2007 body defence (teacher)
advertisement

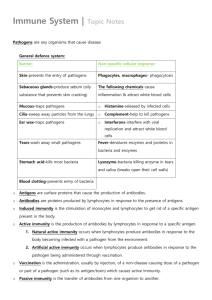
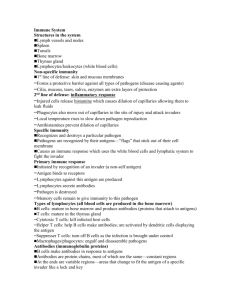
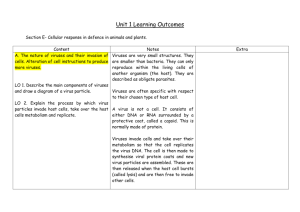
Body defence P. 1 Body defenses A. Causes of disease man is living in a world of microorganisms, many of which are pathogenic and can cause diseases - Pathogens = microbes that cause disease, they include certain bacteria, viruses protozoa and fungi Action of pathogens in humans - they cause infection by damaging the body tissues or producing toxins - they change the internal environment of human body - they upset the normal metabolic activities -- even though there exist over 100,000 species of fungi, only about 50 of these are known to be pathogenic for humans. Of theses, only a few are pathogens; most of them are opportunists (opportunists = able to cause infection in a compromised or weakened host) -- spread of infectious organisms: - contaminated water and food supplies - air currents or droplets - animal vectors (e.g. mosquitoes with malaria parasite) - poor sanitation - social interaction - body fluids / blood their effects are exacerbated by malnutrition and existing infections, since they reduce the body's ability to resist disease B. Against Disease - better life quality - well nourished - clean water and food - well established public health measures e.g. sewage disposal, body checking....etc. - defense mechanisms of the body ---> - prevent entry of pathogens into our body in the first place - fight against those pathogens that have entered - medicine / drugs ---> inhibit the growth of microbes / pathogens C. Defense Mechanisms two major types: - Non-specific Immunity ( Innate Immunity/ Non-adaptive Immunity) - Specific Immunity ( Adaptive Immunity) Body defence P. 2 C-I Innate Immunity - "innate" = " inborn" -- the mechanisms are present from birth and are not dependent upon previous exposure to pathogens - "non-specific" -- act on any type of invading pathogens -- not distinguish between different infectious organisms -- not become effective on subsequent exposure to the same organism - all animals have their innate immunity - first line of innate defense: Physical and Chemical barriers second line of innate defense: non-specific Leukocytes See the figure at below: - antisome = proteins which bind to foreign molecules that have been introduced experimentally, and may aid the elimination of such molecules by phagocytosis -- they have functional similarities to antibody molecules that vertebrates manufacture as part of the adaptive immune response -- may be the evolutionary precursors of antibody - cytotoxic cells = cells kill infectious organisms by secreting toxic molecules on to them or by puncturing their surface membranes. Body defence P. 3 1. Physical and Chemical barriers --- the first line of defence (第一道防線). Possible entrances through which pathogens may enter our body: Reproductive systems Respiratory system Digestive system Mechanical / Physical barriers: ---> prevent entry of pathogens i. intact skin - most effective due to its relatively impermeable horny layer (stratum corneum) ---> cannot be penetrated by most pathogens ii. intact mucous membranes / epithelium (e.g. gut or ciliate epithelium in the respiratory tract) - trapping air born / external agents with mucous - the trapped agents may be removed with the aid of mechanical movement of cilia iii. hairs - occurs in the certain openings of the body (e.g. nose) filter off the pathogens iv. coughing and sneezing reflexes v. blood clot on wound surface The importance of blood clotting in body defence Blood cells involved Red blood cells, blood platelets and special kinds of blood proteins Site of blood clotting On cut skin with damaged blood vessels Prevents excessive loss of blood from the body Function ∵ Excessive bleeding will greatly lower the pressure of the blood in the circulatory system Protects the body from invasion by pathogens through the wound Body defence P. 4 Reference only Haemophilia: - Heparin: an X-linked ingeritable disease due to low concentration of any essential clotting factors excessive bleeding - produced by most cells in connective tissues and liver prevent blood clotting in blood vessels Body defence P. 5 Chemical barriers various liquids and chemicals which are effective in inhibiting or destroying pathogens and prevents them from causing the body trouble i. sebaceous secretions and sweat of skin - low pH ---> inhibit the survival of bacteria on skin surface - contains bactericidal and fungicidal fatty acids ii. acid in gastric juice a powerful sterilizing liquid ---> preventing the entry of pathogens into guts iii. anti-bacterial enzyme (lysozyme) in breast milk, nasal secretions, saliva, tears and most tissue fluids iv. harmless bacteria living in gut and genital tract ---> compete for survival against infectious bacteria and fungi v. anti-bacterial protein (e.g. ) and zinc in semen (zinc is used for treatment of herpes infection) - - however these physical and chemical barriers may be breached by cuts, burns, grazes and enzymes or chemicals from certain pathogens (i.e. the first line of defense is broken) most of the chemical barriers are only weakly effective against viruses and various mechanisms have been evolved by infectious organisms to evade these barriers and gain entry to the body. Thus, a second line of defence is necessary and this relies on several types of cell, collectively called leukocytes. Body defence P. 6 2. Non-specific Leukocytes Leukocytes / Leucocytes (from the Greek leukos, meaning white) - often be called white blood cells, but this term creates the incorrect impression that these cells are always to be found in the bloodstream. - in fact, some leukocytes are never found in the vascular circulation, and those that do enter it spend only a very small proportion of their lifespan there. - we may use either leukocytes or white cells when we need a collective term for the many different cell types that collaborate in an immune response a. Phagocytosis engulfing pathogens that can escape the first line of defense 2 reasons to carry out phagocytosis: - to protect the organism against pathogens - to dispose dead, dying or damaged cells and cellular debris. 2 main types of phagocytic white cell which are responsible for destroying pathogens by phagocytosis - neutrophils - macrophages - eosinophils are also capable of phagocytosis but this is not their main function - when monocytes enter tissues from blood it becomes macrophages - neutrophils do not divide once they have entered the bloodstream -- Neutrophils predominately in blood stream Macrophages / Monocytes -- predominately in tissues (contributing between 50 and 70% of total ' white count') ----- multi-lobed nucleus -granulocytes -most abundant white cell in blood -live only a few days -- (contributing less than 7 % of white cells circulating in bloodstream are macrophage but larger numbers are found widely distributed through out body tissues kidney-shaped nucleus can be recognized in microscope agranulocytes largest white cell long lived Mechanism: Phagocytes are attracted to chemicals produced naturally by bacteria along a concentration gradient. labelling of pathogen cell-membranes that identifies the pathogen as a target for phagocytosis and aids adherence of phagocyte to the pathogen (i.e. Opsonisation) formation of pseudopodia around the target and enclose it in plasma membrane to form a vacuole, Phagosome fusion of phagosome with lysosomes inside the phagocyte enzymes and toxic molecules destruct the pathogen, the products are absorbed by phagocyte and the residues are discharged out of phagocyte Body defence P. 7 Mechanism: labelling of pathogen cell-membranes with a molecule, opsonin, (opsonins are specific serum proteins; in Greek: opson = cooked meat => made ready for the table) that identifies the pathogen as a target (e.g. carbohydrate residues in bacterial cell walls) for phagocytosis and aids adherence of phagocyte to the pathogen (i.e. Opsonisation) triggers a system of contractile actin-myosin filaments inside phagocytes which enable the cell to throw ‘arm’ of cytoplasm formation of pseudopodia around the target and enclose it in plasma membrane to form a vacuole, Phagosome fusion of phagosome with lysosomes inside the phagocyte enzymes and toxic molecules destruct the pathogen, the products are absorbed by phagocyte and the residues are discharged out of phagocyte * - opsonin include antibodies, acute phase proteins and complement they coat the pathogens and bind to receptors in membrane of the phagocytic white cells to promote phagocytosis - toxic molecules in lysosomes e.g. H2O2 and free radicals, they are oxidizing agents ---> uncontrolled oxidation cause break-up of pathogen's membrane since lipids in its cell membrane are particularly sensitive to oxidation. Body defence b P. 8 Cytotoxicity killing the infectious organisms by damaging the cell surface (membrane) - by cytotoxic white cells (may require antibody bound to target or not) e.g. - Eosinophils -- about 3 % of leukocyte in bloodstream -- can generate a burst of oxidising agents -- also granules with degradative enzymes and a cylindrical protein (perforin) that can perforate cell membranes ---> to inflict damage on multicellular parasites, such as worms and flukes...etc, which are too large to be phagocytosed -- not depend on opsonins but adherence to target can be greatly enhanced by opsonins - c. others : Natural killer cells (Ab-independent) and Killer cells (Ab dependent) -- all are large granular lymphocytes Acute Inflammatory Response A local response (at sites of infection, also around cuts, burns and grazes to the skin), besides phagocytosis and cytotoxicity, inflammatory response is a more powerful non-specific response to eliminate pathogens: - release of histamine (and other biologically active molecular) by non-phagocytic basophils and mast cells provoke an intense but acute (short-lived) inflammatory reaction around the site of an infection: [when the Ig E (an antibody molecule) on these cell’s membrane bind to antigen, degranulation occur and histamine contained content is released] - attraction of phagocytes to the site - increase blood flow to the site - local blood vessels become dilated and leaky (i.e. increase vessels permeability) to plasma and white cell ---> redness, swelling, heat, pain - basophils circulate in bloodstream whereas mast cells remain stationary in connective tissue, and are especially abundant in respiratory tract. *- when basophils enter tissues they become mast cells, both of them are non-phagocytic - plasma may contains antitoxins, antibodies, bactericidal, or viricidal - the value of inflammatory reaction is -- the inrush of plasma brings a large number of phagocytic and cytotoxic cells to the infection site, together with molecules that aid their activity, e.g. opsonins and antibodies. -- any harmful substance released by pathogen may also be diluted by the large volume of plasma. - acute inflammatory reaction is accelerated by molecules secreted by the first cells to arrive; these molecules recruit more cells, which in turn release molecules that further enhance the inflammatory reaction. (i.e. positive feedback loops exist to ensure that the reaction , once triggered, proceeds very rapidly). You would also expect, inhibitory mechanisms also exist to damp down the reaction and prevent it from spreading, but if these mechanism fail (as they sometimes do when the infection is persistent) then the inflammation can become chronic and serious damage results. - an allergic inflammatory reaction can also be triggered in some people by non-infectious material, such as pollen grains, house dust mites, animal fur and certain foods (e.g. certain GM foods) - it is worth emphasis that innate responses including inflammatory reactions begin within a few hours of infectious organisms entering the body. This is much faster then the responses of adaptive immunity, even when the pathogens have been encountered before. So the mechanisms of innate immunity are the sole means of defence in the period of at least several days following an infection before a primary adaptive response can be detected. Body defence P. 9 C-II Adaptive Immunity "adaptive" - refers to the ability of the mechanism to change in characteristic ways following an infection (i.e. with memory) (immunological memory is a property that distinguishes adaptive from innate immunity) "specific" - defense mechanism that depends on specific recognition of the invading pathogen for action - exhibit in 'higher' vertebrates (in humans, adaptive immune response is generally more effective against bacteria and viruses than it is against parasites, with which it maintains at best an uneasy truce ??) - response due to induction of lymphocytes by antigens - Small Lymphocytes: -- they are small agranulocytes, no granules in cytoplasm, with large nucleus -- hence they are recognisable under microscope since they have a very low ratio of cytoplasm to nucleus, few organelles and no granules -- two important groups of small lymphocytes: - T cells turn on CMIR - B cells turn on HIR -- both T-lymphocytes (T-cells) and B-lymphocytes (B-cells), like other blood cells, originate from stem cell in haemopoietic tissue (yolk sac and liver in feotus; bone marrow in adults) Body defence P. 10 primary lymphoid tissue (bone marrow, thymus) = tissues where specific lymphocytes are formed) -- B cells mature in bone marrow, while some others migrate via blood to thymus and differentiate into specific mature T cells -- then matured naive B and T cells then migrate to secondary lymphoid tissues secondary lymphoid tissues (e.g. lymph nodes, spleen) = tissues where T cells and B cells accumulate -- where pathogens in blood and lymph are caught ∴ there are the places where pathogens stimulate B and T cells and turn on the specific immune responses Body defence P. 11 Reference information: - mutipotent stem cells: as few as 30 of these stem cells are sufficient to regenerate the entire white and red cell population of a mouse after the original cells have been destroyed by radiation. - The names given to the different types of leukocyte generally tell you something about their function, biochemistry or morphology: 1. Lymphoid cells - spend most of their lifespan in the lymphoid system, which consists of organs such as the lymph nodes, tonsils and spleen, connected by a network of lymphatic capillaries 2. Granulocytes - all have numerous electron-dense structure (referred to granules) in their cytoplasm - neutrophils do not stain with either acidic or alkaline dyes -- eosinophils stain with acidic dyes (of which eosin is one) -- basophils (and mast cells) stain with alkaline (basic) dyes - granules are in fact membrane-bound 'packets', which contain numerous biologically active molecules, including enzymes and toxins. A more accurate biological term for these structure would be vesicles. But, since immunologists always refer to white-cell vesicles as ' granules', many books follow this tradition. 3. monocytes - which migrate out of the blood capillaries and into tissues and organs all around the body, where they differentiate into macrophages. Macrophage literally means 'big eater', from which you can deduce that these cells are phagocytic. Body defence P. 12 - Antibodies (immunoglobulin, is the secreted form of B cell surface receptors without the portion for attachment on B cell membrane) : = a Y-shaped protein molecule synthesized by an animal in respose to the presence of foreighn substance (antigens) for which it has a high affinity. - Antigen: a cell or macromolecule that has ligands in its structure that are bound specifically by receptors in the membranes of T- / B- lymphocytes or antibodies and thus stimulate a specific immune response (e.g. bacteria, virus, drugs, pollutants, pollen grains ...etc.) - Epitopes (antibody binding site on an antigen): the antigenic ligands (with molecular conformations do not usually occur on the cells and macromolecules of the host's own body, they usually are polypeptides, glycoproteins or glycolipids) on the surface of an antigen antibodies (and hence B cells) bind to 'native antigens (i.e. intact antigenic macromolecules) ' as they occur in life, either free in the body fluids or as part of the surface structure of an infectious organism. This is very different from what the cells recognise as an antigen (involve MHC, APC ???) although the epitope represents only a small portion of structure of the infectious organism, the interaction of the epitope with the complementary receptor on an adaptive immune cell triggers an immune response that can destroy the intruder. Body defence P. 13 Antigen specificity, clonal selection & clonal expansion: -- each small lymphocyte has receptor molecules of unique structure and specificity that bind to just one single type of epitope with a complementary conformation or at most a few structural analogues of that epitope --> enables the adaptive immune response to be highly specific -- the population of small lymphocyte in the body consists of millions of different clones (cells of a clone arise from a single cell) -- each clone with receptors for a particular epitope ( at least 108 clones exist in the small lymphocyte population in an individual) -- when infected, particular clones of lymphocytes with complementary receptors for the epitopes on the antigen will be selected to bind with the epitopes (i.e. clonal selection) * - usually an antigen may have a number of different epitopes on their surface and might 'select several clones of naive lymphocytes - naive lymphocytes = lymphocytes that have not yet encounter their corresponding antigen -- the 'selected' lymphocytes will then replicate several times to increase the cell number of those clones (i.e. clonal expansion) Body defence P. 14 - Effector cells & Memory cells -- during clonal expansion: maturation and differentiation of proliferated cells also take place -- most of the new cells formed are plasma cells ( or called effector cells ) ---> short lived and carry out immediate action to eliminate the antigens -- some of the new cells formed differentiate into memory cells ' memory' does not imply any similarity with the mechanisms of memory storage in the brain. However the term is useful in describing changes in the adaptive immune response following the experience of an infection. - with long life and circulate in the body after the original exposure to the antigen is over and the effector cells have died - generally replicate at intervals to replenish the pool of memory cells ---> offer a life-long protection against the antigen: i. larger population in circulation than those naive cells ii. more rapid secondary response which may be effective enough to prevent symptoms from arising or the expansion of the antigen population in the body - primary response -- the response that is elicited when antigen entered into the body for the first time (i.e. first encountered antigen): naive lymphocyte with receptors complementary to epitopes on the antigenic pathogen / and occasionally on a parasite (i.e. clonal selection by specific antigen) Clonal expansion and differentiation plasma cells + memory cells - secondary response -- response caused by any subsequent entry by the same antigen: memory cells ----> effector cells + memory cells response to a previously encountered pathogen may be sufficiently effective to prevent subsequent infections from causing any symptoms (in which case the host animal is said to be immune to that pathogen) - Mechanisms: 1. Cell-mediated immunity (T cell-dependent immunity) 2. Humoral immunity (B cell-dependent immunity / Antibody-mediated immunity) Body defence P. 15 Body defence P. 16 C-II-1 Cell-mediated Immune Response (CMIR) - T cell population is divided into subsets, each with specialized functions: i. Cytotoxic T cells (Tc) - e.g. NK cells and K cells ---> use toxic and pore-forming chemicals to kill the infected own body cells ii. Helper T cells (Th) ---> for regulation: synthesis and secrete a range of molecules (lymphokines) with activating or enhancing effects on other white cells iii. Suppressor T cells (Ts) ---> opposite effect to Th : prevent the activation of other immune cells or cause them to reduce their activity or cease functioning altogether - each subsets have characteristic marker (receptor for ligands) molecules, that have internationally agreed CD number (CD = cluster of differentiation) Primary and Secondary Response of CMIR Specific naive T-cell being selected by 1st encountered antigen 3 kinds of plasma T-cells + memory T-cells (i.e. 1o response) Subsequent encounter of the same antigen Much higher level of the plasma T-cells + more specific memory T-cells (i.e. 2o response) Body defence P. 17 C-II-2 Humoral immunity when antigens reach the lymph node / spleen, B cells there may be stimulated by T-independent antigens (not require the help of T cells) directly or stimulated by T-dependent antigens in the presence of correct T helper cells - antigen stimulate specific B cells multiply and differentiate into memory cells and antibody forming plasma (/ effector) cells (i.e. primary response) - B cells may also be activated regardless of their antigen specificity by certain polyclonal activators. These include powerful mitogens (compounds that cause cells to under mitosis), some of which are also components of bacterial cell walls. Another polyconal activator is the Epstein-Barr virus, which is involved in the causation of an immune-cell cancer (Burkitt’s lymphoma) - Antibodies (immunoglobulins / Ig) -- Y-shaped structured globulin molecules -- secreted form of the same Ig molecules that original B cell used as its surface receptor -- appear in blood stream and tissue fluids -- with antigen binding sites (paratopes) at the two ends of the 'Y' -- help to destroy /eliminate antigen by: i. activation of complement-mediated lysis of bacteria (i.e. cytotoxicity) ii. aid in activation of inflammatory reaction iii. aggregation of small antigens to facilitate phagocytosis iv. neutralize bacterial toxins by forming Ag-Ab complexes which are then phagocytosed v. label the pathogens or antigens (i.e. act as opsonin) for phagocytes vi. activation of K cell cytotoxicity (ADCC) * However antibody-mediated immune responses are most effective against free-living pathogen, parasites and antigens macromolecules in the many types of pathogens, including viruses, that replicate and live inside the cells of their host. Our main defense against these intracellular pathogens is the T cells (via the presentation of the processed intracellular antigens on the cell surface of Ag-presenting cells) Primary and Secondary Response of HIR Specific naive B-cell being selected by 1st encountered antigen Antibody secreting plasma B-cells + memory B-cells (i.e. 1o response) Subsequent encounter of the same antigen Much higher level of the plasma B-cells + more specific memory B-cells (i.e. 2o response) Body defence P. 18 Body defence P. 19 Reference material Body defence P. 20 - primary and secondary responses of Humoral Immunity Primary response Secondary response longer lag period shorter lag period (slower response) (fast response) smaller response sharper increase and higher level of antibodies produced (larger response) short-term effect high level of antibodies stays longer (long lasting effect) mainly IgM mainly IgG Body defence P. 21 Reference material - Human foetus antibodies level Body defence - P. 22 difference between 2 defence systems: Specific defence system Mechanism CMIR or HIR Action on foreign body Act on specific substances only Non-specific defence system Physical and chemical barrier, Phagocytosis, Infamation Eliminate all foreign substances non-selectively Formation of memory cell Both B or T cells may develop and No immunological memory cells is persist in the circulation formed Secondary response Present No such phenomenon Biological significance Immunity can be established to Fight against invading substances fight against the foreign substance in a fast fashion efficiently in secondary response - Biological significance of CMIR 1. establish active immunity to resist infections as formation of T memory cells 2. cause unwanted immune response. Grafts or transplants are rejected if they are immunological incompatible to the recipient. 3. destroy unwanted cells in the body, i.e. tumor. It is found that the T killer cells can eliminate and kill the tumour cells with the aids of phagocytes 4. fast in action to combat the invading pathogens since T lymphocytes circulate within body fluid 5. the deficiency and failure development of CMIR is thought to be related to the “AIDS” (acquired immunodeficiency syndromes). The T cells in this case are destroyed by the HIV (human immunodeficiency virus) and the patient performs no CMIR any longer. - Biological significance of HIR 1. antibodies are produced by the selected B cells to act against the invading bacteria, viruses and toxic matters 2. active immunity is able to establish in the body by the development of B memory cells to prevent disease 3. immunoglobulins (antibodies) can be isolated from the body, and used in the replacement therapy in humoral-antibody-immunodeficiency disease to prevent recurrent bacterial infections 4. serum containing antibodies can be collected from horse, and used in the therapy of tetanus, snake bites, some viral disease (e.g. rabies and other diseases) 6. the immunoglobulins are also used in prevent of graft rejection in patients with transplanted organs; for this purpose anti-lymphocytes serum, containing antibodies against lymphocytes is used. Body defence P. 23 Types of immunity & immunization (Vaccination) 1. Passive immunity - a result of antibodies being passed into an individual in some way, rather than being produced by the individual itself. - more effective and sensitive in a rapid fashion but the duration is short (as antibodies are metabolized in a few months, the protection is short-lived) a. Naturally acquired passive immunity e.g. Abs from maternal blood to - foetus across the placenta; - child by lactation b. Artificially acquired passive immunity e.g. by injection of ready-made Ab (such as treatment of tetanus or snakebites in humans) e.g. rabies, hepatitis A, German meascles during pregnancy, to treat snakebites 2. Active immunity - Abs produced by the individual itself as a result of contact of antigen a. Naturally acquired active immunity as a result of infection by the antigen containing pathogen b. Artificially acquired active immunity (Vaccination / Immunization) to be induced to produce Abs even without suffering disease achieved by injecting small amount of Ag (vaccine) into body - introduced Ags is usually safe because they may be: 1. Living attenuated microorganisms pathogen is treated and becomes unable to cause the symptoms or disease 2. Non-virulent strain of microorganisms or infectious agent of a related harmless disease 3. Dead microorganisms 4. Toxoids the detoxified toxins produced by some diseases 5. Extracted Ags from organism’s cell surface 6. Artificial antigens synthesized by -- transfer the genes of antigens to a harmless organism which have offspring express the Ag to induce immune response; -- amino acid sequence of antigen is determined to synthesize Ag in vitro Body defence P. 24 - Routine immunization Immunization schemes used in tropical countries are a little different from those usual in temperate countries; in the tropics (or sub-tropical cities, e.g. HK) it is important to provide early protection for children against many of the diseases encountered, since their morbidity and mortality are mostly more serious and occur at a young age than in temperate climates. - Vaccines for special groups 1. sex groups young girls are advised to administrated with vaccines of German measles since the disease will cause abnormality of the foetus when the girls are pregnant (boys are also infected by the German measles, but the symptoms are mild so boys are not necessary to have vaccination on such disease) 2. age groups young children are often vaccinated against polio, smallpox, measles, cough etc. since they are high risk group to be infected with such disease 3. occupational groups some occupations are high risk for a certain disease, i.e. hepatitis B vaccine is recommended for medical workers, plague vaccine for sewage workers, field worker etc. The need of a booster dosage in immunization programs: The first injection of vaccine brings about a primary immune response which provides low levels of antibodies and memory B-cells only. However the antibody level is not sufficient to protect the person from infection. The booster injection stimulates the proliferation of memory B cells and production of antibodies which stay in the body for a longer period of time. Therefore, further infection is prevented by the artificial acquired immunization. Assignments: 1. The importance of immunization progammes in Hong Kong and comparison of the incidence of(e.g. Hepatitis B or poliomyelitis) a disease before and after a immunization programme has been introduced. 2. Disscuss the importance of immunization programmes in Hong Kong to personal and community health. Body defence P. 25 D. Other examples of Ag-Ab system: 1. Blood Groups - blood group antigens are a variety of glycoproteins found on the surface membrane of red blood cells - the most important blood grouping methods: a. ABO system - the best known and most important blood grouping system - 2 types of antigens: A and B ----> 4 blood groups Blood Ag on Ab in group RBC plasma surface A A anti-B B B anti-A AB A and B None O None Universal recipient anti-A & Universal anti-B donor - spontaneous existence of antibodies against Group A or Group B antigens in body probably lies in common occurrence of immunogenic sugars of antigen A and antigen B in bacterial cell wall which everyone may have encountered them at early age. b. Rhesus antigen (antigen D) - either present (Rh+) or absent (Rh-) on red cell surface of a person - not make antibodies spontaneously to antigen D in Rh- person until first encounter of Rh+ red cells via: -- first transfusion of Rh+ blood cell into Rh- person; or -- leaking of baby‘s Rh+ blood cells into mother’s bloodstream during first birth of Rh+ baby in Rh- mothers - Incompatible blood transfusion ---> - clumping then lysis of donated red cells - blocking of vital vessels by clumped blood cells ---> failure of kidney - Haemolytic disease of newborns(Rh+) after the first birth of Rh+ baby since antibodies to antigen D is present in mother‘s blood circulation Body defence Reference information P. 26 Body defence P. 27 Reference information Body defence Reference information P. 28 Body defence Reference information P. 29 Body defence P. 30 2. Organ & Tissue Transplantation examples: Organs -- kidney, heart Tissues -- cornea (cornea with no antigen on cell surface, so no rejection would occurs during transplantation, i.e. immunologic tolerance) -- blood transfusion -- blood marrow -- heart valve -- skin grafting -- tendon & cartilage ...etc. Tpes of transplantation: a. Isograft a graft between 2 genetically identical individuals such as identical twins b. Autograft tissue grafted from one area to another on the same individual c. Allograft a tissue grafted from one individual to another individual of the same species but of different genetic constituent d. Xenograft a tissue grafted between individuals of different species such as from pig to man Problems of transplantation: every human has his own cell surface antigen (which is genetic programmed, variation among different persons is due to genetic variation among the population) e.g. A, B antigens on RBC; MHC (major histocompatibility complex) on body cells - if the donor‘s cells do not match with recipient’s the transferred cells will be recognized as ‘ foreigner’. Any foreign tissues will act as antigen which will then elicit the recipient‘s immune response (i.e. the transplanted organ is rejected). In general, two types of response may occur. e.g. blood transfusion -------> HIR transplanted organs -----> CMIR - Mild consequence may be death of the transplanted tissue, eg. skin transplant. - More serious consequence may be death of the recipient. e.g. incompatible blood transfusion hence, before transplantation, tissue histocompatibility test should be carried out first Body defence P. 31 Solution: Prevention of rejection is the best policy. Three methods can be employed. All can minimize the harmful effect of transplantation. they are i. tissue matching - usually organ / tissues from close relations may be more histocompatible to recipient ii. x-irradiation iii. immuno-suppression. - in order to increase the chance of success in transplantation, immunosuppressive drugs or Xirradiation exposure of bone marrow and lymphoid tissues are applied to inhibit the expression of antigen to cell-mediated immunity - if no histocompatible organs could be obtained, artificial device may be any other choice for substitution: -- heart pacemaker (electrical) -- ball & socket joint (mechanical) -- heart valve ( mechanical) -- cochlear implant (electronic) Body defence P. 32 Reference materials - MHC (major histocompatibility complex) they are molecules that occur on the surface membrane of virtually all cells in the body - antigens presented on MHC of body cells or macrophage: antigen receptors on particular T cell's surface binds simultaneously to the processed fragments of particular antigen that bound to MHC on the host cells which are harbouring intracellular pathogens. Then primary response is triggered - if the same antigen is encountered in the next time, secondary response will be triggered Body defence P. 33 E. Chemotherapy (The use of drugs) Chemotherapy - use of chemicals to prevent and cure disease & disorders 1. Chemicals extracted from certain plants 2. Antibiotics - chemicals produced by fungi & bacteria - different antibiotics have different range of effective spectrum ---> suppress the growth of other microorganism (some other fungi or bacteria but not viruses) around them e.g. Penicillin ---> prevent synthesis of bacterial (prokaryotic) cell wall ( Other antibiotics may interfere DNA, RNA, protein synthesis and cellular metabolism of the microorganisms.) Antibiotics can be produced by artificial method, eg. technique of recombinant DNA, protein engineering and cloning. The consequences of indiscriminate use of antibiotics: Frequently used of antibiotics will lead to decrease in effectiveness of them. It is because microbes will be immune to the antibiotics through repeated mutations. It was noticed that certain bacterial cells developed resistance to antibiotics, Ic. The antibiotics failed to kill them in the normal way. Resistance is arose by mutation. This mutation allowed the bacteria to survive in the presence of drugs like penicillin by producing an enzyme to break it down. In the presence of penicillin, non-resistant forms are destroyed. There is a selection pressure favouring the resistant types. The greater the dosage and frequency of its use, the greater are the selection pressures. At last the anti-antibiotic super bacteria are born. When taking antibiotics, it is important to follow the doctor’s instruction to complete the treatment cycle by finishing the pills all even though there is an apparent recover from the disease. Otherwise, a little bacteria still survive and are selected to become the resistant strain. 3. Interferon It is produced by infected cells which can interfere with the viral replication. Interferon triggers a series of events which lead to an inhibition of vira’ protein synthesis, viral RNA transcription, assembly and release of virus particles. It can inhibit cell growth and is used as an anti-cancer agent under certain circumstances. Body defence P. 34 4. Synthetic drugs e.g. Sulphonamides - most widely used synthetic drugs - low cost and effective with some common bacterial diseases - structurally similar to precursor of bacterial nucleic acids, hence competitive inhibition of nucleic acid synthesis in bacteria competition p-aminobenzoic acid (precursor of nucleic acid) Sulphonamides folic acid purines DNA or RNA - Problems of drug therapy -- induction of drug resistant mutants of pathogens if prolonged use -- may cause undesirable side effect (hypersensitivity or irritation) -- may not suitable for all patients, e.g. pregnancy women -- eliminate the normal micro-organism in gut of patients, clonal explosion of resistant mutants may occur Body defence P. 35