LAMA/LABA combination therapy in COPD

ADVERTISEMENT FEATURE
LAMA/LABA combination therapy in COPD
Professor Dave Singh, University of Manchester, Medicines Evaluation Unit,
University Hospital of South Manchester NHS Foundation Trust, Manchester, UK
The prevalence of COPD continues to rise as the global population ages and people continue to engage in behavioural risk factors such as smoking. Some estimates predict that COPD will become the third leading cause of death by 2030.
1 Current treatments aim to improve lung function, mitigate symptoms and reduce frequency and severity of exacerbations.
2 Bronchodilators are the main pharmacological intervention for stable COPD, with long-acting bronchodilators prescribed for the prevention and reduction of symptoms.
2 There are two classes of long-acting bronchodilators used in the treatment of COPD: long-acting muscarinic antagonists (LAMAs) and longacting ß2-adrenergic agonists (LABAs). LAMAs inhibit the action of acetylcholine at muscarinic receptors, while LABAs enhance cAMP signalling through stimulation of
ß2-adrenergic receptors.
2 Additionally, inhaled corticosteroids (ICSs) are anti-inflammatory drugs that are used in patients with a history of acute exacerbations in order to prevent future exacerbations.
Pharmacological management of COPD
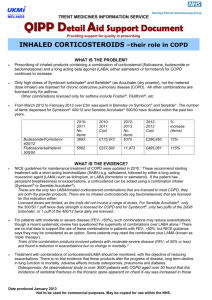
Today, ICS therapy is recommended only as a combination treatment with a LABA, based on a patient’s risk of exacerbation.
2,3 Long-term ICS treatment is associated with multiple adverse effects including skin bruising, 4,5 steroid myopathy, 6 fractures, mouth infections and pneumonia; 7,8 their benefit in patients at low risk of exacerbations is therefore questionable.
Despite this, a substantial proportion of patients with COPD receive inappropriate prescriptions for ICS as an initial treatment, in contradiction of current clinical guidelines.
9
For patients at low risk of exacerbations, long-acting bronchodilators should be the treatments of choice. Owing to the distinct but complementary mechanisms of action of LAMA and LABA treatments, it has been shown that concomitant LAMA and LABA treatment is more effective at improving bronchodilation than increasing the dose of
LABA alone; 10 this approach also reduces the risk of additional dose-dependent, classassociated adverse effects. Medication compliance in patients with COPD decreases as the number of administrations required per day increases, 11 therefore delivery of a LAMA and a LABA in a single inhaler (LAMA/LABA combination therapy) represents a desirable approach to treatment. Multiple studies have demonstrated the additive improvements in lung function of LAMA/LABA combination therapy in a single inhaler compared with their constituent monocomponents.
12-16
LAMA/LABA combination therapy: meeting the recommendations of clinical guidelines
LAMA/LABA combination therapy occupies limited space in the current COPD treatment guidelines from the National Institute of Health and Care Excellence (NICE), 3 where it is restricted to a small cohort of patients who cannot tolerate ICS treatment.
These have served as the main clinical guidelines for physicians in England, Wales and
Northern Ireland; however, they were published in 2010 ahead of several clinical trials demonstrating the efficacy of the newer LAMAs and LAMA/LABA combinations and their approval in Europe. In Scotland, however, the Respiratory Prescribing Strategy issued by NHS Scotland 17 highlights the need for the revision of the NICE guidelines, and instead adopts treatment procedures from the current Global Initiative for Chronic
Obstructive Lung Disease (GOLD) strategy.
It has been known for some time that the main criterion used to diagnose COPD, airflow limitation, correlates only weakly with respiratory symptoms and health-related quality of life in patients with COPD; therefore, the GOLD strategy document has adopted a new approach to account for symptoms and risk of exacerbations.
2 GOLD treatment options, indicated by GOLD group, based on more/less symptoms and higher/lower risk of exacerbations, are shown in the table.
LAMA/LABA combination treatment options
There are currently three LAMA/LABA combination treatments approved by the European
Medicines Agency:
Ultibro ®
(indacaterol/ glycopyrronium,
Novartis)
Anoro ®
(umeclidinium bromide/vilanterol,
GlaxoSmithKline)
Duaklir ® (aclidinium bromide/formoterol fumarate dihydrate,
AstraZeneca)
All three LAMA/LABA combinations improve indices of lung function compared with placebo and their constituent monotherapies.
12,14,16,18,19
Ultibro ® improves dyspnoea compared with placebo and tiotropium 20 in patients with stable COPD. Ultibro ® and Anoro ® have not consistently demonstrated improvements in dyspnoea (as measured by the mean Transitional Dyspnoea
Index [TDI] score) or health status, compared with their monocomponents.
12,18,19
However, the overall pattern of reduction in rescue medication use with
LAMA/LABA combinations compared with monocomponent therapy suggests a benefit in symptom control.
12,18,19 Additionally, there is evidence that Ultibro ® reduces the rate of COPD exacerbations compared with LAMA monotherapy in patients with forced expiratory volume in 1 second <50% who have a history of exacerbations.
21
In addition to improving bronchodilation, Duaklir ® statistically significantly improves health-related quality of life (measured by St George’s Respiratory
Questionnaire, SGRQ) in the AUGMENT trial 16 and dyspnoea (measured by
TDI) in the AUGMENT and ACLIFORM trials.
14,16 Differences with Duaklir ® compared with placebo exceeded the minimal clinically important differences of ≥4 units for the SGRQ 16 and ≥1 unit for the TDI; 14,16 differences between
Duaklir ® and monotherapies were not significant in the individual trials.
14,16
Importantly, from the perspective of the patient, Duaklir ® significantly reduces total daily symptom scores measured using the EXACT-Respiratory Symptoms questionnaire compared with its constituent monotherapies; furthermore, both nocturnal and early morning symptoms are reduced with Duaklir ® .
14,16
Aclidinium bromide is rapidly hydrolysed in human serum with a low capacity for systemic exposure, 22 and has been demonstrated to be suitable for use in patients with COPD and concomitant renal insufficiency without the need for additional monitoring.
23 Duaklir ® consequently has low potential to cause the side effects typical of antimuscarinics, 22 and may be suitable for use in patients with renal comorbidities.
Delivery devices for LAMA/LABA combination therapy
T
he role of the delivery device is also crucial in providing efficacious treatment of
COPD.
24 Incorrect use is common with respiratory inhalers and reduces the efficacy of the drug; 25 complicated administration procedures can further reduce patient compliance. Each LAMA/LABA combination is administered via a dry powder inhaler (DPI). Ultibro ® and Anoro ® are administered once daily via Breezhaler ®
(Novartis) and Ellipta ® (GlaxoSmithKline), respectively. Duaklir ® is administered twice daily via Genuair ® (AstraZeneca); patients reported greater satisfaction with
Genuair ® than with HandiHaler ® (Boehringer-Ingelheim).
26 The three LAMA/LABA combination DPIs are breath-actuated (reducing the need to coordinate breath and hand actions) and include visual and aural feedback to indicate correct usage.
Additionally, Genuair ® and Ellipta ® are multi-dose DPIs, eliminating the need to reload capsule doses which can be difficult to manipulate, particularly for patients with poor dexterity.
AZ_404327_IP_ADVERTORIAL_295x450_DPS_V2.indd 1 29/01/2015 09:22
ADVERTISEMENT FEATURE
Conclusion
The pool of clinical evidence for the superiority of dual bronchodilator therapy above monotherapy is increasing. LAMA/LABA combination has been shown to improve bronchodilation over either monocomponent alone, and there is evidence that this is associated with better symptom control. For patients with low risk of exacerbations, a LAMA/LABA combination is preferable to an ICS/LABA treatment.
27
There are now three LAMA/LABA combinations available in the UK so physicians can select the most suitable COPD treatment for their patient.
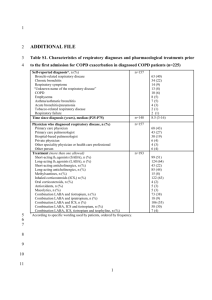
GOLD groups and treatment choices
PATIENT
GROUP
RISK OF
EXACERBATIONS
SYMPTOMS FIRST CHOICE ALTERNATIVE CHOICE
A Low Few SAMA prn or SABA prn LAMA or LABA or SAMA+SABA
B Low More LAMA or LABA
LABA+LAMA
C
D
High
High
Few
More
ICS+LABA or LAMA
ICS+LABA and/or LAMA
LABA+LAMA or LAMA+PDE4-i
or LABA+PDE4-i
ICS+LAMA+LABA or ICS+LABA+PDE4-i
or LABA+LAMA or LAMA+PDE4-i
ICS, inhaled corticosteroid; LABA, long-acting ß2-agonist; LAMA, long-acting muscarinic antagonist; PDE4-i, phosphodiesterase-4 inhibitor; prn, as needed; SABA, short-acting
ß2-agonist; SAMA, short-acting muscarinic antagonist.
PRESCRIBING INFORMATION
(Please consult the Summary of Product Characteristics (SmPC) before prescribing.)
DUAKLIR ® GENUAIR ®
340 micrograms /12 micrograms inhalation powder aclidinium and formoterol fumarate dihydrate
Presentation: Each delivered dose (the dose leaving the mouthpiece) contains 396 micrograms of aclidinium bromide
(equivalent to 340 micrograms of aclidinium) and 11.8 micrograms of formoterol fumarate dihydrate. Each delivered dose contains approximately 11 mg lactose (as monohydrate).
Indication: Duaklir Genuair is indicated as a maintenance bronchodilator treatment to relieve symptoms in adult patients with chronic obstructive pulmonary disease (COPD). Dosage and Administration: The recommended dose is one inhalation of Duaklir Genuair 340 micrograms /12 micrograms twice daily. Consult SmPC and package leaflet for method of administration. Contraindications, Warnings, Precautions:
Contraindications: Hypersensitivity to the active substances or to the excipient lactose monohydrate. Precautions: Should not be used to treat asthma or for treatment of acute episodes of bronchospasm, i.e. rescue therapy. In clinical studies, paradoxical bronchospasm was not observed at recommended doses.
Paradoxical bronchospasm has been observed with other inhalation therapies. If this occurs, stop medicine and consider other treatment. Use with caution in patients with a myocardial infarction during the previous 6 months, unstable angina, newly diagnosed arrhythmia within the previous 3 months, QTc above
470 msec or hospitalisation within the previous 12 months for heart failure functional classes III and IV as per the “New York
Heart Association”. ß
2
-adrenergic agonists such as formoterol fumarate dihydrate may produce increases in pulse rate and blood pressure, electrocardiogram (ECG) changes such as T wave flattening, ST segment depression and prolongation of the QTcinterval in some patients. If effects occur, treatment may need to be discontinued. Use with caution in patients with severe cardiovascular disorders, convulsive disorders, thyrotoxicosis and phaeochromocytoma. Metabolic effects of hyperglycaemia and hypokalaemia may be observed with high doses of ß
2
-adrenergic agonists. Consistent with its anticholinergic activity, use with caution in patients with symptomatic prostatic hyperplasia or bladder-neck obstruction or with narrow-angle glaucoma.
Dry mouth has been observed and may in the long term be associated with dental caries. Patients with rare hereditary problems of galactose intolerance, Lapp lactase deficiency or glucose-galactose malabsorption should not take this medicine.
Interactions: Co-administration with other anticholinergic and/or
ß
2
-adrenergic agonist containing medicines has not been studied and is not recommended. Although no formal in vivo drug interaction studies have been performed with Duaklir Genuair, it has been used concomitantly with other COPD medicinal products including short-acting ß
2
-adrenergic bronchodilators, methylxanthines, and oral and inhaled steroids without clinical evidence of drug interactions. Caution is advised in concomitant treatment with methylxanthine derivatives, steroids, or nonpotassium-sparing diuretics as this may potentiate the possible hypokalaemic effect of ß
2
-adrenergic agonists. ß-adrenergic blockers may weaken or antagonise the effect of ß
2
-adrenergic agonists. If ß-adrenergic blockers are required (including eye drops), cardioselective beta-adrenergic blockers are preferred, and these should be administered with caution. The action of formoterol on the cardiovascular system may be potentiated with medicinal products known to prolong the QTc interval such as monoamine oxidase inhibitors, tricyclic antidepressants, antihistamines or macrolides. Such medicines that prolong QTc interval are known to increase the risk of ventricular arrhythmias and should be administered with caution.
Fertility Pregnancy and lactation: It is considered unlikely that Duaklir Genuair administered at the recommended dose will affect fertility in humans. Duaklir Genuair should only be used during pregnancy if the expected benefits to the mother outweigh the potential risks to the infant. It is unknown whether aclidinium bromide
(and/or its metabolites) or formoterol are excreted in human milk.
The benefit for the breast-feeding child and long-term benefit of therapy for the mother should be considered when making a decision whether to discontinue therapy. Ability to drive and use machines: The effects on the ability to drive and use machines are negligible. The occurrence of headache or blurred vision may influence the ability to drive or use machinery. Adverse Reactions:
Common: Nasopharyngitis, urinary tract infection, sinusitis, tooth abscess, insomnia, anxiety, headache, dizziness, tremor, cough, diarrhoea, nausea, dry mouth, myalgia, muscle spasm, peripheral oedema, blood creatine phosphokinase increased.
Uncommon:
Hypokalaemia, hyperglycaemia, agitation, dysgeusia, blurred vision, tachycardia, ECG QTc prolonged palpitations, dysphonia, throat irritation, rash, pruritus, urinary retention, blood pressure increased.
Rare: Hypersensitivity, bronchospasm including paradoxical. Legal Category: POM.
Marketing Authorisation
Number(s): EU/1/14/964/001 - Carton containing 1 inhaler with
60 unit doses.
NHS Cost: £32.50 (excluding VAT).
Marketing
Authorisation Holder: Almirall S.A. Ronda General Mitre, 151,
08022 Barcelona, Spain. Further information is available from:
AstraZeneca UK Ltd. 600 Capability Green Luton LU1 3LU, UK.
Tel: 0800 783 0033 / 01582 836836 Fax: +44 (0)1582 838 003
Email: Medical.informationuk@astrazeneca.com
Date of Revision: 12/2014. RSP 14 0096 Duaklir and Genuair are both registered trademarks.
Adverse events should be reported. Reporting forms and information can be found at www.
mhra.gov.uk/yellowcard. Adverse events should also be reported to AstraZeneca on 0800 783 0333
References: 1 . World Health Organization. 2012. Available at: http://www.who.int/respiratory/copd/en/index.html.
2 . Global Initiative for Chronic Obstructive Lung Disease.
2014. Available at: http://www.goldcopd.com/guidelinesglobal-strategy-for-diagnosis-management.html. 3 . National
Clinical Guideline Centre. 2010. Available at: http://guidance.
nice.org.uk/CG101/Guidance/pdf/English. 4 . Burge PS et al .
BMJ 2000; 320: 1297-1303. 5 . Pauwels RA et al . N Engl
J Med 1999; 340: 1948-1953. 6 . Levin OS et al . J Neurol
Sci 2014; 338: 96-101. 7 . Mattishent K et al . Drugs 2014;
74: 539-547. 8 . Yang IA et al . Cochrane Database Syst Rev
2012; 7: CD002991. 9 . Price D et al . Int J Chron Obstruct
Pulmon Dis 2014; 9: 889-904. 10 . van Noord JA et al .
Thorax 2010; 65: 1086-1091. 11 . Toy EL et al . Respir Med
2011; 105: 435-441. 12 . Bateman ED et al . Eur Respir J
2013; 42: 1484-1494. 13 . Celli B et al . Chest 2014; 145:
981-991. 14 . Singh D et al . BMC Pulm Med 2014; 14: 178.
15 . ZuWallack R et al . Int J Chron Obstruct Pulmon Dis 2014;
9: 1133-1144. 16 . D’Urzo AD et al . Respir Res 2014; 15: 123.
17 . NHS Scotland. 2014. Available at: http://www.sehd.scot.
nhs.uk/cmo/CMO(2014)14-Respiratory%20Prescribing%20
Strategy%20June%202014.pdf. 18 . Decramer M et al .
Lancet Respir Med 2014. 19 . Donohue JF et al . Respir Med
2013; 107: 1538-1546. 20 . Mahler DA et al . Eur Respir J
2014; 43: 1599-1609. 21 . Wedzicha JA et al . Lancet Respir
Med 2013; 1: 199-209. 22 . Sentellas S et al . Eur J Pharm Sci
2010; 39: 283-290. 23 . Schmid K et al . Clin Ther 2010; 32:
1798-1812. 24 . Sanduzzi A et al . Multidiscip Respir Med
2014; 9: 60. 25 . Chorao P et al . Respir Med 2014; 108:
968-975. 26 . van der Palen J et al . Expert Opin Drug Deliv
2013; 10: 1023-1031. 27 . Vogelmeier C et al . Lancet Respir
Med 2013; 1: 51-60.
Date of preparation: January 2015
Job code: GL/ABF/0115/0185a
AZ_404327_IP_ADVERTORIAL_295x450_DPS_V2.indd 2 29/01/2015 09:22