. 124ul B. 125ml C. 124L D. 125L E. 1500ml 3. The epithelium of thin segment in nephron is ( A) A. simple squamous epithelium B. simple cuboidal epithelium C. simple columnar epithelium D. transitional epithelium E. stratified squamous epithelium 4. In kidney the prostaglandin is secreted by (B) A. podocyte B. interstitial cell C. juxtaglomerular cell D. collecting tubule E. extraglomerular mesangial cell 5.Parafollicular cells in thyroid gland are able to produce ( D) A. rennin B. erythropoietin C. thyroxine D. calcitonin E. prostaglandin 6. The epithelial cells in parathyroid gland are of two types ( C ) A. chief cells and parietal cells B. follicular cells and parietal cells C. chief cells and oxyphil cells D. follicular cells and oxyphil cells E. alpha cells and beta cells II. Fill in the blanks: 1. The parenchyma of kidney may be divided into outer cortex and an inner medulla 2. The renal medulla is composed of 10-18 pyramid-shaped structures, called medullary pyramids , and a lot of elongated parallel arrays of tubules penetrate the cortex, called medullary rays . 3. The cortical labyrinth consists mainly of cortex . A renal lobule consists of 1/2 cortical labyrinth + single medullary ray +1/2 cortical labyrinth . 4. Each nephron is composed of two portions: (1). Renal corpuscle , and (2). Renal tubules . . 5. The collecting tubules are lined with simple cuboidal or columnar epithelium. The cells are pale-staining and the cellular border of two adjacent cells are clearly visible. They are under the control of the aldosterone and ADH . 6. The primary urine is formed in the space of Bowman space , through reabsorption, secreting and concentration of renal tubules to form terminal urine which volume is 1% of the primary urine. 7. The juxtaglomerular apparatus consist of juxtaglomerular cells , Macula densa cells and extraglomerular mesangial cells . 8. The intraglomerular mesangial cells are located among glomerular capillaries , they have receptors for angiotensin II . The extraglomerular mesangial cells are located outside the renal corpuscle in the vascular pole. 9. The main function of distal convoluted tubule in kidney is in the elimination of wasted materials such as hydrogen and ammonium ions , as well as maintain the acid-base balance balance. 10. In the endocrine system, hormones differ greatly in their chemical composition : some are Amnio acid-based hormones ; others are steroids hormones . 11. Thyroxine increases basal metabolic rate, hypothyroidism in the fetal life influence body growth and development of the nervous system . III. Questions: 1. Describe the fine structure of renal corpuscle in detail. glomerulus: fenestrated capillaries, mesangial cells, mesangial matrix Bowman space: Bowman capsule: parietal layer: simple squamous epithelium Visceral layer: podocytes 2. Filtration barrier of kidney: fenestrated endothelium, basal lamina, filtration slits 3. Compare the structures and functions of the proximal convoluted tubule with that of distal convoluted tubule. Proximal Acidophilic Limit of cell Wall Lumen Brush border Distal strong obscure thick irregular + less strong clear thin regular - Function: Proximal: 1) resorbs all of the glucose, amino acids and at least 85% of the sodium chloride and water 2) secretes creatinine and certain foreign substances into the filtrate Distal: 1) Straight portion—establish a gradient of osmolarity in the medulla 2) Convoluted portion—resorbs Na+,H2O transfers K+, This process is stimulated by aldosterone and ADH 4. Compare the structure and function of the juxtaglomerular cells with that of the macula densa. JG cells a. Modified smooth muscle cells b. Are located primarily in the wall of afferent arterioles c. Synthesize renin Macula densa cells a. tall, narrow,closely packed epi.cells of the distal tubule b. elongated, closely packed nuclei (macula densa) c. monitor the osmolarity and volumn of the distal tubule and transmit infromation via gap junction 5. Describe the blood supply of the kidney. (1)extensive, 1200ml/min (2)glomerular Cap. and peritubular Cap. network (3)Vasa recta associated with the Henle loops 6. Which structural characteristics are there in the wall of urinary bladder? Mucosa:transitional epi.+lamina propria Muscularies:smooth muscle Serosa and apical adventitia 7. How do the thyroid follicular epithelial cells synthesize thyroglobulin and release thyrosine? (1) (2) (3) (4) (5) (6) (7) Synthesis of thyroglobulin (TG) from tyrosine Glycosylated by Golgi complex, Secreted into the lumen and iodinated TSH stimulates endocytosis of iodinated TG by follicular cells Lysosomes fuse with the endosomes Proteases cleave off the iodinated residues to form T4 (~90%) and T3 (~10%) T3 and T4 diffuse into the fenestrated capillaries Exercise 14 for histology (Male reproductive system) I. Choice: Select the single most appropriate answer: 1. In spermatogenesis, it includes reduction from the diploid to the haploid number of chromosomes after two meioses, the first meiotic division occurs in the ( C ) A. spermatogonia B. primary spermatocytes C. secondary spermatocytes D. spermatids E. spermatozoa 2. The spermatids become spermatozoa undergoing ( B ) A. spermatogenesis B. spermiogenesis C. meiosis I D. meiosis II E. mitosis 3. The mitochondrial sheath of sperm is located in the ( C ) A. head B. neck C. middle piece D. principal piece E. end piece 4. After puberty the Leydig cells (interstitial cells) may produce (A ) A. androgen B. estrogen C. progesterone D. prostaglandin E. interstitial cell stimulating hormone II. Fill in the blanks: 1. The spermatogenic cells in seminiferous tubules include spermatogonium , primary spermotocyte, Secondary spermatocyte , spermatid and spermatozoon . 2. The epithelium of the prostate gland is simple cuboidal or Simple columnar or pseudostratified columnar epithelium. There are the prostatic concretion in the lumen of the prostate. 3. Segments of the tail in sperm are designated 4 pieces: (1) neck , (2) the middle piece , (3) the principle piece (4) the end piece . 4. In the end of seminiferous tubules, they continue the straight tubule and connect rete testis . they enter the cephalic portion of the epididymis . 5. The surface of testis is covered by tunica vaginalis , beneath it is thicker tunica albuginea . On the posterior surface of the testis, it forms the mediastinum testis . III. Questions: 1. Compare the structure and function of the sertoli cell with that of Leydig cell in the testis. Structure Function Sertoli cell 1) Have pale ,oval nucleus with a large nucleolus 2) Highly infolded 3) tight junction with adjacent Sertoli cells 1) support the spermatogenic cells 2) phagocytose excess cytoplasm 3)synthesize androgen-binding protein (ABP) 4) secrete inhibin 5)establish blood-testis barrier Leydig cell 1) Round to polygonal cells in the interstitial regions 2) Acidophilic cytoplasm Secrete testosterone 2. Describe the compostition of the blood-testis barrier. 1) Tight junction between adjacent Sertoli cells 2) protects developing sperm cells from autoimmune reactions 3. Compare the structure of ductuli efferentes with that of ductus epididymis. Ductuli efferentes: lined by simple epithelium composed of nonciliated cuboidal cells and ciliated columnar cells Ductus epididymis: lined by pseudostratified epithelium with nonmotile stereocilia on their luminal surfaces Exercise 15 for histology (Female reproductive system) I.Choice: Select the single most appropriate answer: 1. In the fifth month of fetus, the primordial follicles are estimated to number about (E) A. 700 B. 7,000 C. 70,000 D. 700,000 E. 7,000,000 2. The secondary oocyte completes the second mature division during (C ) A. follicle matured B. before fertilization C. fertilization D. ovulation E. 36-48 hours before ovulation 3. When ovulation occurs the discharged contents from the ovary include follicular fluid, (E) A. secondary oocyte, zona pellucida and cumulus oophorus B. matured ovum, granulosa cells and cumulus oophorus C. matured ovum, zona pellucida and corona radiata D. primary oocyte, zona pellucida and corona radiata E. secondary oocyte, zona pellucida and corona radiata 4. The location of cervical cancer is often in the ( A ) A. transitional portion between simple columnar epithelium and stratified squamous epithelium B. simple columnar epithelium C. stratified squamous epithelium D. cervical canal E. vaginal portion of cervix 5. The basal layer of the uterine endometrium (D ) A. is sloughed during menstruation B. has no glands C. is supplied by colied arteries D. is supplied by straight arteries E. is avascular 6. Which of the following statements concerning secondary ovarian follicles is true? ( C ) A. They lack liquor folliculi. B. They contain a secondary oocyte C. Their continued maturation requires follicle-stimulating hormone. D. They lack a theca externa. E. They have a single layer of cuboidal follicular cells surrounding the oocyte. II. Fill in the blanks: 1. Primordial follicle consists of a primary oocyte enveloped by only one layer of flattened follicular cells . 2. Only about 400 follicles reach full maturity. The woman’s reproductive life about 30-35 years. 3. There are two types of lutein cells: granulose lutein cells and theca lutein cells . 4. Dependant upon the expulsive ovum fertilized or not, the development of the corpus leteum may be divided into two types: corpus luteum of menstruation which persists for 14 days and corpus luteum of pregnancy which persists for 6 months. 5. The structure of uterus is composed of three layers: endometrium , myometrium and perimetrium . The epithelium of uterus is simple columnar epithelium . 6. The menstrual cycle may be divided mainly into three phases: menstrual phase , Proliferative phase and secretory phase . 7. The epithelium of cervical canal is simple columnar epithelium . The vaginal portion of cervix is lined by stratified squamous epithelium . III. Questions: 1. Describe the structure of the secondary follicles in detail. 1) moves deeper, increases in size 2) Stratum granulosum is 6-12 cell layers thick, fluid filled cavities appear among granulosa cells 3) Cavities eventually coalesce and form the antrum 4) cumulus oophorus which projects into the antrum 5) Cells of the cumulus oophorus that surround the oocyte will remain with it after ovulation and will be referred to as the corona radiata 2. Compare the structure and function of the granulose lutein cells with that of the theca lutein cells. Structure Function Granulosa lutein cells 1) large, pale cells that posses SER, RER, many mitochondria and lipid droplets 2) derived from cells of the membrane granulosa Manufacture most of the progesterone and convert androgens formed by the theca lutein cells into estrogens Theca lutein cells 1) small cells, concentrated mainly along the periphery of the corpus luteum 2) derived from cells of the theca interna Manufacture progesterone and androgens and small amounts of estrogen 3. Describe the structure of the oviduct. 1) The oviducts are subdivided into four regions: the infundibulum, the ampulla, the isthmus and the intramural portion. 2) The wall of each oviduct consists of a mucosa, muscularis and serosa. 4. Describe the structural changes and hormonal control of the endometrium in three phases of menstrual cycle. Proliferative phase: Regulated by estrogens -Epithelial cells in basal portion of glands reconstitute the glands and migrate to cover endometrial surface -Stromal cells proliferate -Spiral arteries lengthen as the endometrium is reestablished Secretory phase: Regulated by progesterone - Endometrium thickens - Glands enlarge Menstrual phase: Decline in the secretion of estrogen and progesterone - Glands stop secreting and endometrium shrinks - Stratum functionalis is sloughed off 5. Compare the structure between resting (nonlactating) and active (lactating) mammary glands. Resting phase: 1) fewer ducts and glands which lumens are small 2) Accumulation of adipose tissue in both interlobar and interlobular connective tissue Active phase: 1) relative amounts of connective tissue stroma and the adipose tissue decrease considerably 2) intense proliferation of the glands alveoli and ducts, the alveoli are distended by the secretion accumulated in their lumens Exercise 16 for Histology (Sense organ) Ⅰ. Choice: Select the single most appropriate answer. 1. The posterior wall of eyeball from outside inward contains A. fibrous layer,vascular layer and retina B. retina,choriod and sclera C. sclera,choriod and retina D. cornea,iris and retina E. Retina, vascular layer and fibrous layer 2. The Müller cells of retina belong to A. sensory neurons B. neuroglial cells C. interneurons D. photoreceptors E. motor neurons 3. The cells used color perception and fine visual acuity are A. ganglion cells B. Müller cells C. bipolar cells D.rods E. cones 4. The optic nerve fibers are constituted by axons of A. ganglion cells B. Müller cells C. Bipolar cells D. rods E. cones 5. The receptor of hearing is located on A. Vestibular membrane B. Crista ampullaris C. Maculae saccule D. Maculae utricle E. Organ of Corti 答案: 1. A 2. B 3. E 4. A 5. E Exercise 17 for Embryology (Fertilization to Implantation) Ⅰ.Multiple Choice: Select the single most appropriate answer. 6. The normal chromosome number of a human spermatid is (E ) A. 23 autosomes plus an X and a Y chromosome B. 22 autosomes plus an X and a Y chromosome C. 23 autosomes plus two X chromosomes D. 23 autosomes plus an X or a Y chromosome E. 22 autosomes plus an X or a Y chromosome 7. Which of the following chromosome constitutions in a sperm normally result in a male, if it fertilizes an ovum? (E ) A. 22 autosomes plus no sex chromosomes B. 22 autosomes plus one X chromosome C. 23 autosomes plus a Y chromosome D. 23 autosomes plus one X chromosome E. 22 autosomes plus a Y chromosomes 8. How many sperms would likely be deposited by a normal young adult male in the vagina during ejaculation? (B ) A. 300 thousands B. 300 millions C. 30 millions D.3 millions E. 300 9. The eight-day blastocyst: F. is surrounded by zona pellucide (D ) G. has about 6 to 8 cells H. lies under uterine epithelium I. is partially implanted J. has a secondary yolk sac 10. Ectopic implantations occur most commonly in the (C ) A. Ovary B. abdominal cavity C. oviduct D. cervix E. mesentery Ⅱ.Fill in the blanks: 1.There are three periods from fertilization to matured fetal: __preembryonic period______________, ______embryonic period_________ and ___fetal period____________. 2.At three days, a solid ball of 12-16 cells called __morula__________, leaves the uterine tube and enters the __________uterus__________. 3.The blastocyst consists of ____trophoblasts__________, ____inner cell mass_________ and ____blastcoele____________. 4.About the fifith day after fertilization, the membrane around the blastocyst, called the ____zona pellucida__________, degenerates and disappears. The _embryoblast pole________ of the blastocyst then attaches to the _uterine___epithelium. 5.Implantation is began on __5th__ days after fertilization and completed by __11th_____ days. 6.The trophoblast differentiates into the multinucleated ____syncytiotrophoblasts_______________ outward and __cytotrophoblasts______ inward. 7. According to the site of relationship between deciduas and blastocyst, three regions of the deciduas are identified as ____deciduas capcularis_________, _____deciduas parietalis______________ and __deciduas basalis____________. 8. Normally, the human blastocyst implants in the endometrium along the ___anterior_______________ and ____posterior______ walll of the body of the uterus. 9. During the second week of the development, the inner cell mass differentiates into ____amniotic cavity_______________ and ___primitive yolk sac____________.The two juxtaposed cells of these two cavities form a flat disc and they are known as the ___bilaminar germ disc___________. III. Questions: 1. The definition of the human Embryology. a science which study the processes and regulations of development of human fetus. 2. The major phases of fertilization and the site where fertilization typically occurs. Processes of fertilization: • • • Phase I penetrate the corona radiata, acrosomal release Phase II ZP with receptors – zona pellucida spongy – the release of local enzymes Phase III Success formation of zygote site: in the ampullary region of the oviduct 3. Endometrial changes that enable implantation and the hormones that modulates this change The endometrium of the uterus is in the secretory phase Hormonal regulation GnRH FSH LH Granulosa/theca cells Estrogens Progesterones 4. Normal sites of implantation and the most common abnormal sites. Implantation site Normal: anterior or posterior wall of the uterus Abnormal 1. Tubal 2. Internal os of the cervix 3. Ovarian 4. Abdominal 5. Morphologic changes in the zygote that occur enroute to the uterus Mitosis and cytoplasmic division Blastula - blastomeres Morula inner cell mass(embryoblast) outer cell rim(trophoblasts) Blastocyst Blastocoele The cells of morula secrete fluid Zona pellucide disappears 6. The development roles of the inner cell mass and the outer cell mass. inner cell mass--embryoblast outer cell rim-- trophoblasts 7. Bilaminar germ discs. Disc between amnion and yolk sac Bilaminar disc Epiblasts Hypoblasts