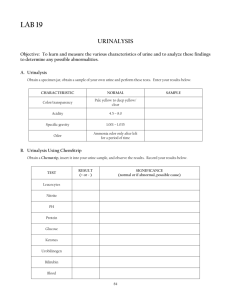
Practical trainings from biochemistry
advertisement

Practical trainings from biochemistry (2nd semester, module A) A1 Serum protein electrophoresis (ELFO) A2 Examination of urine A3 Determination of blood glucose level (glycemia) A4 Determination of alkali phosphatase in serum (ALP) General information Practical trainings are part and parcel of teaching of medical chemistry and biochemistry in the 1 st year of studies of General medicine. Topics of the practical trainings are related to lectures and seminars and try to show how the theory is applied in a laboratory practice. Students can see how biochemistry is used in a clinical medicine. Topics of the 2nd semester improve understanding of biochemistry of a human body. How to make preparations for the practical trainings? 1. Read laboratory safety regulations before the first practical training. You can not work in a laboratory before you are familiarized with the safety regulations (you can download the document from the internet). 2. Prepare the tools: own white laboratory coat permanent marker writing things calculator free page of paper of A4 format (designated for report) 3. It is useful to be familiarized with a laboratory equipment you will use during the practical training (see PowerPoint presentation on the internet). There will be a brief training on handling with the laboratory equipment at the seminar preceding the first practical training. 4. It is necessary to study instructions found in this document thoroughly before each practical training: you must know a theory of used laboratory analytical method and be familiarized with a procedure of your task (do not memorize the procedure step by step, but try to understand it before you start work). Printed procedures of all tasks are available in the laboratory, it is not necessary to bring own copy of the instructions. 5. You should be able to answer the questions: What is the aim of the experiment? What is the general procedure to reach the aim? What is the principle of the used analytical method (i.e. how does the method work)? 6. The instructions include a list of required knowledge for each of tasks. You will be tested by your teacher from the knowledge during each of the practical training. 7. Read laboratory report reuirements (see below). The report is one of credit requirements you must fulfill. Each student treats a laboratory report individualy immediately after an experiment is finished. The report must be checked by your teacher before you leave the laboratory. Only the report confirmed by the teacher can be used as a proof of fulfilled practical training. Keep your reports as your proof of laboratory work by the time you obtain a credit from chemistry. It is not allowed to process the report by a computer. 1 The report must include: 1. 2. 3. 4. 5. 6. 7. 8. 9. name and surname of student + group number date name of the task aim of the experiment (briefly described) principle of used analytical method (briefly described) possible differences from instructions (do not copy a procedure from the instructions) all measured and calculated values description of used calculation (related to your results), calibration curve (task B1 only) all results in a clearly organized table, including an identification number of a control sample (if used in the experiment) 10. conclusion including answers to all questions found in the instructions + evaluation of reached results (compare them with a theory) Model Laboratory Report Full student name / group number Date: 24.12.2000 Task: B5 / Determination of bilirubin concentration in blood serum Aim of work: Aim of the experiment was to determine concentration of both total and direct bilirubin in two samples: my own serum and a control sample No 5. The concentration was measured by spectrophotometry. Reached results were compared with known physiological range of bilirubin concentration. Principle of used analytical method: Spectrophotometry is an analytical method based on absorption of monochromatic radiation by a compound of interest. As its concentration increases the measured absorbance increases too (Lambert-Beer´s law: A = c x l x e, where A = absorbance, c = molarity, l = optical lenght, e = molar absorptive coefficient). Using known value of bilirubin concentration of a standard solution (st) and measured values of the absorbances it is possible to calculate concentration of bilirubin in unknown samples (us), i.e. blood serum and the control sample: cus / Aus = cst / Ast Total bilirubin (= sum of conjugated and unconjugated bilirubin) is determined after chemical transformation of bilirubin to an azo dye, which absorbs in a visible range of an electromagnetic radiation. Conjugated bilirubin can be determined directly after mixing of a sample with a reagent (it is why the term "direct bilirubin" is sometimes used for the conjugated bilirubin), whereas to determine the total bilirubin addition of an accelerator into the reaction mixture is necessary (it releases the unconjugated = "indirect" bilirubin from albumin - its transport protein in blood; only free bilirubin can react with the reagent). Procedure: I have followed the instructions with almost no differences. The only variation was measuring of all the analyzed samples twice to increase precision of the analysis. An average of the values was used as a final result. Measured values: absorbance total bilirubin average: direct bilirubin average: standard 0,690 0,700 0,695 0,124 0,125 0,125 control sample No 5 0,322 0,326 0,324 0,015 0,017 0,016 serum 0,083 0,087 0,085 0,011 0,011 0,011 blank sample 0,016 0,005 Calculations: cus / Aus = cst / Ast cus = (cst / Ast) x Aus The absorbace of a blank sample was subtracted from the other absorbances automatically by the spectrophotometer (the instrument was set to zero using the blank sample before measuring the other samples). Results: concentration of (μM) total bilirubin direct bilirubin standard (known values) 115 23 control sample No 5 serum 54 3 14 2 Conclusion: Concentration of bilirubin in my serum sample was found within the physiological range (for total bilirubin: 3,4 - 17,1 μM, and for direct bilirubin: 0 - 3,4 μM). I have found increased value of the total bilirubin in the control sample No 5, whereas its direct bilirubin was not elevated. A cause of the results can be either a liver damage or increased hemolysis of erytrocytes. The results found in the control sample differ from an expected values (obtained from my teacher) by 3%. Because the alloved deviation is 10%, the results can be evaluated as correct. student signature 2 Organization of Practical Trainings Observe your schedule of the practical trainings. In case of late arrival the practical training must be compensated at some other time, see below. You will work in pair in a laboratory: each study group is divided to 8 working groups (= pairs or groups of three if necessary). Laboratory report must be treated by each student separately (i.e. not in the pair). Practical trainings of the 2nd semester (A1 - A4) alternate with seminars, each working group process the same task at the same time. Organization: 1. 2. 3. 4. 5. 6. 7. 8. 9. use cloakroom (No 418) before you enter the laboratory with laboratory tools only read through all instructions related to your task think about individual steps of the instructions and their order follow the instructions step by step make notes about an experiment during your work (e.g. measured values, possible differences from the instructions,...) wash used laboratory utensils, put your working place in order wash your hands by soap, or in a desinfectant solution if necessary, before you leave the laboratory treat your laboratory report let to check the report by your teacher Compensation of a practical training: If you miss a practical training because of relevant reasons, you may compensate it with the other group of English curriculum, but you should ask competent teacher for the compensation (! each working place for the compensated task is not free in all cases!). The last possibility to compensate any missed practical training is during an examination period (winter one for tasks of the 1st semester; in a summer semester examination period you can compensate only tasks of the 2nd semester). The date for compensation will be known at the end of each semester, see chemistry notice board. No other compensation is possible. All practical trainings must be fulfilled by the end of summer semester, a date for reports submission will be given by your teacher. Literature Everything you need for the practical trainings preparation is found in this document and in the text Laboratory Safety Regulations (see internet). The html version of the instructions, see http://www.lf3.cuni.cz/chemie/english/practical_trainings/index.htm, includes more pictures for better understanding of the procedures. More information related to each task is found in the istructions as either direct internet links or references of the other recomended literature. Printed procedures of all tasks are available in the laboratory, it is not necessary to bring own copy of the instructions. Chemical calculation, related to the practical trainings, you can exercise using the other study material found on the web site: http://www.lf3.cuni.cz/chemie/english/1_year/module_B/1_year_B.htm 3 Serum protein electrophoresis (A1) INTRODUCTION Protein electrophoresis is a well established technique routinely used in clinical laboratories for screening of serum and some other fluids for protein abnormalities. The separation of proteins, primarily accrording to their charge at given pH, is performed on a suitable support medium, e.g. agarose gel. The protein components of plasma or serum constitute almost all the mass of the serum solutes (approximately 80 g/L). The proteins perform a number of functions: carrier proteins, antibodies, enzyme inhibitors, clotting factors, and so on. Serum is the specimen of choice. Plasma can be also used; however, an extra band produced by fibrinogen will be observed (approximately 3 g/L) - a protein that is absent from serum. Serum proteins are commonly classified according to the electrophoretic separation into 6 classes because the agarose gel electrophoresis separates all the proteins to the six fractions: 1. 2. 3. 4. 5. 6. albumin (ALB) alpha-1-globulins alpha-2-globulins beta-1-globulins beta-2-globulins gama-globulins The total serum protein concentrations or the proportions of the individual protein fractions change during a variety of diseases: the electrophoretic analysis is commonly used in diagnostics of diseases. Urine and cerebrospinal fluid can also be analyzed but only after previous increase of their protein concentration made by ultracentrifugation, or other special techniques. The fluids must be concentrated because they contain less proteins than blood serum does. USED METHOD Electrophoretic analysis is based on the separation of proteins in an electric field according to their relative electrophoretic mobility. When an electric field is applied to a medium containing charged particles, the negatively charged particles migrate toward the positive electrode (anode), while the positively charged particles migrate toward the negative electrode (cathode). Supporting media fall into two main classes: 1) supports which allow separation of molecules solely on the basis of net molecular charge (e.g. cellulose acetate, agarose gel); 2) supporting media exerting a sieving effect on the compounds being separated (e.g. polyacrylamide gel): the gel can be considered as a porous medium in which the pore size is of the same order as the protein molecules. The result is that a molecular sieving effect is observed in addition to the electrostatic separation and hence the resolution power of these gels is much greater: there are about 25 or more serum proteins bands observed on polyacrylamide gel in comparison with six bands observed on agarose gel. The many bands seen with polyacrylamide support medium present a complex picture that is hard to interpret and appears to help little in routine clinical laboratory diagnosis. Except for specialized purposes, polyacrylamide cannot be recommended for routine serum protein electrophoresis. The separation is commonly carried out at pH 8.6, which is higher than the pI (= isoelectric point pH) values of the major serum proteins. Proteins are amphoteric molecules: they are either uncharged or negatively or positively charged particles, depending on the pH of a buffer used for analysis. The buffer helps to maintain a constant pH, and it ensures that each protein will maintain a constant charge throughout the course of the separation. If the buffer of pH 8.6 (commonly barbital or Tris-barbital buffer) is used the most of proteins are negatively charged and move toward the anode at a rate dependent on their net charge. Major peaks (bands) observed in order of their migration are those of albumin, alpha-1 globulins (1), alpha-2 globulins (2), beta-1 globulins (β1), beta-2 globulins (β2) and gamma globulins (). Albumin has the highest mobility from all of the fractions. Some of these peaks represent many of different proteins that have a similar migration rate at pH 8.6. However, certain proteins predominate in each peak and variation in their relative amounts is characteristic of certain diseases. In practice, it is desirable to have rapid separation of proteins to preserve sharpness of the bands. The longer the electrophoresis is allowed to proceed, the greater the radial diffusion and the broader the bands. One can decrease 4 the time for a given separation by either decreasing the length of the support or increasing the voltage. With an increase in voltage, there will be a corresponding current increase, and heating may become a limiting factor because of protein denaturation. One way of reducing heating is by lowering of the ionic strength of the buffer. Use of constant voltage is a standard practice in serum protein electrophoresis: separation is achieved within about 30 minutes at about 90 to 100 volts. The separated proteins are fixed (by acid / alcohol mix or by hot air) in the support medium. Fixation causes precipitation of the separated proteins. Staining the proteins (e.g. by amidoblack solution; the medium should be dried in an oven before the staining to evaporate the previous solvent) and subsequent scanning is the most popular method of quantitation of individual protein fractions. Densitometer is used for scanning of separated proteins in a gel, see Fig. 1. Scanning the pattern gives quantitative information about well-resolved protein fractions only. Observation with an experienced eye is helpful in the detection of minor fractions and unsatisfactory separations. Fig. 1: Separated protein fractions of blood serum are represented on the left side. Densitometer graph is illustrated on the right side. Note: Beta-fraction can be separated into beta-1 and beta-2 globulins in agarose gel. Six peaks will be in densitometer graph. Major proteins found in each fraction The list below summarizes principal proteins of each of the fractions, and proteins found between the neighbouring fractions - in interzones (the proteins are of lower concentration than the proteins of individual fractions). Albumin is synthesized in the liver. Its serum concentration is 35 - 55 g/L and half-life 20 days. Albumin is very important binding and transport protein of numerous substances (fatty acids, hormones, bilirubin, drugs, metals). This protein is also included in controlling the fluid balance between intravascular and extravascular compartments of the body (maintenance of oncotic pressure). Albumin is a one of buffer systems in blood plasma. - increased: dehydration - decreased: liver disease, chronic infection, kidney disease, malnutrition, monoclonal gammopathies Albumin /alpha-1 interzone Alpha 1-lipoproteins (= high density lipoproteins, HDL) participate in transport of cholesterol and fat-soluble vitamins. - increased: hyperlipidemia - decreased: liver disease Alpha 1-fetoprotein is an oncofetal antigen synthesized early in fetal development. - increased: liver carcinoma Alpha 1-acid glycoprotein (orosomucoid) is a glycoprotein synthesized in the liver. - increased: in response to a variety of acute and chronic inflammatory stimuly - decreased: if the liver proteosynthesis is damaged 5 Alpha-1 globulins Alpha 1-antitrypsin (= alpha 1-protease inhibitor, API) is an inhibitor of proteolytic enzymes (e.g. trypsin) derived from leucocytes, bacteria, or endogenous production. This substance belong among „acute phase reactants (proteins)“. - increased: acute inflammatory reactions - decreased: hypoproteinemia, inherited conditions Alpha-1 /alpha-2 interzone Alpha 1-antichymotrypsin is an inhibitor of proteolytic enzymes. - increased: acute inflammatory reactions Alpha-2 globulins Alpha 2-macroglobulin is also inhibitor of proteolytic enzymes. Its concentration is dependent on age (higher in childhood). - increased: nephrotic syndrome - decreased: rheumatoid arthritis, myeloma Haptoglobins are a group of proteins that bind free hemoglobin (Hb) to form complexes that are metabolized in the reticuloendothelial system. Hb-haptoglobin complexes preserve the body´s stores of iron for reutilization. - increased: acute and chronic inflammation - decreased: liver disease, hemolytic anemia Beta-1 globulins Transferrin is a major iron-transporting protein in plasma. It transports iron from the intestine and between sites of synthesis and degradation of hemoglobin. - increased: iron-deficiency anemias - decreased: liver diseases, malnutrition, inflammatory conditions, malignance Beta-1/beta-2 interzone Beta-lipoproteins (= low density lipoproteins, LDL) participate in transport of cholesterol. - increased: hyperlipidemias - decreased: starvation Beta-2 globulins C3 fraction of complement is a component of the complex system of serum proteins involved in inflammatory reactions. - increased: acute stress of organism - decreased: active stages of autoimmune diseases (formation of immunocomplexes) Gamma globulins are immunoglobulins synthesized in plasma cells; their are mainly of IgG class. Ig M is found around the „start“ of electrophoresis. - increased: polyclonal (or monoclonal) gammaglobulinemia, liver disease, chronic infections - decreased: small children, hypoimmune syndrom Monoclonal immunoglobulins (paraproteins) can be found in a different position: between alpha-2 and gamma fraction. These proteins are synthesized by beta-cells during multiple myeloma or leucemia. Normal values for individual major electrophoretic serum protein zones: fraction albumin alpha-1 globulins alpha-2 globulins beta-1 globulins beta-2 globulins gamma globulins % 56 - 66 2-3 8 - 12 7 - 10 3-6 10 - 18 Using of electrophoresis in clinical practice Serum protein electrophoresis is a simple technique that is helpful in establishing a diagnosis of monoclonal gammopathies, liver cirrhosis, renal failure, hypogammaglobulinemia, and so on. 6 An „immediate response“ that occurs with stress or inflammation caused by infection, injury or surgical trauma shows decrease of albumin and increase of alpha-1and alpha-2 globulin fractions (acute phase proteins are selectively increased). A „late response“ is correlated with infection and shows an increase in the gamma globulin band due to an increase in immunoglobulins; albumin is decreased and alpha-2 globulin band is increased. An electrophoretic pattern with extremely low intensity of gamma fraction (hypogammaglobulinemia) is observed when an immunosuppressive disease is present. In hepatic cirrhosis there is a broad elevation of the gamma globulins with reduction of albumin (polyclonal gammopathy). Monoclonal gammopathies are due to the clonal synthesis of a unique immunoglobulin and give rise to a sharp gamma globulin band. Nephrotic syndrome shows a selective loss of lower molecular weight proteins: the pattern shows a decrease in albumin (65 kDa) and gamma globulin bands, but a retention of the alpha-2 band composed of the higher molecular protein (alpha-2 macroglobulin, 725 kDa). Hemolytic serum shows fraction of hemoglobin: increased beta band. Literature: ● Engliš, M.: Novinky v medicíně 55: Interpretace elektroforézy plazmatických bílkovin v agarózovém gelu, Avicenum, Praha, 1992 ISBN 80-201-0170-5 ● Tichý, M.: Laboratorní analýza monoklonálních imunoglobulinů (paraproteinů), 1997 ISBN 80-902022-1-7 ● Manuál: Elektroforéza bílkovin - SEBIA K20 REQUIRED KNOWLEDGE Principle of electrophoresis, using electrophoresis in medicine, plasma proteins - classification, function, concentration, difference between plasma and serum PROCEDURE The practical training A1 is only demonstrative, you will not work out a report. Volunteers of students can try the finger capillary blood collection - their blood will be used for the laboratory analysis. Laboratory technician will demonstrate the serum protein electrophoresis. Equipment: equipment for capillary blood collection, centrifuge, applicator carrier, electrophoresis chamber, power supply, tanks for chemical agents (fixation, staining, destaining), gel holders, incubator – držet, pipettes, litter bag, gauze Chemicals: agarose gel Tris-barbital buffer pH 8.5 amidoblack solution with 10% acetic acid (staining solution) destaining solution (contains 0.05 g/dL citric acid) fixative solution (contains 60% ethanol, 10% acetic acid and 30% distilled water) A) Finger capillary blood collection Use gloves in case of blood manipulation ! Equipment: synthetic tips + glass capillaries, holder, lancets, disinfect solution, centrifuge, gauze, plaster, litter bag 7 Procedure: 1. before the blood collection "patient" should toast the hand by hand dryer (to stimulate blood flow to the fingers). 2. disinfect the nygma place (to avoid soreness, choose a site on the side of the fingertip). The surplus disinfect solution has to be removed to prevent the blood hemolysis. 3. remove the protective cap of a lancet and twist in one movement (a full turn). 4. the lancet should be rest gently but firmly against the finger. For those with thicker skin the lancet can be pressed harder against the finger. Press and release the button in one quick movement. 5. collect the blood drop by drop into the synthetic tip (it is necessary to fill the tip approx. in 75%). You can use a class capillary (in synthetic tip) for easier blood collection. 6. cover the blood sample and tap down the blood. Put it to the holder and leave it for 10 minutes (blood coagulation). 7. put the tip with blood to centrifuge for 5 minutes in 4000 RPM for separation of serum. 8. in case of impossibility to separate serum use metal wire to separate the coagulum out of the wall of the tip. Then repeat the centrifugation for 3 minutes. B) General procedure of the technique 1. apply 10 l of serum into the applicator wells 2. applicator contacts the gel surface for 40 seconds 3. put the gel into electrophoresis chamber, according to the polarity indicated on the gel 4. migration of proteins in chamber for 22 minutes at constant voltage 90 V and initial current 12 mA 5. after migration, unplug the chamber and remove the gel plate 6. immerse the gel in the fixative solution for 15 minutes 7. dry the gel at 80oC in air flow incubator-dryer 8. immerse the dried gel in the staining solution for 4 minutes, and destain backround until it is completely colorless and clear 9. hot air fixation of gel 10. evaluation by eye of the protein fraction intensity Task: Evaluate the separated fractions with help of assistant. QUESTIONS The practical training is related to the lectures and seminars: Analytical methods - electrophoresis, centrifugation (summer semester) Structure of amino acids and proteins (winter semester) Composition of blood plasma (summer semester) Expected knowledge of students: the principles of electrophoresis and the centrifugation functions of proteins in a human body structure of proteins, including structures of 20 amino acids found in proteins posttranslational modifications of proteins physicochemical properties of proteins degradation of proteins, including fate of amino group released from amino acids (briefly) proteins of blood plasma and their functions (overview) 8 Examination of urine, urinary sediment (A2) INTRODUCTION Function of kidneys and formation of urine Kidneys eliminate wastes from the body, regulate blood volume and pressure, control levels of electrolytes and metabolites (homeostasis) and regulate blood pH. These processes are vital to life. Kidneys play a role in the endocrine system (e. g. synthesis of erythropoietin). About 1500 litres of blood are filtered through kidneys daily. 150 – 180 litres of ultrafiltrate are formed, approximately 99% of ultrafiltrate is reabsorbed (mainly water) and result is only 0.5 - 2.0 litres of urine excreted per a day (healthy adult excretes 1.5 L of urine daily). Kidneys also play role in an intermediary metabolism (gluconeogenesis and degradation of amino acids). Nephron is the basic structural and functional unit of the kidney. Glomerular filtration and tubular resorption occur in the nephron. Composition of urine Water and water-soluble compounds are excreted with urine. The volume of urine and its composition depends on diet, body weight, age, gender, physical activity, state of health and environmental conditions (temperature and humidity). An adult human produces 0.5 - 2.0 L urine per day (in average 1.5 L). Approximately 95% of the volume of normal urine is due to water. Urine contains organic and inorganic components (see table 1). Organic components in urine N-containing compounds are the most important physiologic organic components of urine: ● urea is synthesized in the liver (urea cycle) from NH 3 which comes from degradation of amino acids. An amount of excreted urea depends on protein metabolism (e. g. degradation of 70 g proteins yields 30 g urea per day). ● uric acid is the final product of endogenous and dietary purine nucleotide catabolism. Renal excretion of uric acid involves 4 pathways - filtration, reabsorption, secretion, and postsecretory reabsorption. Uric acid is freely filtered at the glomerulus. An active anion-exchange process in the proximal tubule reabsorbs most of it. Most urinary uric acid appears to be derived from tubular secretion. Overall, 98-100% of filtered uric acid is reabsorbed and only 6 - 12 % of filtered uric acid is secreted and ultimately appears in the final urine. ● creatinine is a product of muscle metabolism. Creatinine is formed nonenzymatically from creatine by irreversible reaction. Creatinine is freely filtered at the glomerulus (90%) into the ultrafiltrate and 10% of creatinine is secreted by tubule. It is not reabsorbed by the tubules. The amount of creatinine excreted per day is constant at given individual and it is directly proportional to muscle mass and function of glumerules. It can be used as a reference for the quantitation of the other components of the urine. Extent of excreted amino acids is strongly dependent on diet and liver function. Modified amino acids in proteins with specialized function i. e. hydroxyproline in collagen or 3-methylhistidine in actin and myosin can serve as indicators of the proteolysis of the skeletal muscle proteins. Some metabolites can be conjugated with H2SO4 → sulfates, glucuronic acid, glycine and futher polar compounds. These conjugates are synthesized in biotransformation reactions in the liver and they are water-soluble compounds which can be excreted with urine. Metabolites of hormones (catecholamines, steroids, serotonine) also appear in urine. Determination of hormone metabolites in the urine can give an information about production of hormones mentioned above i. e. determination of vanilmandelic acid or 5-hydroxyindol-3-ylacetic acid etc. Another example is human chorionic chonadotropin (hCG, Mr = 36 000). hCG is a proteohormone formed at the beginning of pregnancy. It circulates in the blood and also appears in urine (because its molecule is small). The immunological determination of hCG in the urine forms the basis of a pregnancy test. Urobilinogen (UBG) is a component of urine in a small amount. Urobilinogen is formed from bilirubin in small intestine. Urobilins (bile pigments) are products of urobilinogen oxidation. Variations in concentrations of physiological components of the urine and occurrence of pathological components are used as indicator for diagnosis e. g. glucose and ketone bodies in the case of diabetes mellitus (DM). 9 Proteinuria is a pathologic amount of proteins (mainly albumin) in the urine (more than 0.15 g / 24 hours). Glomerular dysfunction (e. g. glomerulonephritis, bacterial infection, chemical poisons) can lead to proteinuria. Glycosuria means the presence of glucose (Glc) in urine. Glc is freely filtered to the ultrafiltrate at any blood glucose level (glycemia). Reabsorption of Glc increases with growing glycemia but only up to 10 mmol/L. This value leads to saturation of glucose receptors and reabsorption does not increase. Presence of glucose in the urine (glycosuria) increases a diuresis (e. g. diabetes mellitus). Ketonuria means the presence of ketone bodies in the urine (acetoacetate is detected). Ketone bodies (acetoacetate, β-hydroxybutyrate) can appear in urine in case of starvation or diabetes mellitus. Inorganic components of urine Urine contains significant amounts of cations: Na+, K+, Ca2+, Mg2+, NH4+ and anions: Cl-, SO42-, HCO3- and HPO42and trace amounts of other ions. Excretion of ions is mostly regulated by hormones. Amount of various inorganic components varies with diet. Resorption of most of ions Na+, K+, Cl-, HCO3- etc. occurs in proximal tubule. Phosphates and ammonia are buffer systems in urine. Tab. 1: Overview of physiologic concentrations of several analytes in the urine and their relation to metabolism. analyte urea creatinine uric acid physiologically (mmoL/day) 67 - 580 8 - 18 1.5 - 4.4 note MOSTLY relation to metabolism waste product of amino acid degradation waste product of muscle metabolism end-product of purine degradation Na+ 119 - 208 MOSTLY main cation in ECF Cl119 - 208 MOSTLY main anion in ECF K+ 40 - 120 main cation in ICF phosphates 12.9 - 42.0 buffer system in urine Ca2+ 2.5 - 6.2 in bones and blood 2+ Mg 3-5 important in ICF osmolality 500 - 1 200 concentration of osmotically effective particles (Values of concentrations were assumed from Národní číselník laboratorních položek - NČLP na CD-ROM MZČR) Obtaining a urine sample Urine is easily available biological material. We use either first morning urine sample or timed urine collection (e. g. 24 hours) for examination. The rules of first morning urine collection („lege artis“): 1. Patient is quiet overnight. 2. It is important to first clean genitalia before urine collection. 3. As patient starts to urinate, lets some urine fall into the toilet, then collect urine in the container provided, then void the rest into the toilet. This type of collection is called a midstream collection. The container must be clean and dry. 4. Urine sample must be taken to laboratory until 1 hour. Urinary sediment Urinary sediment is a term including microscopic examination of urine. It is a common test of urine that is carried out with chemical analysis simultaneously. A fresh urine should be used to determination of urinary sediment. Examination of urinary sediment evaluates the presence and number of erythrocytes, leukocytes, epithelial cells, bacteria, casts (cylinders) or crystals. Urinary sediment may contain organ and nonorgan components - see tab. 2. Cells are organ components of urinary sediment. These cells can be plasma cells or cells of urinary tract. Erythocytes, neutrophils, eosinophils, macrophages and lymphocytes can be components of urinary sediment. Cells of renal origin (epithelial cells) are typical components of urinary sediment. Urinary sediment may contain futher cells: trichomonas, yeast, intestinal epithelial cells or tumor cells. 10 Casts (cylinders) are small cylinder-shaped formations of cells (leukocytes, erythrocytes, epithelial cells, bacteria) associated with glycoprotein. This glycoprotein protects the inner surface of tubule. The presence of casts in urinary sediment always means seriously affected kidney. The nonorgan components are crystals of salts (oxalates, urates, phosphates). Another group are crystals of small amino acids - cystine, leucine, tyrosine. Crystals are pathological components which are found in the case of urolithiasis. Note: Urolithiasis (greek lithos = stone) is the process of forming stones in the kidney, bladder, and/or urethra (urinary tract). Kidney stones can be composed of calcium oxalate, calcium or ammonium phosphate or crystals of urate. Many clinical laboratories apply a staining of urinary sediment. Tab. 2: Overview of components of the urinary sediment with their physiologic values and causes of increased concentrations component erythrocytes leukocytes squamous (flat) epithelial cells simple cuboidal epithelia cells hyaline cylinders physiologically / l up to 5 up to 10 up to 15 from renal tubules - damaged kidneys no in the case of dehydration granulated cylinders no bacteria yeast urate uric acid oxalate Ca2+ phosphate carbonate amorphous crystals cause of increased concentration various diseases of kidneys and urinary tract (bleeding) acute and chronic inflammation of urinary tract from epithelia of urinary tract (they have not a clinical significance) up to 40 no in the case of dehydration from fruit in the case of dehydration they are casts formed from denaturated proteins (in tubules or collecting ducts) granula = rests of cellular membranes fixed on hyaline cylinders - damaged glomerules infection or contamination beware of confusion of erythrocytes! (mainly in older urine of diabetics) in the alkaline urine (NH4+) in the acidic urine in the acidic and neutral urine in the alkaline and neutral urine in the alkaline urine in acidic urine: urate, Na+, K+, Ca2+, in alkaline urine: phosphates Ca2+, Mg2+, carbonates (Data number./l were assumed from textbook MZ ČSR: Nejedlý, B; Tobiška, J.; Zahradníček, Z.: Základní a morfologické vyšetření moče) Creatinine clearance test In renal physiology, creatinine clearance (Ccr) is the volume of blood plasma (mL) that is cleared of creatinine per unit time (sec). Clinically, creatinine clearance is a useful measure for estimating the glomerular filtration rate (GFR) of the kidneys in mL/sec. Clearance is a ratio of the mass generation and concentration at a steady state. Creatinine is freely filtered at the glomerulus and it is not reabsorbed by the tubules. The amount of produced creatinine is relatively constant, being directly proportional to the body surface area. Creatinine clearance can be calculated if values for creatinine serum concentration (c s), creatinine urine concentration (cu) and urine flow rate (V/t) are known. Generally, timed urine collection (24 hours) or fractional urine collection (3 hours) are performed. Amount of excreted creatinine corresponds to the amount of filtered plasma. Creatinine clearance can be corrected to body surface area of 1.73 m2 - see tab. 3. formula: Ccr (mL/s) = cu / cs x V / t V / t = urine flow (mL/s) 11 Tab. 3: Physiological values of creatinine clearance (Ccr) in v mL/s and mL/min corrected to body surface area (1.73 m2) Ccr, (mL/s, /1.73 m2) 1.05 -1.52 1.23 -1.97 Age group Infants: 6 - 12 mounths Children: 1 - 3 years 3 - 13 years Adults: women 1.57 - 2.37 (average: 1.88) 1.58 - 2.67 Ccr, (mL/min, /1.73 m2) 63 - 91 74 -118 94 - 142 (average: 113) 95 - 160 men 1.63 - 2.60 98 - 156 (Creatinine clearance data were assumed from textbook: Masopust, J.: Klinická biochemie – požadování a hodnocení biochemických vyšetření I. a II. díl, Univerzita Karlova, Karolinum, Praha, 1998) USED METHOD Examination of urine and urinary sediment Physical examination of urine Physical characterics that can apply to urine include volume, density, colour, turbidity, foam and smell. Normal diuresis is about je 1500 mL per 24 hours. Density is about 1.015 - 1.030 g/mL. Colour of normal urine is usually light yellow but varies according to recent diet. The yellow colour of urine is due to presence of a yellow pigment, urochrome. Concentrated urine (low hydration!) is more darker. Clear yellow colour is caused by vitamin B intake. Dark yellow and yellow-brown colour is given by presence of bilirubin; red and brown colour is due to blood (hemoglobin) and porhyrins. Oxidation of urobilinogen produces urobilin → normal urine is darker due to urobilin. Normal urine is transparent or clear; becomes cloudy upon standing. Cloudy urine (turbidity) may be evidence of salts (crystals), bacteria, erythrocytes, leukocytes or epithelial cells. Foam is created by agitation of solution due to presence of proteins, foam is yellow-brown in presence of bilirubin. Smell (or "odour") is due to the breakdown of urea to ammonia. An intensive smell is due to bacteria (formation of ammnonia). Chemical examination of urine Quantitative analysis is mostly carried out in timed urine collection (most often 24 hour). Detected concentration of analyte is converted to "loss" of given substance in the urine per 24 hours. It is necessary to know an exact value of volume of urine. Urea and sodium chloride are the most quantitative components of the urine. Semiquantitative analysis is used as a common screening. This is a fast but only orientation determination of components in the urine. This basic chemical examination is carried out by diagnostic (PHANs): test strips are plastic strips to which chemically specific reagent pads are affixed. Number of reagent pads is different on PHANs e. g. GlucoPHAN has one reagent pad for detection of glucose in the urine. HeptaPHAN test strips are simple, easy to use reagent strips for the detection of 7 key diagnostic chemical markers in human urine (pH, proteins, glucose, ketone bodies, urobilinogen, bilirubin, blood, hemoglobin - see tab. 4). Strip is immmersed in urine sample for 1 – 2 seconds. After about 1 minute we compare the color change of reagent pads to the corresponding color chart (scale) on the bottle label. We evaluate the intensity of color change by units (0 - 4; 0 = negative, 4 = massive concentration), only pH value is written out. Tab. 4: Reagent pads on HeptaPHAN test strips reagent pad pH proteins glucose ketone bodies urobilinogen bilirubin erythrocytes hemoglobin physiologically 5-6 0 0 0 0 0 0 0 principle of reagent pad acid-base indicator (pH = 5 - 9) note pH > 8 is due to bacteria indicator is sensitive to albumin glucose oxidase / peroxidase → chromogen more sensitive to acetoacetic acid than acetone sensitive to UBG and stercobilinogen vit. C does not matter beta-OH-butyrate does not react ↑ vit. C → false ↓ azo-coupling (the same at UBG) peroxidase activity Hb → oxidation of indicator (Hb from broken erythrocytes) 12 strong bacterial contamination → ↑ pH - urinary pH may range 4.5 - 8.0, urine from healthy individuals is weakly acidic pH = 5 - 6, acidity of urine depends on state of metabolism, e. g. vegetarian diets increase alkalinity pH = 7 – 8; bacterial infections also increase the alkalinity due to NH4+ Proteins - small amount is present in the urine (up to 0.1 g/L), physical exercise increases the excretion (up to 5 g/L!); physiological value of excreted proteins is 150 mg per a day, proteinuria appears if the amount of excreted proteins > 150 mg Glucose - small amounts of Glc may be excreted by kidney (up to 0.8 mmol/L); higher amount = glycosuria; glucose threshold in kidneys is 9-10 mmol/L (if this level is got over glucose is excreted with the urine); glucose is decreased in the urine in the case of presence of bacteria Ketone bodies - include acetone (2 %), acetoacetate (33 %) and β-hydroxybutyrate (65 %) - in total < 1.5 mmol/L; higher amount of ketone bodies is associated with increased breakdown of fatty acids (i. e. starvation, diabetes mellitus). Urobilinogen - is a colourless product of bilirubin reduction. It is formed in the intestines by bacterial action. Part of it is resorbed and returned to the liver, while the rest is excreted in feces (= enterohepatic circulation). Trace amounts can be detected in urine. Physiological value is less than 17 µmol/L. Bilirubin - if it is present in the urine (pathological value in the case of bilirubinemia above 30 - 34 µmol/L), only „conjugated bilirubin“ is water-soluble → this bilirubin is excreted only with bile under physiological conditions; nonconjugated bilirubin is water-insoluble → it is transported in complex with albumin; bilirubin comes from breakdown of hemoglobin, bilirubin is yellow-orange Blood - should not be detected under physiological conditions; cause can be physical trauma, glomerulonephritis, kidney stones Detection of urinary sediment Urine sample is centrifuged for 10 min at 2000 RPM. Supernatant is sucked up by suction pump and sample is concentrated 10x. Sediment is mixed thoroughly and pipetted 40 l of it to the special chamber used for microscope. A plastic slide contains several chambers. These chambers create a grid and this grid enables the quantitative evaluation of the urinary sediment i. e. number of particular elements in 1 l of urine. The sediment is inspected at magnification 400 to 450x. Literature: Masopust, J.: Klinická biochemie: Požadování a hodnocení biochemických vyšetření. Karolinum, Praha, 1998. ISBN 80-7184-649-3 Koolman, J., Rőhm, K.-H.: Color Atlas of Biochemistry, Thieme, Stuttgart, 1996. ISBN 1-58890-247-1 Němečková, A. a kol.: Lékařská chemie a biochemie, Avicenum, Praha, 1991 Štern, P. a kolektiv autorů: Obecná a klinická biochemie pro bakalářské obory studia, Univerzita Karlova, Karolinum, Praha, 2005. ISBN 80-246-1025-6 Nejedlý, B., Tobiška, J., Zahradníček, Z.: Základní a morfologické vyšetření moče, Ministerstvo zdravotnictví ČSR Manuál: Diagnostické proužky PHAN, Lachema, Brno, 1996 REQUIRED KNOWLEDGE Function of kidneys, structure of nephron, formation of urine - glomerular filtration and tubular resorption, influence of hormones upon function of kidneys, composition of urine. PROCEDURE Your task is to examine 3 urine samples: samples No. 1 and No. 2 (in plastic bottles on the table) and No. 3 = your own urine in container. Chemical examination of urine is carried out in all 3 samples simultaneously. Sample of your own urine (No. 3) is tested by chemical and microscopic analysis (urinary sediment). Centrifuge test tube is filled up to the mark with a sample No. 3. 13 Practical training is composed of 3 tasks: task 1: Chemical examination of urine by diagnostic test strips HeptaPHAN and chemical reagents task 2: Detection of urine elements (urinary sediment) task 3: Creatinine clearance test Equipment: 6 graduated test tubes + 1 centrifuge test tube, holder , container, diagnostic test strips HeptaPHAN, plastic slide with chambers, microscope, water bath, litter bag, wash bottle, gauze Chemicals: sulfosalicylic acid solution Fehling´s reagents I and II (in dosing bottles) Lestradet´s reagent (sodium nitroprusside) 2 urine samples (in plastic test tubes) your own urine sample (container) Task 1: Chemical examination of urine A) Diagnostic test strips Heptaphan for determination of pH, glucose, urobilinogen, bilirubin, ketones and blood in urine First of all see instructions on the last page of the procedure found on your working table. 1. mix all samples thoroughly by 3 turning of each tube by 180 degrees and back (DO NOT shake) 2. remove one test strip and reseal the strip box immediately after use. Completely immerse all reagents pads in specimen (no longer than 1-2 seconds). 3. run edge of the strip against rim of urine container to remove excess urine, hold or place the strip in a horizontal position 4. after about 60 seconds compare the tests pads for pH, protein, glucose, urobilinogen, bilirubin, ketones and blood to corresponding color scale on the label 5. use the scale of evaluation: 0 / 1 / 2 / 3 / 4 (0 = negative, 4 = the most positive finding) B) Detection of proteins by sulfosalicylic acid 1. put 2 mL of urine to 3 test tubes 2. add about 10 drops of sulfosalicylic acid, mix the content evaluation: Proteins found in urine are precipitated by sulfosalicylic acid. We evaluate the intensity of turbidity (or appearance of the precipitate) against a dark backround.The turbidity of urine must be compared to original urine sample. Evaluation after addition of sulfosalicylic acid: no turbidity = 0 transparent turbidity (possibility to read through it) = 1 stronger turbidity (without possibility to read through it) = 2 "milk" turbidity or flake = 3 curdy precipitate = 4 C) Detection of glucose by Fehling´s reagent 1. put 1 mL of Fehling´s solution I and 1 mL of Fehling´s solution II in all 3 test tubes 2. add 2 mL of urine sample to the each test tube, mix them 3. place the test tubes into the hot water bath (99 °C) for 2 minutes at least evaluation: formation of precipitate of Cu2O (orange-brown or finally red) in positive reaction D) Detection of ketone bodies by Lestradet´s reagent (sodium nitroprusside) 1. put 3 small piles (one for each urine sample) of Lestradet´s reagent on the filter paper and mark them 2. add 1 - 2 drops of urine sample to each pile evaluation: violet-red colouring in positive reaction 14 Your report should contain clearly organized table containing results of the examination of all 3 urine samples by both the strips and chemical analyses. Task 2: Detection of urine elements (urinary sediment) Procedure: 1. fill a centrifugal test tube with a sample of your own urine (sample No. 3) up to the upper mark (= 10 mL) 2. centrifuge the test tube for 10 minutes (2000 RPM) 3. suck up 9 mL (to the lower mark on the test tube) of supernatant to the waste by suction pump in the fume cupboard 4. mix thoroughly the sediment and pipette 40 L of it to the special chamber used for microscope 5. inspect the sediment (magnification 450x): count the number of each type of element per one medium grid area (see the picture next to the microscope; calculate an average number from 10 medium grid areas): evaluation of the urine sediment = number of particular elements within 1 L of urine Describe and draw characteristic formations which are observed. Task 3: Creatinine clearance test Task: Calculate the creatinine clearance for this patient: An adult man excreted 1.5 L of urine per 24 hours. The chemical analysis shows the urine creatinine concentration of 5.98 mmol/L and plasma creatinine concentration of 72 mol/L. Compare your result with reference value of creatinine clearance for adults in tab. 3. QUESTIONS The practical training is related to the lectures and seminars: 1. Biochemistry of kidney (summer semester) 2. Metabolism of saccharides, lipids, amino acids, purines and tetrapyrrols (winter semester) Expected knowledge of students: 1. definition of pH, buffers, acidity of urine (excretion and reabsorption of protons) 2. substances found in urine - their chemical structure, excretion by the kidney, relation to the metabolism: proteins, glucose, urobilinogen, bilirubin, ketone bodies, hemoglobin, urea, uric acid, creatinine, anorganic ions (H+, Na+, K+, Cl-, Ca2+, Mg2+, phosphates) 15 Determination of blood glucose level (glycemia) (A3) INTRODUCTION Glycemia and its maintenance Glucose is the principal circulating monosaccharide in the blood and the major energy source of the cells. Definition: glycemia is blood glucose level (concentration). Normal fasting glycemia is in the range: 3.3 – 6.1 mmol/L. Blood glucose level is regulated by lot of mechanisms. Disorder of these mechanisms can be expressed as hyperglycemia or hypoglycemia. Hyperglycemia is a condition in which an excessive amount of Glc circulates in the blood plasma. It is usually, but not always, associated with diabetes mellitus (DM). Hypoglycemia is decreased blood concentration of Glc less than 2.2 mM (e. g. in case of an overdose of insulin). Hypoglycemia can cause drowsiness, weakness and comatose state. Glycosuria means the presence of glucose in the urine. Glycemia is regulated by hormones. Hormones included in regulation of glycemia are the following: insulin, glucagon, cortisol, catecholamines and growth hormone. Insulin is a peptide hormone synthesized in the islets of Langerhans (beta-cells) in pancreas. If glycemia increases, insulin is secreted into the blood. Insulin influences carbohydrate and lipid metabolism within the cells. Insulin and its influence on carbohydrate metabolism: 1. Insulin promotes Glc entry to skeletal muscle, heart and an adipose tissue (GLUT-4) → ↓ glycemia. 2. Insulin activates glycolysis within the cell 3. Insulin activates glycogen synthesis Generally: Insulin promotes Glc entry to cells from blood and also activates the utilization of Glc within the cell. Defects in insulin secretion or disorders of insulin receptors lead to diabetes mellitus. Glucagon is a peptide hormone produced in the islets of Langerhans (alfa-cells) in the pancreas. Glucagon is secreted if the glycemia is decreased. Target organ of glucagon is liver (an antagonist of insulin). This hormone activates a release of Glc into the blood → ↑ glycemia. Glucagon does not act in peripheral tissues. Glucagon receptors are associated with G-proteins. Glucagon and its influence on carbohydrate metabolism: 1. Glucagon activates the glycogenolysis in the liver → Glc is released into the blood → ↑ glycemia 2. Glucagon activates the gluconeogenesis in the liver → Glc is released into the blood → ↑ glycemia Cortisol is a steroid hormone synthesized in adrenal cortex. This hormone is synthesized from cholesterol. Cortisol belongs among glucocorticoids and activates proteolysis → proteins are hydrolyzed to particular amino acids → these amino acids can be used to gluconeogenesis → Glc → ↑ glycemia. Biochemical tests Basic biochemical information about carbohydrate metabolism is a blood glucose level determination (in whole blood, plasma or serum). Glycemia can be measured in arterial, venous and capillary blood. Determination of blood glucose level is a routine test in clinical biochemistry. An overview of glycemia values is showed in tab. 1. Tab. 1: Overview of fasting blood glucose levels during human life. serum glucose concentration (mmol/L) age until 1 day 2.22 – 3.33 until 4 weeks 2.78 – 4.44 from 4 weeks until 15 years 3.33 – 5.55 from 15 years until 60 years 3.88 – 5.83 from 60 years until 70 years 4.44 – 6.38 from 70 years until 99 years 4.61 – 6.10 (Data were assumed from Národní číselník laboratorních položek - NČLP na CD-ROM MZČR). 16 Fasting glycemia determination (on an empty stomach) Fasting glycemia determination is tested because glycemia is increased after meal and then glycemia returns to normal values. A person fasts overnight (12 hours) before the test. Blood collection is carried out in the morning (7:00 - 8:00 a. m. the best). Glycemia determination after meal (= postprandial glycemia) Blood collection is carried out 1 hour after meal containing saccharides. Glycemic profile Glycemia is often measured at diabetics several times per day: on an empty stomach, after meal and at night (5x or 9x per day, e. g. at 6:00, 12:00, 17:00, 22:00 and at 3:00 o´clock). This determination is used to therapy (e. g. how to dose insulin). oGTT (= oral glucose tolerance test) In the test, a person fasts overnight (at least 8 hours). Then first, the fasting plasma glucose is tested. After this test, the person receives a drink containing 75 g of Glc in 250 – 350 mL of water (during the period 5 – 15 minutes). Blood samples are taken up to four times (after 30, 60, 90 minutes and 2 hours) to measure the blood glucose level. Diabetes mellitus is diagnosed if value of glycemia is higher than 11.1 mmol/L after 2 hours. Values between 8 – 11.1 mmol/L are termed as „impaired glucose tolerance". If the first morning glycemia is higher than 8 mmol/L, oGTT is stopped. Oral glucose tolerance curve can be constructed as dependance of glycemia values and time - see Fig. 1. Fig. 1 was assumed from http://www.mfi.ku.dk/ppaulev/content.htm - Textbook in Medical Physiology and pathophysiology – Section VII: Endocrine Glands in Humans – Chapter 27: Blood glucose and diabetes Oral glucose tolerance curve can be divided into 3 parts: a) Rate of resorption of Glc from intestine shapes the ascending part of curve. A patient with hyperthyroidism has a rapid intestinal absorption and a rapid combustion of Glc. The myxoedematous patient (hypothyroidism) has a slow absorption and a slow combustion of Glc. b) A peak level of curve is dependent on good liver function (glycogen synthesis) and on insulin action in the liver. 80% of resorbed glucose is converted to glycogen in the liver under normal conditions. Blood glucose concentration in portal vein is up to 22.2 mmol/L, while concentration of Glc is maximum 11.1 mmol/L in peripheral tissues. Incresing glycemia stimulates an insulin secretion into the blood. Peak of glycemia is reached in 45 - 60 minutes. Decrease in insulin secretion is typical of beginning insulin-dependent diabetes mellitus. Glucose is not converted to glycogen in the liver sufficiently and peak of glycemia exceeds the value 11.1 mmol/L. 17 c) Descending part of curve is dependent on insulin action and it is a criterion of utilization of glucose. Its disorder (slowed-down and insufficient return to normal values) is a classical manifestation of diabetes mellitus. Disorder is a manifestation of absolute or relative lack of insulin. Literature: ● Devlin, T.M.: Textbook of Biochemistry with Clinical Correlations, 4 th edition, Willey-Liss, Inc., USA, 1997 ISBN 0471-15451-2 ● Masopust, J.: Klinická biochemie: Požadování a hodnocení biochemických vyšetření I a II. díl, Univerzita Karlova, Karolinum, Praha, 1998 ISBN 80-7184-649-3 USED METHOD In practical training A3 glycemia is determined by two 2 manners: a) by glucometer and b) by photometer. Principle of glycemia determination by glucometer GLUCO TOUCH: Glucometer is an apparatus able to measure blood glucose concentration immediately. Only one drop of blood is enough for this fast test. Drop of blood is dropped on a pink area of the test strip. A pink area of the test strip contains enzymes and other chemical reagents needed to reaction with glucose. Glucose in drop of blood is oxidized to hydrogen peroxide and gluconate by enzyme glucose oxidase. Produced H2O2 reacts with another reagent to form a product (blue colour). This reaction is catalyzed by enzyme peroxidase. Glucometer is based on principle of photometry so that intensity of blue colour of product is proportional to blood glucose level. Principle of serum glycemia determination by photometer: Glucose is oxidized by oxygen. The reaction is catalyzed by enzyme glucose oxidase to hydrogen peroxide and gluconate. The H 2O2 is determined by oxidative coupling reaction with phenol and 4-aminoantipyrine. This reaction is catalyzed peroxidase. The amount of arising chromogen (scarlet colour, Amax = 498 nm) is proportional to glucose sample concentration. REQUIRED KNOWLEDGE Structure of glucose - its properties and function, digestion and resorption of saccharides, entry of glucose to cell, utilization of glucose within the cell, overview of basic metabolic pathaways of saccharides, effect of insulin and glucagon on metabolism of glucose, principle of spectrophotometry PROCEDURE Practical training A3 is composed of these parts: A) Finger capillary blood collection B) Glycemia determination by glucometer (in whole blood) C) Serum glycemia determination by spectrophotometer D) Glycemia monitoring after consumption of a sweet drink (only volunteers) Practical training starts with capillary blood collection. First, glycemia is measured by glucometer. The first drop of blood is removed during capillary blood collection and the second drop of blood is dropped to the pink area of the test strip. Then the test strip is inserted into the glucometer and you immediately continue in capillary blood collection to the synthetic tip. Serum is used to glycemia determination by spectrophotometer. Equipment: spectrophotometer, glucometer + test strips, equipment for capillary blood collection, test tubes, pipettes, water bath, litter bag, wash bottle, gauze Chemicals: glucose standard solution (20 mmol/L) reagent (the content: buffer, glucose oxidase, peroxidase, 4-aminoantipyrine, 3-methylphenol) control serum (Lyonorm = animal serum rich with human serum analytes) distilled water pure glucose for preparation of a sweet drink (oGTT) 18 A) Finger capillary blood collection Procedure: 1. before the blood collection "patient" should toast the hand by hand dryer (to stimulate blood flow to the fingers). 2. disinfect the nygma place (to avoid soreness, choose a site on the side of the fingertip). The surplus disinfect solution has to be removed to prevent the blood hemolysis. 3. remove the protective cap of a lancet and twist in one movement (a full turn). 4. the lancet should be rest gently but firmly against the finger. For those with thicker skin the lancet can be pressed harder against the finger. Press and release the button in one quick movement. 5. collect the blood drop by drop into the synthetic tip (it is necessary to fill the tip approx. in 75%). You can use a class capillary (in synthetic tip) for easier blood collection. 6. cover the blood sample and tap down the blood. Put it to the holder and leave it for 10 minutes (blood coagulation). 7. put the tip with blood to centrifuge for 5 minutes in 4000 RPM for separation of serum. 8. in case of impossibility to separate serum use metal wire to separate the coagulum out of the wall of the tip. Then repeat the centrifugation for 3 minutes. B) Glycemia determination by glucometer 1. press the blue power button and take a test strip. Before testing, the confirmation dot (on the back of the test strip) should be off - white. 2. hold the test strip under your finger and touch the drop of blood to the pink area 3. check to see that confirmation dot on the back of the test strip has turned completely blue 4. insert the strip into the glucometer (pink side up) 5. the result (in mmol/L) appears on display in 30 sec. Note your result to the report. C) Serum glycemia determination by spectrophotometer You need a serum sample obtained from capillary blood collection - see point A mentioned above. Preparation of standard glucose solutions: You will need three standard solutions of different concentration (20 mM, 10 mM and 5 mM) for the analysis. Only one of the standards is available: 20 mM solution of glucose. Other standards can be prepared by dilution of the 20 mM solution: 1. prepare 1 ml of 5 mM glucose solution 2. prepare 1 ml of 10 mM glucose solution Use larger plastic test tubes and an automatic pipette for the dilution. Preparation of solutions (blank sample, standards, samples) for the spectrophotometric analysis: 1. mark all test tubes (11 pieces) by water proof marker beforehand 2. each solution (except blank sample) process twice according to the table: test tube No pipetted volume pipetted solution 1 distilled water 10 l (= blank sample) 2,3 5 mM glucose solution (standard) 10 l 4,5 10 mM glucose solution (standard) 10 l 6,7 20 mM glucose solution (standard) 10 l 8,9 Lyonorm (= control sample) 10 l 10,11 own serum 10 l 19 3. add 1 mL of the reagent (use feeder) to each test tube 4. mix thoroughly and incubate the test tubes exactly for 15 minutes in water bath (37 °C) 5. measure their absorbances by the spectrophotometer at 498 nm against the blank sample (the measurement has to be finished up to 40 minutes after the incubation) 6. pour rests of the measured solutions into the waste bottle (next to the spectrophotometer) and put the used test tubes into the special container containing a disinfectant D) Glycemia monitoring after consuming of a sweet drink Immediately after blood collection drink or eat anything sweet (only volunteers). Repeat the finger-capillary blood collection after 30, 60 and 120 minutes. Determine glycemia by glucometer only. Tasks: Create a comprehensive table containing your results (measured absorbances, calculated conversion factor of each standard solution: f = cst/Ast, see Lambert-Beer law, and glucose concentrations). Calculate the average value of the conversion factors. Using the factor calculate the glucose concentration in both your own and control serum and express their concentrations as the average of the duplicate determinations; add the values to the table (see above). Compare the glucose concentration values measured by glucometer and by spectrophotometer. Discuss the differences. Make a note of the time passed from the last eating before the blood collection. Give the glycemia value after consuming of sweet drink and compare it with the initial level. QUESTIONS The practical training is related to the lectures and seminars: Digestion and absorption of basic nutrients - carbohydrates (summer semester) Metabolism of carbohydrates I and II (winter semester) Structure of carbohydrates (winter semester) Analytical methods - spectrophotometry (winter semester) Expected knowledge of students: structure of physiologically important carbohydrates (glucose, fructose, galactose, sucrose, lactose, maltose, starch, glycogen, cellulose) - structural formulas, types of chemical bonds structure of glucuronic acid and gluconic acid digestion of carbohydrates - enzymes, products transport of glucose through cell membranes metabolism of glucose (glycolysis, gluconeogenesis, hexose monophosphate pathway, synthesis and degradation of glycogen, transformation of glucose to other monosaccharides and compounds, e.g. glucuronic acid, glucitol) - substrates, important intermediates, products, regulatory reactions and their regulation, localization in both the cell and the human body effect of insulin and glucagon on metabolism of glucose principle of spectrophotometry 20 Determination of alkali phosphatase (ALP) activity in serum (A4) INTRODUCTION Alkali phosphatase (ALP) is the group-name of relatively nonspecific hydrolytic enzymes. In a case of pH > 7 the ester bonds of H3PO4 can be cleaved by ALP. pH optimum of ALP is about 10.5. R-O-PO32- + acceptor → R – OH + acceptor – PO32ALP occurs in liver, bones, intestine, kidneys and placenta. There are found three isoenzymes: placental, intestinal and tissue nonspecific (= enzymes called as the bone, liver and kidney isoforms). Total ALP activity in blood serum of the health human is given mainly by activity of both hepatic and bone isoenzymes (isoforms). Diagnosis is determined by these isoenzymes because both are present in the blood. ALP does not occur in erythrocytes and leukocytes. Function of ALP ● in transport processes in the liver ● in bones → in bone structure ALP shares on Ca2+ installation (it is a component of membrane of osteoblasts) ● ALP shares on fatty acid transmission and absorption of Ca2+ in intestine Enzyme activity ALP activity is various during a human life. Bone isoenzyme has a higher activity in children until 1 year, then it falls down but the activity is increased in puberty (growing bones). If growth of bones is finished there is a low level of bone isoenzyme - see tab. 1. Elevated activity of bone isoenzyme is due to an increased activity of osteoblasts. We have to know the age of a pacient for ALP activity determination. Half-life break up of ALP is 3 – 5 days, that is different at individual isoenzymes. Tab. 1: Serum total ALP activity in dependence on human age. age until 6 weeks until 1 year until 10 years until 15 years above 15 years activity in serum (kat/L) 1.20 – 6.30 1.40 – 8.00 1.12 – 6.20 1.35 – 7.50 0.66 – 2.20 Serum activity of bone isoenzyme ALP in age group above 15 years is 0.1 – 1.6 kat/L. NOTE: Values of total ALP activity and bone isoenzyme were assumed from Národní číselník laboratorních položek - NČLP na CD-ROM MZČR. Separation of particular isoenzymes Every isoenzyme has a characteristic mobility during electrophoresis. Electrophoresis on cellulose acetate membranes is used to separation of hepatic, bone and intestinal izoenzyme. Placental isoenzyme activity is increased from 16th week of pregnancy. This isoenzyme is thermostabile. An inactivation by heat can be used to separation of isoenzymes. Bone isoenzyme of ALP is inactivated by temperature 56 oC for a period 15 min. Immunochemical methods can be also used to determination of ALP isoenzymes. Clinical significance of ALP The increasing in activity of the hepatic isoenzyme is caused by obstruction of the bile ducts. Hyperparathyroidism and bone fractures cause increasing in activity of bone isoenzyme. Determination of ALP activity in the serum is mainly used to diagnosis of bone and hepatobiliary diseases. Increased ALP activity is caused by: 21 ● hepatitis (viral, chronic, toxic alcoholic) ● liver diseases (alcoholics), biliary obstruction (e. g. tumor), liver cirrhosis, liver cancer (hepatom), mononucleosis ● bone tumors (metastases from a primary tumor of bone cells), osteosarcoma ● bone fractures Determination of ALP activity is a component of general biochemical test of liver and biliary duct function (screening test). This test includes the determination of activity of the following enzymes: ALT, AST, GMT and bilirubin. ALP is also determinated in oncology test or in bone metabolism test (determination of bone isoenzyme ALP). Literature: Masopust, J.: Klinická biochemie: Požadování a hodnocení biochemických vyšetření I a II. díl, Univerzita Karlova, Karolinum, Praha, 1998 ISBN 80-7184-649-3 USED METHOD The ALP activity is determined in serum or plasma (with heparin) by spectrophotometric method. Substrate is 4nitrophenylphosphate (colorless) which is cleaved by ALP to 4-nitrophenol (yellow) and phosphate in N-methyl-Dglucamine buffer. The concentration of 4-nitrophenol (Amax = 405 nm) is proportional to the ALP activity. Enzyme reaction is stopped by NaOH. ALP 4-nitrophenylphosphate (colorless) + H2O → phosphate + 4-nitrophenol (yellow) Because of the heat instability of the bone isoenzyme, its activity can be calculated as a difference of activities before and after thermic inactivation of the sample. REQUIRED KNOWLEDGE Structure, properties and function of enzymes, fundamentals of enzyme kinetics, activity of enzymes - its interference and units, isoenzymes, relationship between enzymes and their organ localization, importance of enzymes in medicine, principle of spectrophotometry PROCEDURE In practical training A4, total ALP activity and activity of bone isoenzyme is determined in serum Lyonorm. Equipment: water bath, float holder, Eppendorfs (plastic test tubes with cover), tubes + holder, automatic pipette (0 - 0.2 mL), spectrophotometer, litter bag, gauze Chemicals: buffer pH =10.4 (reagent No. 2) enzyme substrate (reagent No. 1) stop solution (70 mM NaOH solution) serum (Lyonorm P) Procedure: A) Inactivation of bone isoenzyme of ALP by heat Serum Lyonorm contains total ALP i. e. all isoforms. Mark the Eppendorf tube by the permanent marker and pipette 0.2 mL of serum. Close the tube and incubate it at 56 oC in water bath exactly 15 min (use float holder). Bone isoenzyme of ALP is inactivated by heat and you obtain 0.2 mL of inactive serum. 22 B) Determination of ALP activity in serum 1. process the both serum samples: inactivated (by heat) and without inactivation (= “native”), according to the next manner: Test tube No 1 2 50 μL H2O pipette: 50 μL serum native (blank) (total ALP) 3 4 5 50 μL serum native 50 μL serum inactive 50 μL serum inactive (total ALP) (ALP without bone isoenzyme) (ALP without bone isoenzyme) 2. add 200 μl of buffer and 200 μl of water to each test tube, mix it! 3. preheat 3 min at 30oC in water bath. 4. add 50 μl of substrate to each test tube. Take out always one test tube, add the substrate, mix it and return back to the water bath. The incubation time should be the same for all samples. 5. incubate the test tubes exactly 15 min at 30oC from adding of the substrate (= time for enzyme reaction). 6. add 2 ml of stop solution to stop the incubation (i. e. to stop the ongoing reaction in the mixture), mix the test tube immediately. 7. measure the absorbances of all samples in 405 nm (use the blank sample). 8. pour rests of the measured solutions into the waste bottle (beside the spectrophotometer) and put the used test tubes into the special container containing a disinfectant. Task: Calculate the average of total ALP activity and the average of activity of the bone isoenzyme in serum by use of the information: According to Lambert-Beer law the absorbance of serum of known total ALP activity (3.96 μkat/L) was measured under the same conditions (as in your experiment): A = 0.970. Describe the calculations by that values of ALP activity in all samples were obtained. serum native serum native absorbance average serum inactive serum inactive --------------- ---------------- ALP activity (kat/L) Results: Total ALP activity: ………………… μkat/L Bone isoenzyme activity: ………………… μkat/L Discussion: compare your results with the physiological ranges Serum total ALP activity in age group above 15 years: Serum activity of bone isoenzyme ALP in age group above 15 years: 23 average 0.66 - 2.20 kat/L 0.1 – 1.6 kat/L QUESTIONS The practical training is related to the lectures and seminars: Enzymes and coenzymes I and II (winter semester) Regulation of biochemical processes in the cell (winter semester) Biochemistry of liver cell (summer semester) Expected knowledge of students: structure, properties and function of enzymes nomenclature of enzymes terms: apoenzyme, cofactor, coenzyme, prosthetic group, allosteric site, subunits, proenzymes, isoenzymes, specificity of enzymes fundamentals of enzyme kinetics (Michaelis-Menten equation, Michaelis constant, activity of enzyme and its units, catalytical concentration, modulation of enzyme activity, inhibition of enzymes) compartmentalization of biochemical processes (enzymes of metabolic patways found in different compartments of the cell) and tissue distribution of enzymes (e.g. enzymes of glycolysis are found in all cells but enzymes of urea synthesis are only in hepatocytes; look for other examples) principle of spectrophotometry Last update: 22.2.2007 24