Guillain - Kerala Medical Journal
advertisement

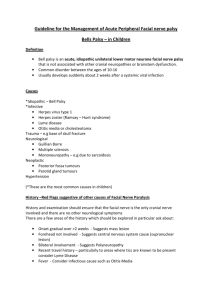
Guillain-Barré Syndrome with Bilateral Facial Nerve Paralysis Author- Dr. Ranzeeb Rasheed, PG in Gen. Medicine, MGMC&RI, Puducherry Co-author- Dr. Kalirattiname, Associate Prof., MGMC&RI, Puducherry Abstract Guillain-Barré syndrome is an acute demyelinating disorder of the peripheral nervous system that results from an aberrant immune response directed at peripheral nerves. It may also involve cranial nerves. The exact mechanisms which cause the conditions aren't clear, but about 60 per cent of those affected will have had a throat or intestinal infection, flu or major stress within the previous two weeks. Bacteria such as Campylobacter and mycoplasma pneumonia, and viruses such as Epstein Barr virus and cytomegalovirus are some of the organisms that have been reported to be involved. Introduction Bilateral facial nerve palsy is an extremely rare presentation. Common causes for bilateral facial nerve palsy are Guillain-Barré syndrome, leukaemia, Lyme’s disease, sarcoidosis, leprosy, and trauma. Case Presentation A 14 year old male student presented with 1 month history of lower limb weakness with bilateral facial weakness. He was treated for the same in a different hospital. One week prior to the onset of weakness, he had fever with sore throat. One month back the patient had experienced sudden onset of weakness of lower limb which was progressive in nature with inability to walk along with difficulty in swallowing and bilateral facial weakness over a period of 1-2 weeks. This was followed by a mild recovery in the weakness of the lower limb and complete resolution of dysphagia with persistence of facial weakness. The whole episode was managed conservatively. On examination, there was bilateral lower motor neuron type of facial palsy along with lower limb weakness (2/5 in all muscle groups) while power in the upper limb was normal. All deep tendon reflexes demonstrated areflexia. Plantars were flexor. No bladder or bowel involvement with normal fundoscopy. Blood investigations were normal. CSF demonstrated elevated protein content with normal cell counts suggestive of albumino-cytological dissociation. CSF bacterial antigen detection for H. Influenza type B, Streptococcus Pneumoniae, Meningitidis Group A, Meningitidis Group B, and Streptococcus Group B were absent. MRI brain showed no significant abnormalities. EMG / NC finding were suggestive of generalised, symmetric, motor>sensory (axonal > demyelinating) polyradiculonueropathy affecting lower limbs more than upper limbs Patient was started on steroids; improvement in lower limb power along with mild recovery of facial weakness was noted over a period of one week from admission. Discussion Bilateral Facial Nerve Palsy may be the presenting feature of metabolic, infectious, vasculitic, immunological, neoplastic causes. Patient with history of tick bite with presence of erythema chronicum migrans with recent travel abroad should be suspected to have Lyme’s disease, other infectious disease like HSV and IMN should be ruled out by doing serology screens , multiple sclerosis should be screened by doing MRI brain , CSF for oligoclonal bands and visual evoked potential. Sarcoidosis , SLE , Vasculitic disorders should be ruled out by doing a ANA , ACE levels , pANCA, cANCA , other causes like leukemia, lymphoma can be diagnosed by doing a peripheral smear and bone marrow biopsy. Guillain-Barré syndrome is an Acute Inflammatory Demyelinating Polyradiculonueropathy that presents with facial nerve palsy in 27-50% of cases. Other cranial nerves may also be involved. Diagnosis is confirmed clinically by the presence of ascending flaccid paralysis, areflexia without any definite sensory level with CSF showing albumin- cytological dissociation and nerve conduction studies showing demyelinating pattern. Management includes IVIG infusion or Plasmapharesis along with ventilator support in case of respiratory failure due to involvement of diaphragm. Conclusion Guillain-Barré syndrome should be included in the differential diagnosis of bilateral facial nerve palsy. Reference 1) JEREMY H. REES, PH.D., M.R.C.P., SARA E. SOUDAIN, B.SC., NORMAN A. GREGSON, PH.D., AND RICHARD A.C. HUGHES, M.D. , CAMPYLOBACTER JEJUNI INFECTION AND GUILLAIN–BARRÉ SYNDROME , THE NEW ENGLAND JOURNAL OF MEDICINE Nov. 23, 1995 2) Dr Trisha Macnair, Guillain-Barre syndrome, www.indymedia.us/en/2009/04/37135.shtml 3) Guillain-Barre syndrome, www.pubmed.com A.D.A.M. Medical Encyclopedia., 4) Charles F. Bolton, M.D., The Changing Concepts of Guillain–Barré Syndrome, N Engl J Med 1995; 333:1415-1417November 23, 1995 5) Guillain Barre Syndrome, Disease of Peripheral Nerves, Part 5Diseases of Spinal Cord, Peripheral Nerve and Muscle, 8th edition, Adams and Victor’s Principles of Neurology.