Disclosure What is COPD? Goals of therapy Treatment Strategy
advertisement

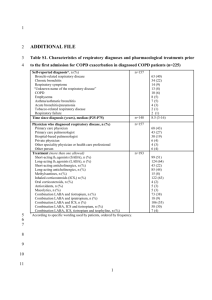
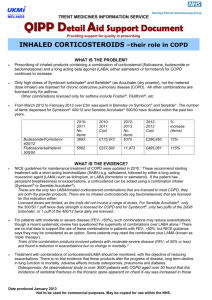
3/25/2013 COPD Management: Maintenance Disclosure Dr. Wheeler has nothing to disclose. What is COPD? Objectives 1 Discuss current guidelines and treatment strategies 2 Discuss the role of pulmonary rehabilitation 3 Discuss the role of oxygen therapy Goals of therapy Include: • Alleviate symptoms of disease Definition: “A preventable and treatable disease with some extrapulmonary effects that may contribute to the severity in individual patients. Its pulmonary component is characterized by airflow limitation that is not fully reversible. The airflow limitation is usually progressive and associated with an abnormal inflammatory response of the lungs to noxious particles or gases” - GOLD guidelines and WHO Treatment Strategy Based on disease severity…. GOLD – Shortness of breath • • • • Prolong time between exacerbations Reduce severity of exacerbations Maximize exercise capacity Improve health status 1 3/25/2013 Treatment Strategy I: Mild II: Moderate III: Severe IV: Very Severe Modified Medical Research Council Dyspnea Scale (mMRC) … assesses shortness of breath Treatment Strategy COPD Assessment Test (CAT) … Sx and QoL Treatment Strategy COPD Combined Assessment … assess risk of We will get there… Classes of Drug Therapy • Smoking Cessation Therapy Beta Agonists Anticholinergics Inhaled glucocorticoids Combination therapies Phosphodiesterase 4 Inhibitors • Vaccinations • • • • • • • • • • Methylxanthines Mucolytics Antitussive Antibiotics Oral steroids 2 3/25/2013 Therapy for ALL COPD Patients Bronchodilators Smoking Cessation ! Beta Agonists and Anticholinergics Vaccinations: • Influenza Vaccination • Pneumococcal Vaccination • Many available IV, PO, INH, SC • INH preferred; maximum direct effect on airways – MDI, DPI or neb Physical Activity • Increase FEV1 – Improved expiratory flow relates to the dilation of the airways Avoidance of Risk Factors Beta Agonists MOA: relaxation respiratory tract smooth muscle via stimulation of β2‐adrenergic receptors causing ↑cAMP thus blocking bronchoconstriction AE: • resting sinus tachycardia; could participate cardiac rhythm disturbances (rare in inhaled formulations) • somatic tremor in elderly (higher doses, inh=oral) • hypokalemia especially when combined with thazides Beta Agonist Drugs Short Acting (SABA) Long Acting (LABA) • Albuterol: Ventolin, ProAir (MDI and neb) 2 INH q4h •Formoterol: Foradil (DPI)* and Performist (neb) •Arformoterol: Brovana (neb) • Levalbuterol: Xopenex (MDI and neb) 2 INH q4h • Pirbuterol: Maxair (MDI) 2 INH q4h •Indacterol: Arcapta Neohaler* (DPI) … 75mcg…? – Once daily; prolonged duration – Rapid onset (NOT rescue) Approved for bronchospasm •Salmeterol (Serevent Diskus)* * FDA approved COPD Anticholinergics Muscarinic Antagonists: Short Acting: (SAMA) • Ipratroprium bromide: Atrovent (MDI) 2 INH QID Long Acting: (LAMA) • Tiotropium : Spiriva (DPI) Inhale contents of one capsule daily MOA: • Blockage of acetylcholine effects on M3 receptors leading to ↓cGMP which blocks constriction Benefits: •Improve lung function, decreases dynamic hyperinflation, dyspnea and exacerbations •LAMA – Additionally improves trough airflow … prolonged effect AE: •Poorly absorbed systemically thus minimal ADE •Dry mouth and cough, nausea, blurred vision •Ipratropium associated with bitter, metallic taste (some pts) •Neb solutions used with face masks :precipitation of acute glaucoma (eye exposure) New Drug Aclidinium bromide (Tudorza): Dose: 1 inhalation twice daily Detectable in blood within 10 minutes of inhalation Primarily metabolized via hydrolysis to inactive metabolites 1% excreted unchanged drug Half‐life of 5 to 8 hours No dose adjustments for renal or hepatic insufficiency Does NOT inhibit CYP450 enzymes Adverse effects: – Headache (6%) – Nasopharyngitis (5%) – Cough (3%) • Warnings: paradoxical bronchospasm, worsening narrow angle glaucoma, urinary retention • • • • • • • • 3 3/25/2013 Preferences? • SABA = rapid onset to improvement of lung function and symptoms … RESCUE • SABA scheduled v prn: Evidence showing increased exposure with scheduled dosing without clear benefit • Comparison: albuterol and ipratropium compared in RCT – both drugs improve lung function similarly Pearls Therapy indicated in more advanced disease (GOLD II‐IV) when SABA alone or combined with a SA antiACH is insufficient to control symptoms. • LABA or LAMA therapy is acceptable choice – • • Choice may be influenced by comorbiditties LAMA often preferred over LABA based on trial evidence suggesting once daily LAMA superior to BID LABA – Tiotropium v salmeterol: tiotropium increased time to first exacerbtion and reduced risk of exacerbation by 17% – Small but significant increases in lung function with tiotropium v salmeterol Indacterol 150mcg or 300mcg or placebo v tiotropium 18 mcg for moderate to severe COPD (n=1683) – Similar benefit and adverse event profiles for each treatment LABA + LAMA increases efficacy • Tiotropium + formoterol v tiotropium only: – Combo therapy had greater improvement in lung function and required less SABA use Volgelmeier,C et al. N Engl J Med 2011;364:1093 Van Noord JA. Eir Res[or K 2005;26:214 Donohue JF et al. Chest 2002;122:47 Combo Bronchodilators Study of 813 patients; % patients demonstrating bronchodilator benefit… •11.2% after ipratropium only •27.4% after albuterol only •34.6% after combination therapy with albuterol and ipratropium Initial lack of response to SA bronchodilator does not predict long term response to treatment with LA bronchodilator Retrospective of 2 RCT of COPD patients (n=921) •Demonstrated improvements in FEV1 after 1 year of treatment with tiotropium regardless of initial responsiveness to bronchodilator Albuterol/ipratropium: Combivent* 75/15 mcg (MDI) 2 INH QID Duoneb* 0.75/.5 (neb) 3mL q6h Donohue JF. et al. Chest. 2004;126(2 suppl):125S–137S. Tashkin D et al. Chest. 2003;123(5);1441-1449. So what do I do? Stick with guidelines and consider patient specific needs. Anticholinergics and beta agonists have similar role. Short acting bronchodilators for persistent or worsening symptoms But… when symptoms progress requiring regular use, long acting bronchodilators are more effective and convenient. Inhaled Steroids Inhaled Corticosteroids (ICS) MOA: anti‐inflammatory effects result from decreased formation, release, and activity of the mediators of inflammation (examples, kinins, histamine, liposomal enzymes, prostaglandins, and leukotrienes) Benefit: Reduce airway inflammation, decrease exacerbations, modestly slow progression of symptoms, … when part of a combined therapy regimen, NOT as single COPD therapy. AE: dose and technique dependent • common: dysphonia, oral thrush • long‐term use in COPD patients unknown in terms of ADE ICS • Beclomethasone: Qvar (MDI) 50‐400 mcg – 1‐2 INH BID • Budesonide: – Pulmicort 100, 200, 400 mcg (DPI): 1‐2 INH BID – Pulmicort Respules 0.5/3mL neb • Fluticasone: – Flovent 44, 110, 220 (MDI): – Flovent Diskus 50, 100, 250mcg (DPI) FDA approved for asthma 4 3/25/2013 LABA/ICS Combos Commonly used in combination for stage III‐IV patients LABA+ICS v LAMA 1323 patients with stable severe COPD (Salmeterol + fluticasone) or tiotropium only x 2 years ICS + LA bronchodilator prevents 1 exacerbation for every 6 patients treated x1 year But Addition of ICS increases risk of pneumonia by 3 extra cases for every 100 patients treated x1 year And ICS (budesonide or fluticasone) increases fracture risk; NNH = 83 x3 years of treatment •No difference in exacerbation rates •More Salmeterol/fluticasone patients needed antibiotics •More tiotropium patients needed oral corticosteroid •Mortality lower in salmeterol/fluticasone group •Patients in salmeterol/fluticasone group with better health status at study end Possibly initiate with LABA if asthmatic component warrants it. LABA/ICS Combos • Fluticasone/salmeterol – cost effectiveness data over placebo or either individually – Advair Diskus (DPI): 1 INH BID • 100/50mcg, 250/50mcg*, 500/50mch – Advair (HFA MDI): 2 INH BID • Budesonide/formoterol: Symbicort (HFA MDI): 2 INH BID – 80/4.5mcg, 160/4.5mcg* • Mometasone/formoterol : Dulera (HFA MDI) : 2 INH BID Refractory disease Sx or repeated exacerbations of COPD despite optimal therapy with LA bronchodilator + ICS (GOLD III‐IV) Be sure to : •Assess for comorbidities contributing to dyspnea •Initiate pulmonary rehab •Assess inhaler technique •Smoking cessation Triple therapy: • Tiotropium and salmeterol and fluticasone Phosphodiesterase 4 Inhibitors MOA: inhibits breakdown of cAMP via PDE‐4 inhibition which in turn reduces inflammation in the respiratory tract •Roflumilast (Daliresp) 500mcg tablet – FDA approved for reduction of exacerbations in patients with COPD associated with chronic bronchitis and history of exacerbations – No dosage adjustment for elderly or renal impairment – Strong 3A4 or dual inhibition with 1A2; increase levels AE: Nausea, reduced appetite, abdominal pain, diarrhea, sleep disturbances, Headache, weight loss Oral Steroids Rarely used for maintenance Reserve for exacerbation treatment Long term systemic treatment has significant side effects. Evidence of increased morbidity and mortality with long term use. IF used for maintenance: • Lowest dose possible • Seek objective measures 5 3/25/2013 Methylxanthines Bronchodilator •Options: Theophylline •MOA: mediated by inhibition of phosphodiesterase III and IV leading to bronchodilation, possible effect on inspiratory muscle •NOT preferred; limited effect and toxicity and multiple DDIs – DDI: 1A2 and 3A4 inhibitors and inducers •Level monitoring: 8‐12 mcg/mL •Low dose theophylline does reduce exacerbations •AE: dose related – Serious: development of atrial and ventricular arrhythmias and grand mal convulsions (may occur without prior medical history) – Common: headache, insomnia, nausea, heartburn Antibiotics Chronic therapy generally not warranted for stable COPD maintenance Anti‐inflammatory effect of antibiotics Erythromycin v placebo bid x1 year Mucolytics Thick secretions can be problematic Carbocysteine: 1500mg daily Other options: Acetylcycsteine, guaifenesin, inhaled hypertonic saline or increased fluid intake •Little evidence supporting their use May improve chest discomfort for some with chronic bronchitis, but… airflow limitations, dyspnea and sputum volume not changed INH Acetylcysteine may produce bronchoconstriction Antitussives • Cough is a protective mechanism! • Regular use of antitussives in stable COPD is NOT recommended. •Fewer exacerbations in erythromycin group Azithromycin v placebo 250mg daily x1yr •Fewer exacerbations in azithromycin •Improved quality of life •Hearing loss associated with azithromycin use Conflicting results from few small studies re: chronic antibiotic use. AE and resistance impact not assessed Vasodilators Not enough evidence to support use in patients with pulmonary hypertension associated with COPD. Narcotics IV or PO opiates can be effective for treatment of dyspnea in COPD patients with very severe disease. 6 3/25/2013 Others Treatment Strategy Not tested; no data •Nedocromil •Leukotriene modifiers •Acupuncture •Homeopathy COPD Combined Assessment … assess risk of No evidence of benefit but some of harm •Anti‐TNF alpha antibody (infliximab) Treatment Strategy Assessing Response • Monitor symptoms GOLD Stage Primary Treatment Alternative All patients: Smoking cessation, vaccines, physical activity, avoidance of risk factors A SAMA prn or SABA prn LAMA or LABA or SABA and SAMA B LAMA or LABA Pulmonary Rehab LAMA and LABA C ICS + LABA or LAMA Pulmonary Rehab LAMA and LABA D ICS + LABA or LAMA Pulmonary Rehab ICS and LAMA or ICS + LABA and LAMA or ICS+LABA and PDE4‐inh. or LAMA and LABA or LAMA and PDE4‐inh. Oxygen therapy Indications: •PaO2 at or below 55mmHg or SaO2 at or below 88% with or without hypercapnea. Confirm twice over 3 week period in stable patient OR •PaO2 at or below 59mmHg or SaO2 at or below 89%, if there is evidence of pulmonary hypertension, heart failure, or polycythemia (Hct>55%) – Dyspnea – Exercise tolerance – Cough – Sputum production • Amount of prn medication use • Frequency of exacerbations Benefits • Long term supplemental oxygen improves survival in patients with COPD and severe resting hypoxemia. • Short term evidence of benefit in patients with more moderate hypoxemia at rest or upon exertion. – Smaller studies with inconsistent criteria Improvement in – Physical activity – Sleep quality – Mental function 7 3/25/2013 Pulmonary Rehabilitation: What is it? Patient Concerns • Embarrassing and bulky oxygen tank • Non‐compliance – Only use for rescue – Only use at night • Using oxygen during the day and night reduces risk of death by half compared to patients only using oxygen at night • Physician prescribed plan of care – Exercise and education – Minimum 6 weeks • Therapist leads sessions – Reconditioning and restoring • Patients set goals – Outcomes documented – Support groups • Fears – “Addicted to oxygen” – Won’t be able to travel Components Pulmonary Rehabilitation Goals: • • • • • Education: – Disease pathology – Stress management – Nutrition – Medications – Pursed lip breathing – What to do if… – Getting good sleep Reduce symptoms Improve quality of life Increase physical participation in life Increase emotional participation in life Assessment • • • • • • 6 minute walk test Stationary bike test Treadmill test Sit to Stand Test Spirometry Borg Scale • Conditioning: – Unsupported arm exercises – Strength – Endurance • Support – Emotional – Social network Evidence of Benefit • • • • • • • • • • • Improved exercise capacity (A) Reduced perceived dyspnea (A) Improved health related quality of life (A) Reduced anxiety and depression associated with COPD (A) Reduces number of hospitalizations and days hospitalized (A) Improved arm function; strength and endurance (B) Improves survival (B) Benefits extend beyond duration of training (B) Improves recovery after exacerbation (B) Enhances effect of LA bronchodilators (B) Respiratory muscle training can be beneficial, especially when combined with general exercise training. (C ) 8 3/25/2013 Not the whole story… Extrapulmonary Manifestations • Weight loss • Muscle dysfunction – Respiratory muscle – Peripheral muscle • Osteoporosis • Cardiovascular diseases • Coronary artery disease • Cerebrovascular disease • Co‐morbidities – Gastroesophageal reflux – Anemia – Depression – Anxiety Lead in for …. –Exacerbations: –Treatment with comorbid conditions 9